Playlist
Show Playlist
Hide Playlist
Intestinal Malrotation
-
Slides Structural GI Diseases.pdf
-
Download Lecture Overview
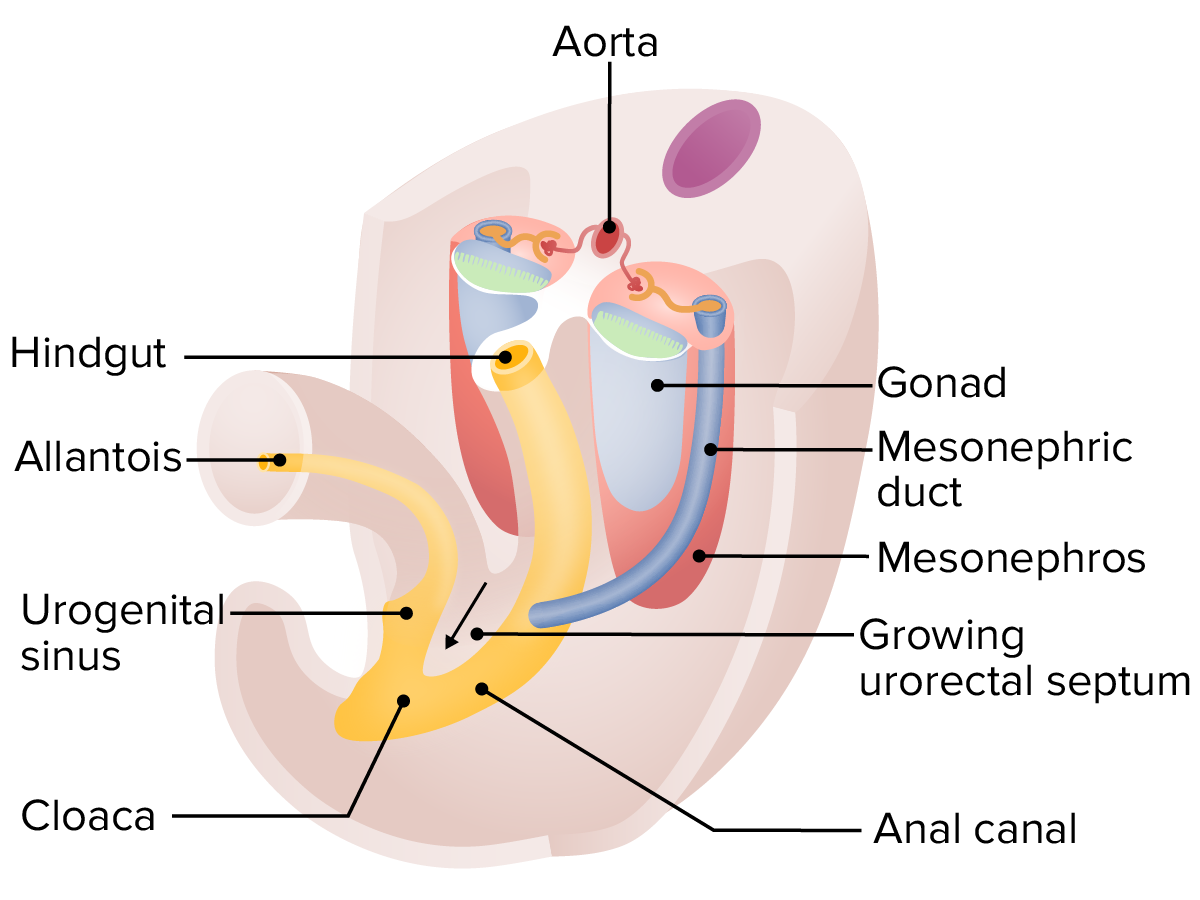
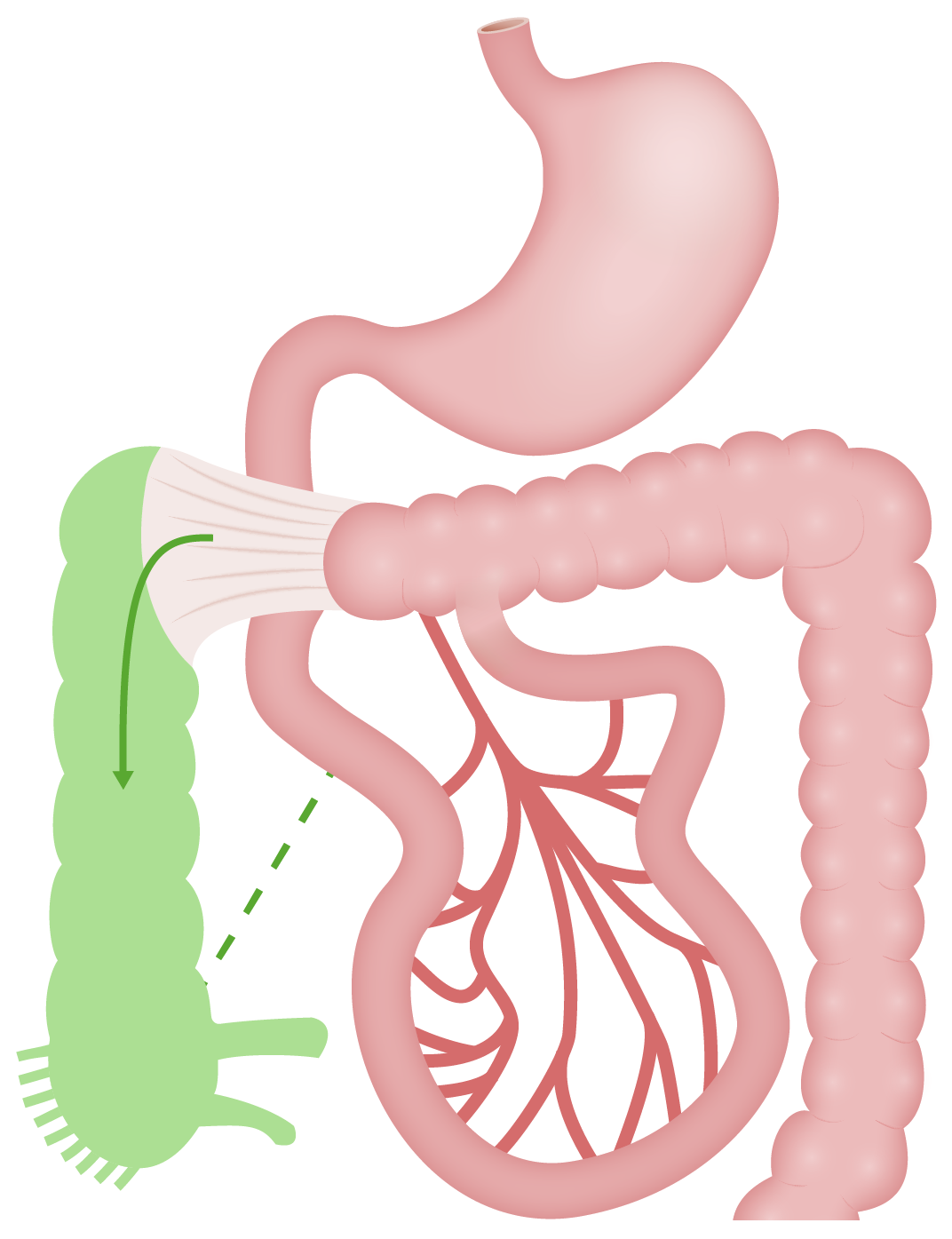
00:02 Let’s switch gears to malrotation. 00:05 This isn’t so much a problem with the enteric passage itself, but rather that it’s mislocated within the abdominal wall. 00:13 So, here’s a classic example. 00:15 An infant is born three weeks of age, could be older, and is brought to the emergency department presenting with bilious or dark green vomiting and abdominal pain. 00:25 He gets an urgent upper GI contrast study which shows emptying of stomach contents into the right lower quadrant instead of across the ligament of Treitz. 00:35 So bilious emesis in any baby is concerning. 00:40 Abdominal pain, and certainly, when you see emptying of stomach contents into right lower quadrant on the upper GI study, you know this child has malrotation. 00:54 So, what’s malrotation? This is one of the most common causes of intestinal obstruction in infancy. 01:01 It is a surgical emergency. 01:03 These children may not go home and come back later. 01:07 This presents as a volvulus. 01:10 Fifty percent of these children will present in their first month of life and 90% will present in their first year of life, although a tiny percent may present years later. 01:23 This is caused by an incomplete rotation of the gut during embryological development. 01:29 Recall your embryology. 01:31 The gut actually passes outside of the child, twists around and then goes back in again. 01:36 If that rotation is incomplete, this child may have malrotation. 01:43 So, what you’ll see when you look at the child now that they’re born is the cecum remains high up in the abdominal compartment and fixed, attached to the posterior abdominal wall. 01:56 It’s attached there by Ladd’s bands, which are remnants of peritoneum that are fixing it against the abdominal wall. 02:04 These Ladd’s bands now may obstruct the duodenum and prevent the passage of food out past the stomach through to the duodenum and into the jejunum. 02:16 So, what you can see is these children will have an abnormal location, where the dotted lines are in this film, and it will be moved up and the Ladd’s bands will be fixed there obstructing the duodenum. 02:30 Patients with malrotation will have acute, forceful, and this is key, bilious emesis. 02:37 Bilious emesis in a child under one year of age is malrotation until proven otherwise. 02:44 That’s a very important clinical pearl. 02:48 These children will absolutely get small bowel obstruction and all the compromises that can happen as a result including peritonitis, sepsis, shock, and death. 02:58 Early onset is classic, usually in the first year of life like we said, and often in the first month, these children will get abdominal distention and they often may present as bloody diarrhea later as that intestinal wall is now desiccating and necrotic and they’re now bleeding into their intestinal compartment. 03:17 Later onset patients, those rare that come later, may be asymptomatic. 03:22 They may have chronic insidious emesis. 03:25 They may have failure to thrive, anorexia or poor feeding and they may suffer from malabsorption. 03:31 So these children are sometimes harder to detect. 03:36 So physical exam findings in children with malrotation include that early, they may be relatively well appearing. 03:42 The mom says, “My baby has been so healthy her whole life." "I don’t understand why this is happening.” The child should have signs of dehydration, some abdominal distention, some diffuse abdominal tenderness. 03:53 It’s rare for a baby to be able to localize their tenderness. 03:57 Shock or sepsis is common especially if there is a delay in diagnosis or the child has been having symptoms for many days prior to presentation. 04:08 Guaiac-positive stool, or frankly, bloody stool is a sign that this has been going on too long. 04:15 So, to make the diagnosis, any infant with bilious emesis has malrotation until proven otherwise. 04:23 An ultrasound or radiologic studies are indicated, and we’ll talk about what those are. 04:29 And then, we must do a surgical evaluation and a surgical correction for this problem. 04:35 So the radiologic findings, most centers are moving towards ultrasound. 04:41 An experienced ultrasonographer can follow the sweep of the intestine and actually comment on the orientation of the blood vessels into the intestine. 04:50 Keep in mind if a child has malrotated, essentially, twice, the orientation of the blood vessels may still be normal and then it will require understanding whether they followed the sweep of the intestine. 05:02 It’s important to speak with the ultrasonographer and determine exactly what they found in a case like this. 05:09 If the ultrasonographer isn’t sure, we would proceed to an upper GI. 05:15 A plain film and an upright abdominal X-ray may show distended loops of bowels with air-fluid levels but is unlikely to make the diagnosis. 05:24 What you can see here on the right side of your slide is an upper GI. 05:29 And in this case, they did a small bowel follow-through that is not necessary to make this diagnosis. 05:36 The green arrow is showing a corkscrew-like drainage of the duodenum as it’s failing to cross over the body and across the ligament of Treitz onto the left upper quadrant. 05:49 So the drainage of the fluid coming out of the gastric compartment is going inferiorly instead of across in a corkscrew-like manner. 06:02 This is classic for malrotation. 06:06 You can see the duodenal contents are inappropriately located in the right lower quadrant instead of the left upper quadrant. 06:17 So, if we suspect the child has malrotation, and we’ve shown it either on ultrasound or an upper GI, we now have to manage this patient. 06:26 Critical is fluid resuscitation. 06:29 These children are usually dehydrated, and we’ll start with fluid resuscitation so that they’re stable for surgery. 06:35 We will also correct any electrolyte imbalances that might be happening. 06:40 Broad spectrum IV antibiotics will be indicated for septic patients, children who’ve gone on too long. 06:48 An example of antibiotics I might choose are Zosyn, or you might choose a fourth-generation cephalosporin and vancomycin. 06:57 Generally, very powerful broad spectrum antibiotics. 07:03 Then, we hand these children over to the surgical team and they will perform the Ladd procedure. 07:10 This is a resection of the necrotic portion of small bowel and a reorientation of the intestinal contents within the abdominal compartment. 07:20 So, potential complications of a malrotation are necrotic bowel. 07:25 If these children need a large amount of bowel removed, they will develop short gut syndrome, which is a real problem and may require long-term hyperalimentation resulting in liver failure, or in worse case scenarios, may require a small bowel transplant. 07:44 Sometimes children, postoperatively, will develop adhesions which can then later result in, again, a small bowel obstruction.
About the Lecture
The lecture Intestinal Malrotation by Brian Alverson, MD is from the course Pediatric Gastroenterology. It contains the following chapters:
- Malrotation: Case Study
- Malrotation: Pathology
- Malrotation: Signs & Symptoms
- Malrotation: Diagnosis
- Malrotation: Management
Included Quiz Questions
What is the most important finding that would suggest an infant has intestinal malrotation?
- Bilious emesis
- Shock
- Fever
- Diarrhea
- Blood in stool
A newborn girl is having bilious emesis. An upper GI study is done. Which of the following findings in imaging study is indicative of intestinal malrotation?
- Emptying of stomach content into RLQ instead of across the ligament of Treitz
- Gas shadow under the right dome of diaphragm
- Distended transverse colon
- Multiple air-fluid levels
- No specific finding
Which of the following therapy is indicated before corrective surgery is performed for intestinal malrotation?
- Fluid resuscitation
- No preparation is required
- Laxatives
- Enema
- Intra-rectal antibiotics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. Best explanation I heard so far of the disease. Thanks!