Playlist
Show Playlist
Hide Playlist
Irritable Bowel Syndrome
-
Slides GIP Irritable Bowel Syndrome.pdf
-
Download Lecture Overview
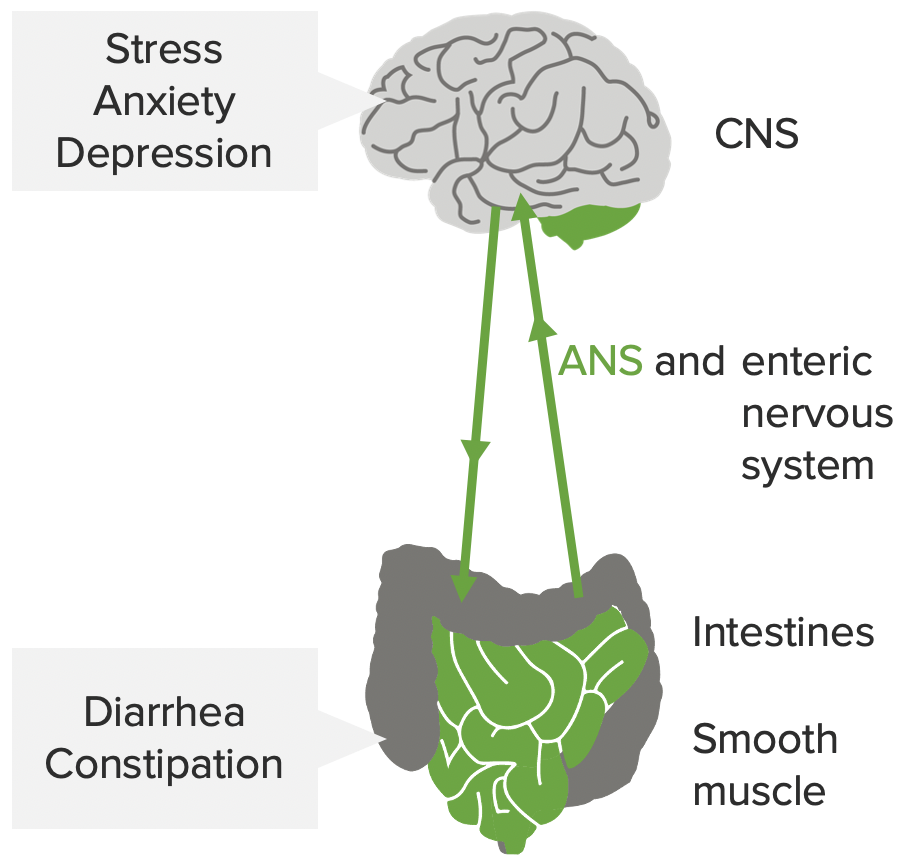
00:01 All right. Welcome to the world of Irritable Bowel Syndrome. 00:05 This is IBS. This should be not confused with inflammatory bowel disease which is IBD. 00:13 IBS or irritable bowel syndrome is a functional bowel disease. There's really not identifiable pathologic changes that we can recognize. 00:22 And it's characterized by chronic abdominal pain and altered bowel motility. And there's no identifiable organic cause. 00:30 Doesn't mean it doesn't exist and it doesn't mean it's only in your head. 00:34 This is a real entity and you will have patients who will suffer from this. Let's look at the epidemiology. 00:41 So, the onset is typically younger individuals who will tend to have this - it may or may not be related to the stressors of young adult life. 00:50 We'll talk more about stress in a minute. Overall, the most common patient is going to be a woman. 00:57 So, somewhere between two-thirds and three-quarters of patients with irritable bowel syndrome are female. 01:04 In North America, there's a relatively high prevalence of about 10% to 15% of the population total. 01:13 And in most of the developed nations of the world, there is a similar prevalence. 01:19 In the developing parts of the world, we don't have a firm handle on prevalence. 01:25 And in fact, infectious causes of bowel symptoms are much, much, much more common. 01:34 The pathophysiology. We don't have an organic cause but we do know that there is abnormal bowel motility. 01:41 So, what is being shown on the little column on the left is food moving along the tubular bowel in a nice, uniform top to bottom fashion and there's a relatively common speed by which things transit throughout the bowel. 01:55 In irritable bowel syndrome, you may either have faster or slower, or even waves of peristalsis that go backwards. 02:06 So, it's an abnormal frequency and irregularity of contractions. There is also an increased sensitivity to cholecystokinin. 02:15 So, these are - this is a polypeptide hormone that is secreted at the time of food entering the stomach. 02:23 And that will drive the normal peristaltic wave. It will be part of the mechanism by which peristalsis is allowed to proceed. 02:31 We do know that in irritable bowel syndrome, the tubular gut is much more sensitive to the cholecystokinin. 02:42 Because of the abnormal bowel motility, frequently with a higher frequency and faster transit time, there's typically diarrhea. 02:50 But in some cases, you may have irritable bowel syndrome with constipation, so called IBS-C Intestinal inflammation may underline this. In fact, I'm going to show you some possibilities. 03:06 These are heavily debated. We don't know why this happens. 03:11 But you may have in some individuals slightly more lymphocytes within their lamina propria and/or mast cells and these would release mediators that will increase the bowel motility. 03:25 This may happen after infections and we may have increased serotonin levels which also modulate bowel motility. 03:32 What we have are patients who have increased sensitivity to pain which may be associated with increased receptor stimulation but they also, well, pound for pound or cubic centimeter per cubic centimeter of gas, these patients will feel distension of the bowel much more acutely than those without irritable bowel syndrome. 03:59 There is clearly a psychosocial element of IBS. Greater than 50% of patients have depression and/or anxiety. 04:09 Now, it's not clear whether the depression and anxiety are causing IBS or patients have this because they have IBS and sorting that out may be very difficult. But in the setting of IBS, any increased stress may drive increased corticotrophin-releasing factor activity giving rise to increased glucocorticoids which may stimulate increased sensitivity to abdominal pain and may alter bowel motility. 04:38 The clinical presentation. So, depending on whether you just have irritable bowel syndrome or if you have it with constipation, you may or may not have diarrhea but you will always have abdominal pain and you will have an increased sensitivity to bowel distension. With diarrhea, you'll have lose and watery stools. 