Playlist
Show Playlist
Hide Playlist
Lupus Nephritis – Nephritic Syndrome
-
Slides Nephritic Syndrome.pdf
-
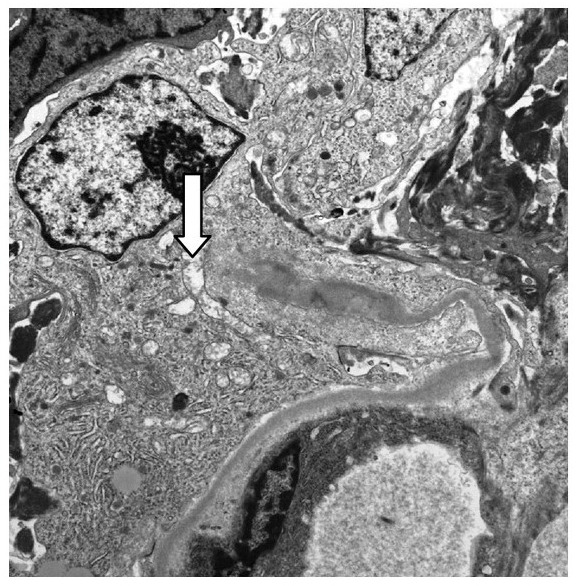
Download Lecture Overview
00:01 So, lupus nephritis occurs in about 50% of patients who have systemic lupus erythematosis. 00:07 So, not all patients diagnosed with SLE, systemic lupus erythematosis, are going to get lupus nephritis but about 50% of them will. 00:16 It's a frequent cause, when they do get nephritis, of morbidity and mortality in that patient population. 00:22 And there's an increase in incidence in females, Hispanic or Latino population, as well as African American populations. 00:30 When we think about the etiology of lupus nephritis, it's really multifactorial. 00:35 Those are genetic predisposition so we can see an increase in concordance rate in monozygotic twins. 00:40 It's polygenic, meaning that multiple genes are involved. There's environmental factors. 00:46 There's a higher prevalence in lower socioeconomic settings and there's probably viral antigens that are involved as well. 00:53 And there's an immune component as well. Remember, patients have a loss of tolerance. 00:57 They have a tendency towards autoimmunity and polyclonal B cell activation. 01:02 So, it's an autoimmune disease. 01:04 So, when we think about the pathogenesis, there are antibodies that are produced against self-antigens. 01:11 Patients are recognizing self as foreign. The antibody target are actually nucleosomes. 01:16 Those are the nephritic antigens. So, when cells undergo apoptosis and necrosis, what happens is they fail to clear from the circulation, they spill their contents into the circulation so now that is recognized as foreign, and the immune system becomes exposed to those intracellular contents directing antibodies against them. 01:36 So, thinking about the pathogenesis of this disease, again, we have antibodies that are directed at the nucleosomes, forming immune complexes. 01:43 There's a couple of different ways that they can deposit in the kidney. 01:46 The first way is that we can have an anti-nucleosome antibody that's going to cross-react with an intrinsic renal antigen and then bind that antigen directly. 01:57 It could be that an anti-nucleosome antibody will bind to that soluble nucleosome that's in the circulation and antigenic, and then that circulates as an immune complex and that immune complex will passively trap or deposit in they kidney. 02:13 And the third way is that the nucleosome antigen will deposit first and implant in the kidney, and then an antibody will then secondarily recognize it, bind to that, form an immune complex insitu, complement, of course, is activated. 02:29 So, when we think about diagnosing our patients with lupus, there's a couple of things that can really help us within our armamentarium. 02:36 Number one, when we're looking at blood values, we can look at lupus serologies in particular. 02:41 These are things like the anti-nuclear antibody. 02:43 That's exactly what we're looking for, that anti double-stranded DNA which is a little bit more specific for the nucleosome. 02:50 It can tell us, that titer can tell us about disease activity in our patients. 02:55 Patients who have active lupus nephritis will have low serum complements. 03:00 Remember, we talked about what's happening here. 03:02 This is antigen antibody stimulating classical pathway of complement activation so we will see both a low C3 and a low C4 complement, and low total complement in the serum. These patients have active urine sediment, probably on the order of excitement in terms of infection-related GN. 03:20 There's a lot of red blood cells in here, dysmorphic in features and plenty of red blood cell cast to see in that particular sediment. 03:26 Now, I do want to mention membranous lupus nephritis. 03:31 So, we'll talk about that in just a moment but membranous lupus nephritis is much like membranous nephropathy. 03:37 Sometimes patients can manifest just with nephrotic syndrome due to a membranous in association with their lupus nephritis. 