Playlist
Show Playlist
Hide Playlist
Intussusception in Children
-
Slides Intussusception Pediatrics.pdf
-
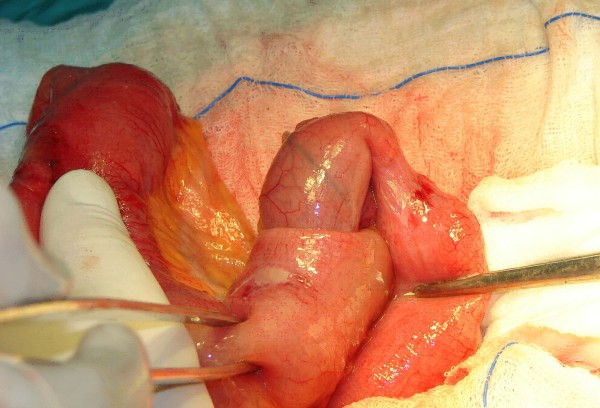
Download Lecture Overview
00:02 In this lecture, we’re going to discuss intussusception. 00:07 Intussusception is a prolapse of proximal portion of intestine into a distal portion of intestine. 00:14 Perhaps, the easiest way to see it is on the right side of this slide where you can see the proximal intestine invaginating into the distal intestine. 00:26 It’s sometimes hard to describe this to families and patients, and the way I will sometimes describe it is if we have a balloon animal -- balloon, you know those long balloons that we make balloon animals out of -- and I push my finger into the balloon animal and I can see my finger, that’s often how it happens. 00:44 It starts really on this side of the intestine and pushes it in, and it’s from a lead point, something abnormal in the side of the intestine that’s causing that piece of intestine to invaginate. 00:58 Intussusception is mostly a pediatric problem. 01:02 It’s most common abdominal emergency in children in the two years of age range. 01:10 It usually happens between three months and six years of age. 01:15 And the peak incidence is around six months to twelve months. 01:20 The majority of cases are idiopathic. 01:23 We can’t figure out what was the problem that cause this to happen. 01:28 There was no obvious lead point. 01:30 Although we suspect that the lead point is almost invariably a Peyer's patch. 01:36 Remember, the Peyer's patch is that area of lymphoidal tissue in the ileum in children where they have a larger amount of lymphoidal tissue. 01:46 These Peyer’s patches can be slightly inflamed or enlarged and could be the lead point for an intussusception. 01:53 And because these Peyer’s patches are mostly in the ileum, most intussusception is ileocecal. 02:01 In other words, it comes from the ileum and goes in through the cecum and into the large intestine. 02:08 Patients who have intussusception will have a classic triad of symptoms. 02:15 So, the classic triad is intermittent colicky abdominal pain, vomiting, and bloody stools. 02:25 Now, this is what you’ll see written on your test, and you should definitely remember this. 02:31 The reality as though is that most intussusception, we do not actually find bloody stools. 02:37 It’s a rare finding when the diagnosis has been missed for a long period of time. 02:45 The other thing that’s key to discuss with any patient who’s presenting with intussusception is a remarkable altered mental status. 02:55 Children with intussusception, for reasons we do not understand, can have such altered mental status. 03:00 They can literally be unarousable. 03:03 And this mental status will wax and wane between severe somnolence and severe irritation and abdominal pain. 03:12 These children may have a sort of cyclical severe irritability followed by excessive somnolence. 03:19 In the differential diagnosis, for an unresponsive child, it’s intussusception. 03:27 Complications from intussusception generally happen if a patient has a delay in diagnosis. 03:34 In this picture of this little boy here with intussusception, this is a remarkable photo because you can actually see the right upper quadrant mass that is his intussusception. 03:46 This child is severely ill, likely because of a delay in diagnosis. 03:51 Delay in diagnosis isn’t that uncommon. 03:53 It could be a tricky thing to figure out because children this age can’t tell you why things hurt. 03:59 And sometimes, you just confuse this for something like gastroenteritis. 04:05 However, if a delay in diagnosis is happening, children may develop complications. 04:11 They may develop obstruction at their intestinal wall. 04:14 The passage of material can’t continue to pass that intussusception and they have small bowel obstruction. 04:20 They may develop intestinal edema. 04:24 The edema may lead to intestinal ischemia or death of the bowel wall, which is a surgical emergency. 04:31 It can lead in turn to perforation. 04:34 And once that intestinal wall perforates, they may develop peritonitis, which is a bacterial infection of the entire peritoneal cavity. 04:44 Peritonitis eventually leads to shock, and potentially, even death if the diagnosis isn’t made or the child isn’t treated. 04:54 So, let’s go through typical physical exam findings for a child with intussusception. 05:01 On your abdominal exam, you may be able to palpate a sausage-shaped abdominal mass. 05:08 This is important to remember and this is often on a test. 05:12 Realistically, however, it’s very rare to find an actual palpable mass. 05:17 The reason being is that these children are usually noncompliant with your abdominal exam. 05:23 And when they’re resisting your abdominal exam, it’s hard to get through that abdominal musculature to actually feel the mass. 05:30 Takes some patience. 05:33 What you may notice is this mass, if it’s the classic ileocecal intussusception, is in the right upper quadrant, and that’s important to remember. 05:44 Patients may get a currant jelly stool. 05:49 I don’t know if you’ve ever seen currant jelly, but it’s that red thick consistency. 05:53 And when you see that, that is usually associated with intussusception. 05:58 However, remember, the majority of children, we actually don’t see bloody stools in. 06:04 Nonetheless, high yield on a test is currant jelly stools. 06:10 This is usually a later finding. 06:13 It’s a result of a delay in diagnosis, and that child is bleeding because the intestinal wall has become edematous and has started becoming getting damaged. 06:21 That child is at risk for peritonitis. 06:24 So how do we diagnose it? If we suspect intussusception, the test of choice is the ultrasound. 06:32 What we’ll do is we’ll hold the abdominal probe up to the abdominal wall and we’ll look inside and we’ll see this very classic picture, which is often common to go on the [00:06:41] test, and we’ll call it a target sign. 06:46 What you can see here is an inner intraabdominal intussusceptum. 06:51 That’s the piece of intestine that is entering the distal segment. 06:56 And an outer, intussuscipiens. 07:00 The intussuscipiens is the part of the intestine that is receiving the proximal material. 07:07 So, what you see then is this bull’s eye picture where you have the outer wall of the intestine followed by the inner wall of the intestine, and that’s a classic finding on ultrasound. 07:19 The inner piece and the outer piece. 07:24 How do we treat intussusception? Well, in most children, this is ileocecal, which means that if we could re-expand that colon, we can actually effectively push out the intussuscipiens, the proximal portion, pop it out, and actually fix the problem without doing surgery. 07:43 And this is in fact what we do. 07:46 Usually, we use air. 07:48 We used to do things like contrast enemas. 07:51 That’s less commonly performed now. 07:53 This is a nonsurgical approach that’s done by your radiologist where they insert air forcefully into the rectal vault and try to re-inflate that colon. 08:04 This image here is a contrast, not an air enema. 08:08 This has about a 75% success rate. 08:12 If that doesn’t work, we typically will then move on to surgery. 08:18 We often do surgery also if there’s peritonitis present. 08:22 In other words, the bowel has already perforated because we want those surgeons to run the bowel and look for areas of necrosis that might need to be cut out. 08:31 If there’s a concern for perforation, of course, we’re going to go for surgery for that very reason. 08:37 And if the child is acutely ill or toxic-appearing, chances are that’s what’s happened. 08:42 We’re going to be calling the surgeons. 08:45 Surgery is also indicated when a pathologic lead point is suspected, such as in children over 6 who often have lymphoma as a cause. 08:55 So, let’s review the important things to remember with intussusception that are likely to show up on your exam. 09:02 What is the most common location? We’re talking about the right upper quadrant. 09:06 Remember, the lower cecum has material that’s going up into the ascending colon, and you’ll notice that mostly in the right upper quadrant. 09:16 The classic triad of symptoms is right upper quadrant pain, a mass and bleeding in the stools. 09:24 The characteristic ultrasound finding is that bull’s eye. 09:29 And if you do a rectal exam in a child who has a delay, you’ll notice currant jelly stools. 09:35 And lastly, the typical age group for intussusception is in children between the ages of three months to six years with the most of them happening around a year of age. 09:46 If you see intussusception in a child who’s over six years of age, this is non-Hodgkin’s lymphoma until ruled out. 09:55 Basically, over six years of age, or really over five years of age, we’re worried about a pathologic lead point as opposed to something benign like a Peyer’s patch. 10:07 The last caveat I’ll leave you with before we end this lecture is that remember, there is one condition which is associated with intussusception that is different, and that’s Henoch-Schonlein purpura. 10:20 We’ll do a separate lecture on HSP, but remember, HSP causes more often, ileo-ileal intussusception rather than ileocecal intussusception because the lead point there is in fact one of the purpura from Henoch-Schonlein Purpura.
About the Lecture
The lecture Intussusception in Children by Brian Alverson, MD is from the course Pediatric Gastroenterology. It contains the following chapters:
- Intussusception: Pathology
- Intussusception: Signs & Symptoms
- Intussusception: Physical Exam Findings
- Intussusception: Diagnosis & Treatment
Included Quiz Questions
A 2-year-old boy presents with altered mental status and intermittent crying. What is the most likely diagnosis?
- Intussusception
- Gastroenteritis
- Duodenal atresia
- Gastroesophageal reflux
- Lyme disease
Which of the following is the most common type of intussusception?
- Ileocecal
- Ileoileal
- Colocolic
- Gastroduodenal
- Jejunoileal
A 2-year-old boy is brought to the clinic with intermittent colicky pain. Which of the following is most helpful to diagnose this patient if he has intussusception?
- Ultrasonogram
- Technetium 99m pertechnetate scan
- CT abdomen
- MRI abdomen
- Plain X-ray abdomen
You suspect that a boy has intussusception which is later confirmed by imaging. Which of the following is an indication for surgery in this patient?
- Signs of peritonitis
- Donut ring sign on ultrasound
- Projectile vomiting
- Intermittent crying
- Intermittent drawing up of legs
Which of the following is the classic triad of intussusception?
- Intermittent Colicky abdominal pain - Vomiting - Bloody stools
- Bloody stools - Vomiting - Nausea
- Vomiting - Dysphagia - Colicky abdominal pain
- Projectile vomiting - Sausage-shaped abdominal mass - First male child
- Diarrhea - Abdominal mass - Vomiting
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is one of the best lecture from Dr. Alverson, along the ones such as Asthma and bronchiolitis. It is very well explained and also contains clinical pearls that I'm quite sure my colleagues are not aware of. This lecture will help me to better diagnose this disease and better explain it to parents. I'm looking forward to use this knowledge in real life.
Everything is so well explained, he takes the time to put in his 2 cents from his own experience and highlights the high yield points for the exams. Not to mention any time I've asked a question, I've got an answer the very next day