04:58 There should not be blood in those stools because you're not causing any epithelial damage. 05:04 With the diarrhea, clearly increased bowel movements. And there may be real urgency that occasionally may lead to incontinence. 05:13 The IBS with constipation may give rise to very hard stools, infrequent bowel movements because we're not moving with the same transit time through the GI tract and may require straining with defecation. 05:28 Making the diagnosis, it's a clinical history. It's pain that occurs classically a day per week for the previous three months. 05:37 So, that's the clinical definition. And so, all you have to do is ask a patient, how often are you having pain, maybe what other symptoms you're having with it, and for how long have you had that? If they gave you a day per week for three months, that is the clinical criteria. 05:53 The physical exam is not very helpful. There may be a little bit of abdominal distension, some tenderness but it's very hard to find anything on a physical exam and notably, there's not going to be borborygmi. You will have normal bowel sounds. 06:07 The laboratory tests are really more exclusionary. We want to rule out other causes of the diarrhea or the constipation. 06:17 So, people with irritable bowel syndrome should not have an anemia because there was no bleeding and they have normal absorption. 06:24 So, the CBC should be fine. Calprotectin is actually a biomarker that allows us to see whether there is inflammation we detect it in the stool. 06:35 And if that is elevated, then, we would implicate things like inflammatory bowel disease, not irritable bowel syndrome. 06:44 We want to make sure that there's no infection. We'll do stool cultures, ovas and parasites and we will certainly want to look to make sure that there is no elevated thyroid hormone activity because clearly, thyrotoxicosis or hyperthyroidism can cause increased abdominal or bowel transit. 07:04 Abdominal radiograph, usually, not all that helpful. You may see focal areas of spasm but you may or may not capture that at any particular time that a patient comes in. 07:15 And the colonoscopy with biopsy, it's just to rule out other things. 07:18 There's nothing to be seen by the pathologist in the setting of irritable bowel syndrome. 07:25 How do we manage it? So, you can do some dietary modifications and many cases, it's felt that this is more of a psychological benefit rather than a true change in how the bowel is behaving. 07:36 But eating more fiber for example, is felt to give a better sort of bowel transit. 07:44 And certainly with increased fiber, you, for a patient who has constipation, that may improve their symptoms. 07:51 Pharmacologic agents may be helpful. So antidiarrheal agents, things that will cause increased fluid retention within the bowel. 08:00 Things that cause or will help with spasm. You may try probiotics just to see if the bowel microflora is somehow responsible and helping the patient with their psychological issues, helping them to develop a more Zen-like approach to life may be helpful. 08:20 With that, irritable bowel syndrome and how to look at it.
About the Lecture
The lecture Irritable Bowel Syndrome by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is irritable bowel syndrome?
- Functional bowel disease causing chronic abdominal pain and altered bowel motility without identifiable organic cause
- Functional bowel disease causing acute abdominal pain without identifiable organic cause
- Functional bowel disease causing acute abdominal pain with multiple identifiable organic causes
- Subtype of Crohn disease
- Subtype of ulcerative colitis
What is the typical age of onset of irritable bowel syndrome?
- 20–40 years old
- 30–50 years old
- 40–60 years old
- 10–30 years old
- 10–50 years old
Which of the following describes the pathophysiology of irritable bowel syndrome?
- Abnormal motility
- Caseating granulomas
- Non-caseating granulomas
- Increased Th2 cell population
- Epithelial erosion and ulceration
Which of the following symptoms is NOT consistent with irritable bowel syndrome?
- Bloody diarrhea with mucus
- Loose and watery stools
- Abdominal pain
- Frequent bowel movements
- Bowel urgency
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very well and clearly explained and nice to listen to.