Playlist
Show Playlist
Hide Playlist
Inclusion Body Myositis
-
Slides Inflammatory Myopathies.pdf
-
Download Lecture Overview
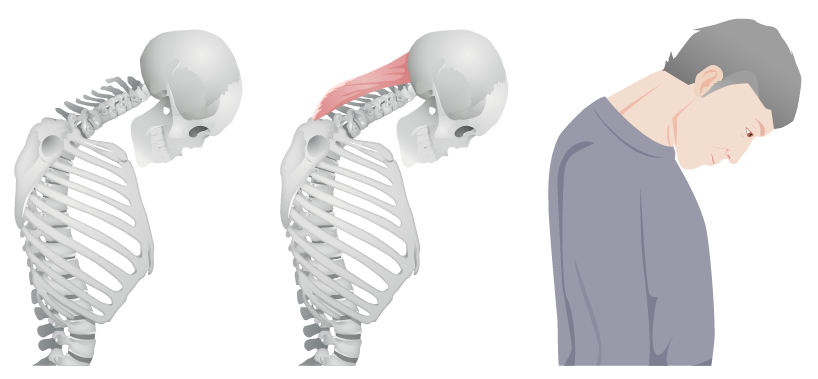
00:00 So, now let's move to the 3rd type of inflammatory myopathy, inclusion body myositis. And again, we're going to draw on some important similarities and differences between inclusion body myositis or IBM and poly and dermatomyositis. For inclusion body myositis, we typically see a sub-acute or even a chronic onset. And some of these patients have symptoms that are developing over the course of years which is different from what we typically see with poly and dermatomyositis. How about the distribution? Well, here distribution is critical. 00:35 We see in inclusion body myositis the distribution is more likely to be asymmetric. Poly and dermatomyositis are very symmetric, the weakness is same on the right as it is on the left. 00:45 And that's not the case for many patients with inclusion body myositis. It is still painless. 00:50 These are myopathies and not myalgias. But the distribution is different. And this is important and something that I would like for you to remember. Patients typically present with proximal lower extremity weakness. Again, difficulty getting upstairs, difficulty raising out of a chair. 01:08 But in the upper extremity, they have distal weakness. Difficulty gripping or holding on to things, or eating, or using a utensil. And that distribution should point us away from poly and dermatomyositis towards inclusion body myositis. What about sensory changes? It's a myopathy, so we really shouldn't see sensory changes, it's often normal, but patients may have a co-occurring neuropathy and that's unique again to IBM and something that we should consider. It's okay to have some sensory changes if we're concerned about inclusion body myositis. And consistent with that, we see reflexes are often normal to maybe decreased and again there may be a little bit of a neuropathy component that we find on exam or see on our nerve conduction study and that's not inconsistent with this diagnosis. And see or hear, we see a patient and you can see in his hands, there's atrophy particularly of the muscles on the thenar eminence and there's clear involvement of weakness of the distal muscles of the hands and arms and this would be suggestive of patterns, suggestive of inclusion body myositis. What about the work-up for inclusion body myositis? Well again, we're looking for signs of an inflammatory myopathy and so the first thing we do is check the CK, and we can see elevations in the thousands. This can be variable based on the timing of the patient's presentation and typically the CK elevation is less than what we see with poly and dermatomyositis. Importantly, on muscle biopsy, we see a characteristic finding inclusion bodies containing amyloid within the muscle. a muscle biopsy is not required to establish this diagnosis. But when that's performed, the presence of inclusion bodies, amyloid deposits within the cell is diagnostic of this condition. And again, we can't underscore the importance of the physical exam. The classic distribution with weakness that involves the wrist flexors, the finger flexors and knee extensors, proximal lower extremity, distal upper extremity is critical in diagnosing this condition. Management is a little bit different than poly and dermatomyositis. Inclusion body myositis tends to be more refractory to steroids. We typically try steroid treatment in selected cases, but it's not always effective. So, what about the pathophysiology? What's going on in inclusion body myositis to take the normal fascicle and result in a damaged fascicle? Well, let's walk through what's happening to healthy myocytes and turning them into degenerating myocytes. We're going to see some similarities with poly and dermatomyositis. Immune cells are involved but importantly, inclusion body myositis is a degenerative condition and so the primary driver is really degeneration of the muscle and the myocyte as opposed to inflammation around it. We do see CD8 T-cells around muscle fibers, but importantly we see autophagic vacuoles. This inclusion bodies within the myocytes where there's accumulation of excess proteins and this is a key driver of the degeneration and necrosis that's happening within the muscle. Importantly, we look at the capillaries and we can see capillary changes as well. So let's focus in a little bit further on what's happening at the level of the muscle. This is a chronic inflammatory condition and we see around the myocyte, infiltration of cytotoxic CD8 cells. The express MHC class 1 and are attached to a degenerating or necrosing muscle fiber. Importantly, the driver of this process is not the primary inflammation from the CD8 cell. The first process isn't that the activated T-cell travels to the muscle, but something else sets off this degeneration of the muscle and the CD8 T-cells are responding to that process. This is somewhat unclear, our field hasn't worked out all of those details. It could be a virus. It could be muscle aging. There could be some abnormal protein process that's going on. This may be specific to certain HLA geno types. There may be impairment in autophagy and other mechanisms may drive the primary degeneration that sets this off. As a result of that process, there is a release of cytokines and chemokines around the muscle. Release of cytokines and chemokines attracts things like CD8 T-cells and we see those around the muscles. But what's going on inside the muscle fiber is accumulation of misfolded proteins. Amyloid, phospho-tau, ubiquitin. These excess proteins are accumulating and we see them in vacuoles inside muscle fibers. All of these are indicative of cell stress and muscle fiber damage leads to weakness and degeneration begets further degeneration and this process continues in a chronic mechanism. So importantly, we're seeing inflammation around the muscle. But whereas the primary driver was the immune system for poly and dermatomyositis, this is really a degenerative condition which most explains what we see with vacuoles on the muscle biopsy as well as it's poor response to corticosteroids when we think about treatment. On the muscle biopsy, here are some characteristic findings. And again, we're looking at muscle fibers, those at the large bluish green and pink fibers that you see on the left and right here. We do see some inflammation. There are small purple lymphocytes in between the muscle fibers. But if you compare to what we saw with poly and dermatomyositis, we don't see as much muscle inflammation or inflammation around the muscle. And importantly, in the black arrows, we see vacuoles. Accumulation of amyloid and other proteins within the muscle fibers indicating degeneration.
About the Lecture
The lecture Inclusion Body Myositis by Roy Strowd, MD is from the course Acquired Neuromuscular Diseases.
Included Quiz Questions
What will a muscle biopsy show in a patient suffering from inclusion body myositis?
- Vacuoles within muscle fibers
- Perimysial and perivascular inflammation
- Intra-fascicular infiltration of CD8+ T cells
- Fatty replacement
- Normal findings
Which of the following is a characteristic clinical feature of inclusion body myositis?
- Muscle weakness proximally in the lower extremities and distally in the upper extremities
- Symmetrical distribution of muscle weakness
- Decreased ability to sense pressure or temperature changes
- Increased reflexes in both upper and lower extremities
- Acute onset
Intracellular deposition of which of the following is characteristic of inclusion body myositis?
- Amyloid
- Hyperphosphorylated tau
- Sphingomyelin
- PAS-positive inclusions
- Glycogen
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |