Playlist
Show Playlist
Hide Playlist
Pediatric Inflammatory Bowel Disease (IBD): Diagnosis
-
Slides Inflammatory Bowel Disease.pdf
-
Download Lecture Overview
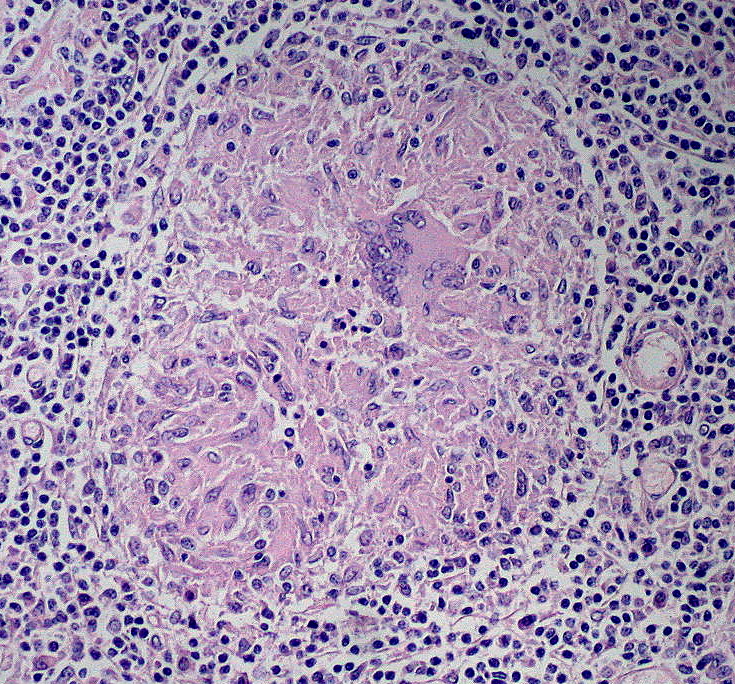
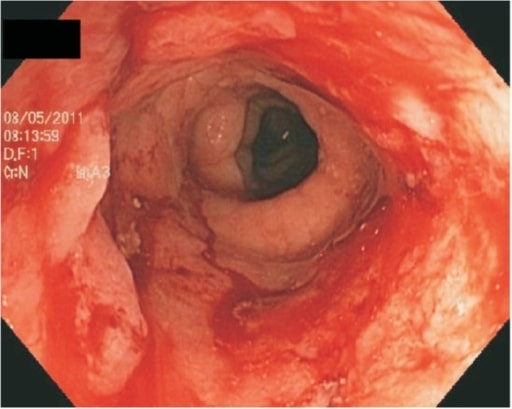
00:02 So on physical exam, one key aspect to check in any child where we’re suspecting inflammatory bowel disease is the vital signs and growth trends. 00:14 The growth trends are important because it’s frequent in children who are diagnosed with inflammatory disease to have a history of malingering and low level symptoms for even years prior that had gone ignored. 00:29 The abdominal exam, you will note tenderness with or without distention depending on the severity and the area of the illness. 00:37 Ileitis is common in Crohn’s disease. 00:40 So a right lower quadrant mass or tenderness may herald as a Crohn’s disease patient. 00:49 Of course, it could also be appendicitis. 00:51 What you’re looking for is that in connection with a chronic malingering course. 00:57 Certainly, patients with perianal skin tags, fissures, and fistulae are strongly concerning for Crohn’s disease. 01:04 Keep in mind, the patients with Crohn’s and other IBD may have extraintestinal manifestations of inflammatory bowel disease. 01:14 This includes uveitis, the apthous also as you see in Crohn’s, arthritis, arthritis, pancreatitis, skin rashes, especially erythema nodosum. 01:26 Remember erythema nodosum is a rash primarily on the shins, red, swollen lesions that are reasonably large and quite tender. 01:37 Also, these patients may have jaundice if they a hepatitis picture. 01:41 And certainly, these patients may develop delayed puberty or delayed growth as a result of chronic inflammation and infection. 01:50 Patients with inflammatory bowel disease will often have abnormal lab findings that are relatively nonspecific. 01:58 Iron deficiency anemia is common both because of inflammation but also because of chronic low level blood loss and a lack of adequate oral iron intake. 02:10 Patients with Crohn’s disease and ulcerative colitis may also have elevated sed rate and elevated CRP. 02:18 These three things are quite common and will occur in up to 75% of patients with inflammatory bowel disease. 02:26 Another key one which we see frequently in patients who are admitted for their first known flare is a low albumin. 02:35 Additionally, we can get stools studies that can be diagnostic such as a fecal calprotectin, which can help us make the diagnosis or we can look for things in stool that aren’t getting absorbed because of malabsorption, like alpha-1 antitrypsin or fecal fat or other tests along that line. 02:55 Stool studies include infectious enterocolitis because sometimes, a child with bloody diarrhea don’t have inflammatory bowel disease, they have bacterial enterocolitis. 03:07 This may be where this new this new PCR testing that is just starting to come out on stool comes in very helpful. 03:16 If a patient is on his way to the OR for what is presumed to be inflammatory bowel disease and the PCR test develops something like Yersinia, it’s possible that we’ve missed the opportunity to make a diagnosis of infectious enterocolitis. 03:31 And this child does not require an operative procedure. 03:35 C. diff testing is usually indicated. 03:38 However, keep in mind, patients with inflammatory bowel disease are actually more prone to C. diff infections. 03:45 So a C. diff infection does not rule out the presence of inflammatory bowel disease. 03:52 This new test, relatively new, that we obtained, which is the fecal calprotectin is much more highly sensitive and specific for inflammatory bowel disease. 04:01 We can also get a lactoferrin. 04:04 And like I stated before, we can do fecal fat and alpha-1 antitrypsin. 04:10 So if we suspect inflammatory bowel disease because we don’t want to right off do endoscopy on everyone, we may choose do some imaging, but do remember, upper and lower endoscopy with biopsies is the gold standard for diagnosis. 04:25 There’s no one where we’ll make a diagnosis where we don’t do endoscopy. 04:30 There are classic endoscopic findings such as skip lesions in Crohn’s or continuous inflammation from the rectal upward in ulcerative colitis that we seen on endoscopy that might not be appreciated on imaging. 04:46 However, there are a few images we can get if we’re trying to get a sense of what’s going on. 04:53 The upper GI series may be useful in that it can identify lesions that are causing indentations of the mucosa of the upper GI tract. 05:03 We could get a CT scan, but again, we’re trying to move away from radiation in children. 05:09 So taking the world by storm now is MRE, which is magnetic resonance enterography. 05:18 This is an MRI of the intestine that is very good for picking up small bowel disease. 05:24 In fact, it’s about 90% sensitive. 05:27 So this is a very good test for Crohn’s disease in particular. 05:32 On this slide you can see characteristic differences between Crohn's disease and ulcerative colitis. 05:37 The site is different in these diseases and in Chron's disease it can appear really anywhere on the GI tract from the mouth to the anus. 05:45 And will skip areas. We call these skip lesions. 05:48 You can see spots here and there, but not continuously tipically. 05:52 In ulcerative colitis you will see continuous involvement backwards from the rectum. 05:57 It may go only a little way or it may go all the way to the ileocecal valve. 06:03 The histology is also different between these two diseases. 06:06 In Crohn's disease we'll see trends, mural involvement. You can see crypt abscesses and you can see granulomas or linear ulcerations. 06:15 However, in ulcerative colitis it's primarily a mucosal disease. 06:20 You can see cryptitis or crypt abscesses sometimes, but you will not see these granulomas.
About the Lecture
The lecture Pediatric Inflammatory Bowel Disease (IBD): Diagnosis by Brian Alverson, MD is from the course Pediatric Gastroenterology.
Included Quiz Questions
Which lab finding is NOT consistent with inflammatory bowel disease?
- Elevated anti-CCP
- Elevated ESR
- Elevated CRP
- Low albumin
- Elevated fecal calprotectin
A 12-year-old boy is diagnosed with inflammatory bowel disease. Which of the following extra-intestinal manifestations is most likely in this patient?
- Arthritis
- Recurrent pneumonia
- Inguinal hernia
- Cholecystitis
- Conjunctivitis
Which of the following laboratory findings is most likely in a patient with active Crohn's disease?
- High fecal calprotectin
- Elevated serum iron
- Bacteriuria
- Elevated albumin
- Stool Clostridium difficile toxin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. Important topic in paediatrics. I feel more confident to recognise this disease in children.