03:44 And when that happens, they could have normal serum complements and they may have minimal serological abnormalities including their double-stranded DNA and ANA. 03:53 So, do keep that in mind but there's some helpful clues that could really help us ultimately make the right diagnosis in that patient population. 04:02 And of course, as always, for most of my glomerular diseases, if we really wanna clinch the diagnosis, a renal biopsy is imperative. 04:10 Now, before we're going on to that looking at our pathology, let's take a moment to talk about the classification of lupus. 04:16 So, in 2003, the International Society of Nephrology and the Renal Pathology Society reclassified lupus based on Classes I through VI. 04:24 All you need to be responsible for from a clinical standpoint and taking care of these patients as well as your boards is understanding what Class III, IV, and V lupus nephritis means. 04:34 Class III lupus nephritis is what we refer to as focal proliferative. 04:40 What that means is that less than 50% of glomeruli are involved with a proliferative lupus nephritis. 04:47 So, we have endothelial cell proliferation in addition to mesangial cell proliferation and we also have subendothelial deposits. Class IV is diffused proliferative. 04:57 So, that simply means that instead of less than 50%, we've got more than 50% of the glomeruli involved with this particular disease process. 05:06 Again, proliferative. We've got endothelial cell proliferation, mesangial cell proliferation, subendothelial deposit immune complex. 05:13 Class V is our membranous form of lupus nephritis and so, patients manifest more with a membranous type of histology with subepithelial deposits and nephrotic syndrome. 05:25 Now, interestingly, in order to differentiate between membranous lupus and primary membranous nephropathy, membranous lupus are always going to have some mesangial deposits and mesangial hypercellularity. 05:39 So, when we think about the pathology for lupus nephritis, what's shown here is somebody who has diffused proliferative lupus nephritis. 05:48 This is an H and E stain and what I want you to appreciate are the capillary loops. 05:54 Instead of having beautiful, delicate, thin capillary loops, these are big, chunky capillary loops. 06:00 They are also referred to as wire loops and the reason why they're so chunky is because those are filled with subendothelial immune complexes. 06:09 So, again, when we see that, those wire loops, those big subendothelial immune complexes that are big and chunky, taking up that capillary loop wall, we really have to think about lupus. 06:20 I also want you to remember the name wire loops because that might be a buzz word that's important for you for your step. 06:27 On electron microscopy, we can see just about everything. 06:30 These patients will have mesangial immune deposits, they will have subendothelial immune deposits, and they can also have some subepithelial immune deposits. 06:39 So, we tend to see just about everything on our EM. 06:43 Our immunofluorescence is also important. 06:45 We can see pretty much all of our heavy chains. 06:49 So, we have IgG, IgA, IgM, that are all positive, and then we also have C3 and C1q, and that's why we also call this full house. 07:01 So, if anybody plays poker, they'll understand that a full house is 3 of a kind and 2 of a kind. 07:05 What that refers to is that 3 heavy chains, IgG, IgA, and IgM, and our complements, C1q and C3. 07:13 That's also a buzz word that I do want you to keep in mind cuz that will probably come up for your USMLE. 07:20 Okay, in terms of their clinical presentation, it's really variable. 07:26 It depends on the pattern of injury. 07:29 Okay? So, some patients, if they have, let's say, a Class IV and a Class V, meaning that they have the membranous component and they have that proliferative component. 07:39 They can have both nephrotic and nephritic syndrome. 07:42 But ultimately, when you diagnose and take care of these patients, they tend to have a more relapsing and remitting disease course. 07:51 So, over time, they have exacerbations, they go into remission, and then they will have these exacerbations again with their lupus nephritis. 08:00 So, in terms of treatment, it's going to really depend on their clinical presentation in the class of lupus nephritis on biopsy. 08:07 So, again, if I have a patient sitting in front of me with lupus, I absolutely need a biopsy and I need my pathologist by my side for us to really make the correct clinical interpretation of what's going on and prognosticate, and figure out how we wanna best treat this patient. 08:23 So, if we are thinking about treatment, it's really going to include those patients who have Class III through V. 08:30 Those are the ones that have risks for renal progression and loss of function. 08:34 So, they have to be treated aggressively. 08:36 So, treatment are going to be patients, again, who have active lesions. 08:40 Again, Class III through V and that's gonna include cyclophosphamide, an alkylating agent, or mycophenolate mofetil which is an antimetabolite, trade name is called CellCept, and then we do that along with glucocorticoids which are steroids. 08:54 We use that in induction-type regimen so we're using higher doses for a 6-month period of time to induce a remission. 09:02 We then use maintenance therapy with the same agents typically. 09:07 So, if we're using cyclophosphamide to begin with, we will switch to mycophenolate mofetil or azathioprine, another antimetabolite, to maintain that remission along with a low-dose steroid. 09:18 Alternative agents include rituximab, that's our anti-CD 20 monoclonal antibody. 09:23 Now, used with just lupus alone or using that particular agent in somebody for an induction regimen may not be as beneficial but it's something that we have in our back pocket for people who have resistant lupus nephritis. 09:38 We also have multitargeted therapy. 09:40 So, there's some patient populations, particularly Eastern Asian populations, that may do better with things like a calcineurin inhibitor in addition to the mycophenolate mofetil and steroids. 09:53 So, again, these are alternative agents that if our patients fail either cyclophosphamide alone or mycophenolate mofetil or induction therapy, we can move to these alternative agents to see if they can help our patient. 10:05 There's plenty of new therapies that are on the horizon. 10:07 Alemtuzumab, which is another CD 20 antibody, is right there on the cusp of potentially being a newer therapy for these patients. 10:15 So, stay tuned because they do believe that there's exciting things for lupus nephritis coming down the pipeline.
About the Lecture
The lecture Lupus Nephritis – Nephritic Syndrome by Amy Sussman, MD is from the course Nephritic Syndrome.
Included Quiz Questions
Which of the following is involved in the pathogenesis of lupus nephritis?
- Autoantibodies against nucleosomes
- Inappropriate activation of the alternative complement pathway
- Autoantibodies to type IV collagen in the glomerular basement membrane
- Persistent HCV antigenemia
- Autoantibodies that stabilize C3 convertase
Which of the following is associated with lupus nephritis?
- Anti-dsDNA antibodies
- Normal C3 and C4 complement levels
- Decreased AH50
- Bland urinary sediments
- Anti–cyclic citrullinated peptide (CCP) antibodies
Which of the following differentiates membranous lupus nephritis from classical membranous nephropathy?
- Mesangial hypercellularity on renal biopsy
- Low C3, C4, and total CH50 complement levels
- Active urinary sediment with RBC casts
- Abnormal serologic testing results
A renal biopsy of a patient with SLE shows inflammatory injury involving >50% of glomeruli. What is the classification of this patient's lupus nephritis?
- Class IV, diffuse lupus nephritis
- Class II, mesangial proliferative lupus nephritis
- Class III, focal lupus nephritis
- Class V, membranous lupus nephritis
- Class VI, advanced sclerosis lupus nephritis
Which of the following is true regarding the management of lupus nephritis?
- Induction therapy should consist of glucocorticoids combined with either cyclophosphamide or mycophenolate mofetil.
- Aggressive immunosuppressive therapy is indicated in patients with lupus nephritis class IV, V, or VI.
- Induction therapy for lupus nephritis consists of glucocorticoid monotherapy.
- Mycophenolate mofetil, which is an anti-CD20 antibody, is the preferred choice for maintenance therapy.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |