Playlist
Show Playlist
Hide Playlist
Intestinal Malrotation
-
Slides GIP Intestinal Malrotation.pdf
-
Download Lecture Overview
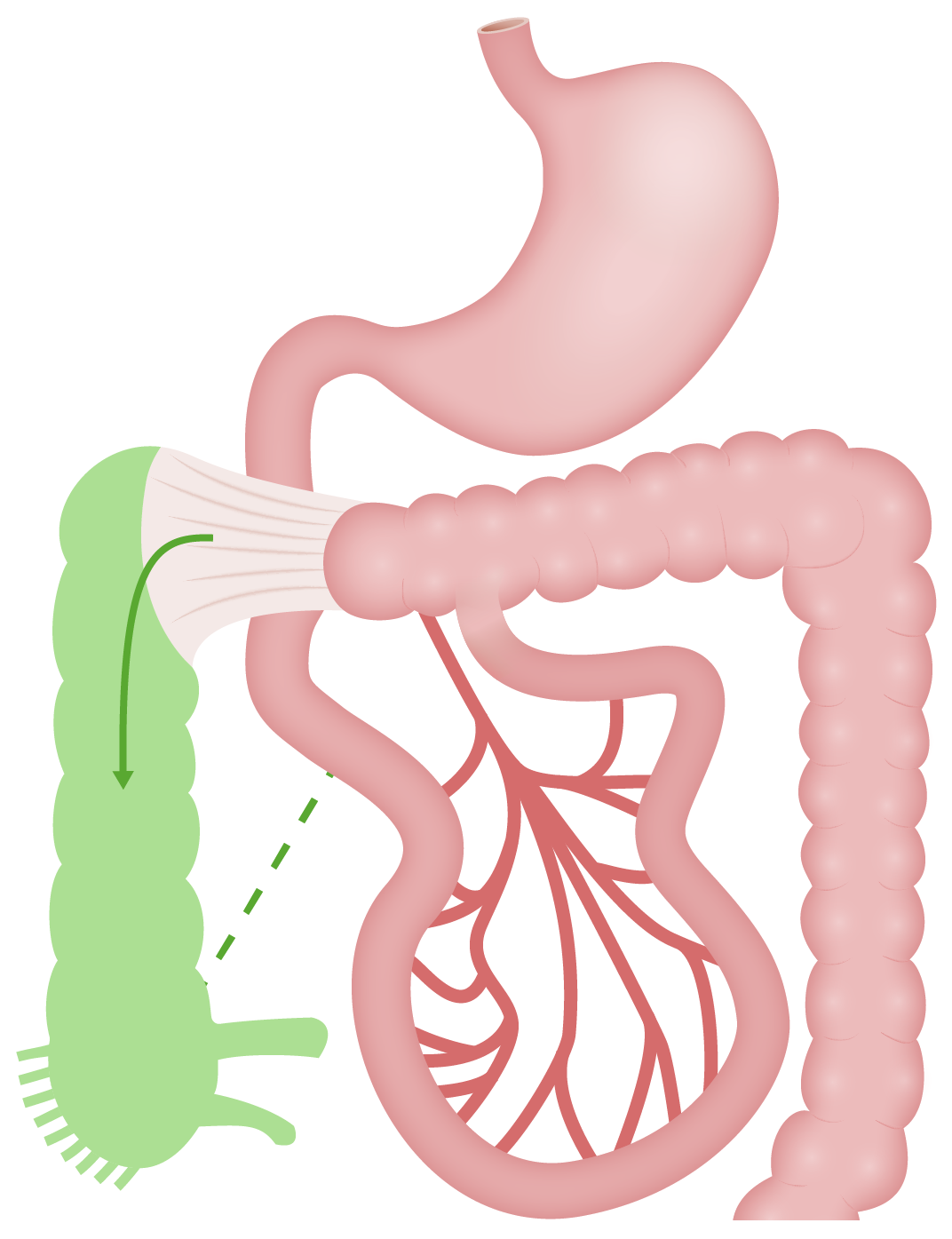
00:00 In this talk, we're going to cover the topic of intestinal malrotation, which occurs remarkably quite frequently, but in most cases, is completely asymptomatic. 00:15 So intestinal malrotation is a failure of the GI tract undergo its normal rotation. 00:20 You'll see in a moment, we'll give you a video. 00:23 The bowel goes through some pretty impressive contortions as it develops in utero. 00:30 If it doesn't completely go through its normal folding and rotation around the mesenteric vessels during embryogenesis, then you can potentially have some pathology. 00:42 The epidemiology, as they said, this is remarkably common, about 1 in 500 births. 00:48 It doesn't mean that all of these babies are going to be symptomatic. 00:51 And indeed, many people are walking around some of you watching this video, who have this particular anomaly, and you're just fine. 00:59 You'll see that it will vary depending on the severity of the malrotation. 01:04 So about 30% of babies who have this, who have significant malrotation will be picked up within the first month of life. 01:11 And usually, if they're going to be symptomatic, they'll be picked up within the first year of life. 01:16 So if you're a medical student, and you're watching this now, and you've not been diagnosed, don't worry about it, you're not going to have any problems. 01:24 60% of the babies who do have symptomatic disease will have some other congenital anomaly. 01:31 So if this is associated with a variety of other genetic problems, and also some developmental problems that may be related to the failure to rotate appropriately. 01:45 For example, a congenital diaphragmatic hernia where they just don't have complete development of the diaphragm, and you have the bowel pressing up into the thoracic cavity. 01:56 So for the pathophysiology, let's look at this because this is impressive in terms of all of the contortions the bowel will go through. 02:03 The overall mechanism, what's driving this is not completely understood. 02:08 All we can do is say this is what is known to happen. 02:12 There's clearly in many cases a genetic basis, particularly in those babies who have other congenital abnormalities. 02:20 So normally, the loops of bowel start developing outside of the abdomen, that happens as a result of the elongation of the bowel, along the umbilical cord into the yolk sac. 02:35 We have to actually if you think about it expand from about millimeters of bowel initially in the developing fetus, to something it at full length is going to be about 7 meters of small bowel and 1.5 meters of large bowel. 02:52 In order for this to happen, you have to have some elongation, so a lot of growth. 02:57 It's protruding outside of the abdominal cavity. 03:00 And then at some point, it starts to rotate. 03:03 It's about a 270 degree rotation counterclockwise, as you look at the umbilicus counterclockwise, that allows them the small bowel to loop around and underneath the larger bowel. 03:17 And eventually you're going to have the gastroduodenal junction with the ligament of Treitz tacked up into the left upper quadrant and the cecum tacked down into the right lower quadrant. 03:31 And that gives us the final confirmation that we're used to seeing when we do abdominal dissections or just anatomical dissections. 03:41 So there can be varying degrees of malrotation, this entire convoluted process. 03:47 What's being shown here is complete non rotation. 03:51 The small bowel sits completely over on the right side of the abdomen and the colon sits completely on the left side. 03:58 And the mesenteric vessels are splayed out, as you see there. 04:04 The cecum in a incomplete rotation kind of sits mid abdomen just underneath the epigastrium. 04:10 So that's a partial malrotation that is tethered in place. 04:15 So instead of having that tethered in the right lower quadrant in the normal rotation, it's tethered into midline with the lads bands, so fibers connective tissue and the cecum sits up there. 04:29 As part of this malrotation process, you may actually twist the mesentery. 04:34 It's not developing appropriately and it may become captured up into these loops of bowel that are not spinning appropriately. 04:42 And when that happens, you have a volvulus. 04:44 You will have compromised of the vasculature to various portions of the bowel. 04:49 So the mesentery becomes twisted. 04:51 As a result of that you can have ischemic bowel or a completely obstructed small bowel is part of this tied intestines in knots. 05:01 So the clinical presentation will depend on whether you have a partial malrotation or a complete malrotation. 05:09 And depending on whether you've compromised vasculature or you have twisted the bowel and actually tied it up on itself. 05:16 As I've already pointed out, most of you are most of the people who will have this will be completely asymptomatic. 05:23 And they would only be diagnosed when they go to surgery, for example, for something happening otherwise in the abdomen. 05:29 There may be duodenal obstruction. 05:32 So many of the times with that partial malrotation, the duodenum is compromised, and you will not have good gastric emptying. 05:40 As a result of that, you'll frequently bilious vomiting, forceful bilious vomiting as a result of that duodenal obstruction. 05:50 Sometimes, if the obstruction is more proximal to the ampulla of Vater you won't have any bile within that. 05:58 So besides the bilious vomiting, you will also frequently have abdominal distension. 06:03 There's food not moving through the GI tract appropriately as a result of the volvulus. 06:10 Late signs when there's very symptomatic disease can include any of the things you would expect as you are infarcting or otherwise damaging the GI tract. 06:19 So you may have hematochezia, bright red blood per rectum. 06:24 You may have hematemesis, you're vomiting blood. 06:27 As a result of blood loss, and malabsorption, the baby may be hypotensive. 06:33 As a result of the hypotension and the blood loss, the baby may become diaphoretic, and clearly tachycardic. 06:39 So these are all kind of secondary to the loss of blood and/or the obstruction. 06:47 We've changed from a baby to a young kid. 06:50 In this particular case, this was not as severe, a malrotation. 06:55 So there is more of a midgut volvulus that appears later on in life, early years 7, 8, 9 or into the teenage years. 07:05 There may be vomiting that's associated with this as the bowel becomes obstructed. 07:10 There will be failure to gain weight because there is malabsorption. 07:14 The baby may or the young adult may have chronic diarrhea, and there will clearly be abdominal pain. 07:20 The diagnosis is made on a variety of imaging and clinical evaluations. 07:27 So the classic study that is performed to look at this is an upper GI series. 07:34 So we put in barium, or we have the patient ingest barium, and then we follow that through the early portions of the GI tract. 07:43 One, we want to rule out that there's no perforation. 07:46 So if we have ischemia, we have an injury, we may have perforated, that's a surgical emergency. 07:53 In this particular case, what we're seeing is a double-bubble sign. 07:56 So we're seeing on the right hand side, a big bunch of barium that's in the stomach, and then it's coming out through the pylorus. 08:03 And the proximal duodenum has kind of a bubble. 08:06 And then there's a narrowing, and then there's a more distal bubble. 08:10 That's the double-bubble sign. 08:12 And that narrowing in between is where we've malrotated the valve. 08:17 The upper GI series, they said as the gold standard when the patient is hemodynamically stable. 08:23 So the ligament of traits. 08:25 Remember, we talked about the duodenojejunal segment being tethered into the left upper quadrant that's through the ligament of Treitz. 08:32 If that sits to the right of midline, and we can see that on various imaging series, then we know that we have a malrotation. 08:43 The duodenum may also very frequently have a classic corkscrew appearance. 08:47 And this kind of makes sense if you think about this basically wrapping on itself. 08:52 And that indicates that we also have a volvulus, the bowel is tied up in knots. 08:58 What do we do about this? So clearly, if it's really severe and symptomatic, we need to give fluid resuscitation, we need to give intravenous antibiotics because there's probably some degree of bowel necrosis and we have GI flora leaking into the perineum. 09:13 We want to keep the baby or the young kid completely NPO that means Nils per os for the Latin speakers out there. 09:22 So nothing by mouth, and we clearly want to do a surgical correction. 09:29 For very healthy children with no bowel ischemia, the mortality is near zero. 09:34 And in fact, as I already intimated, you can have this and not be symptomatic at all for your entire lifetime. 09:42 But with greater severity of the malrotation and with volvulus, and with infarction, the mortality will clearly increase. 09:51 So if we have intestinal necrosis. 09:54 If the baby has to be born early because of the maldevelopment, if there are other associated congenital anomaly, the incidence of death will increase. 10:04 Usually surgery does pretty well. 10:07 And patients that need to go to surgery usually will survive if there's about a 3-9% even after surgery. 10:16 With that we've covered bowel malrotations.
About the Lecture
The lecture Intestinal Malrotation by Richard Mitchell, MD, PhD is from the course Congenital Gastrointestinal Tract Disorders.
Included Quiz Questions
What is the pathogenesis of intestinal malrotation?
- Abnormal rotation around mesenteric vessels
- Abnormal rotation around the duodenum
- Abnormal rotation around the central axis
- Abnormal rotation around the diaphragm
- BRCA mutation
What is a potential symptom of duodenal obstruction from malrotation?
- Forceful bilious vomiting
- Jaundice
- Hiatal hernia
- Rectal bleeding
- Shortness of breath
What are the important steps in the management of intestinal malrotation?
- Fluid resuscitation, antibiotics, NPO, surgery
- Fluid resuscitation, lower GI series
- Fluid resuscitation, colonoscopy, biopsy
- BRAT diet, antibiotics, surgery
- BRAT diet, surgery
Why does the bowel initially develop outside of the abdomen?
- Elongation of the bowel along the yolk sac
- Elongation of the bowel along the liver
- Elongation of the bowel along the spleen
- Absence of peritoneum
- Absence of pericardium
What is the typical presentation for non-volvulus malrotation?
- Asymptomatic
- Epigastric abdominal pain
- Jaundice
- Fever
- Chills
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |