Playlist
Show Playlist
Hide Playlist
Hypernatremia: Etiology
-
Slides Water Balance Hypo and Hypernatremia.pdf
-
Download Lecture Overview
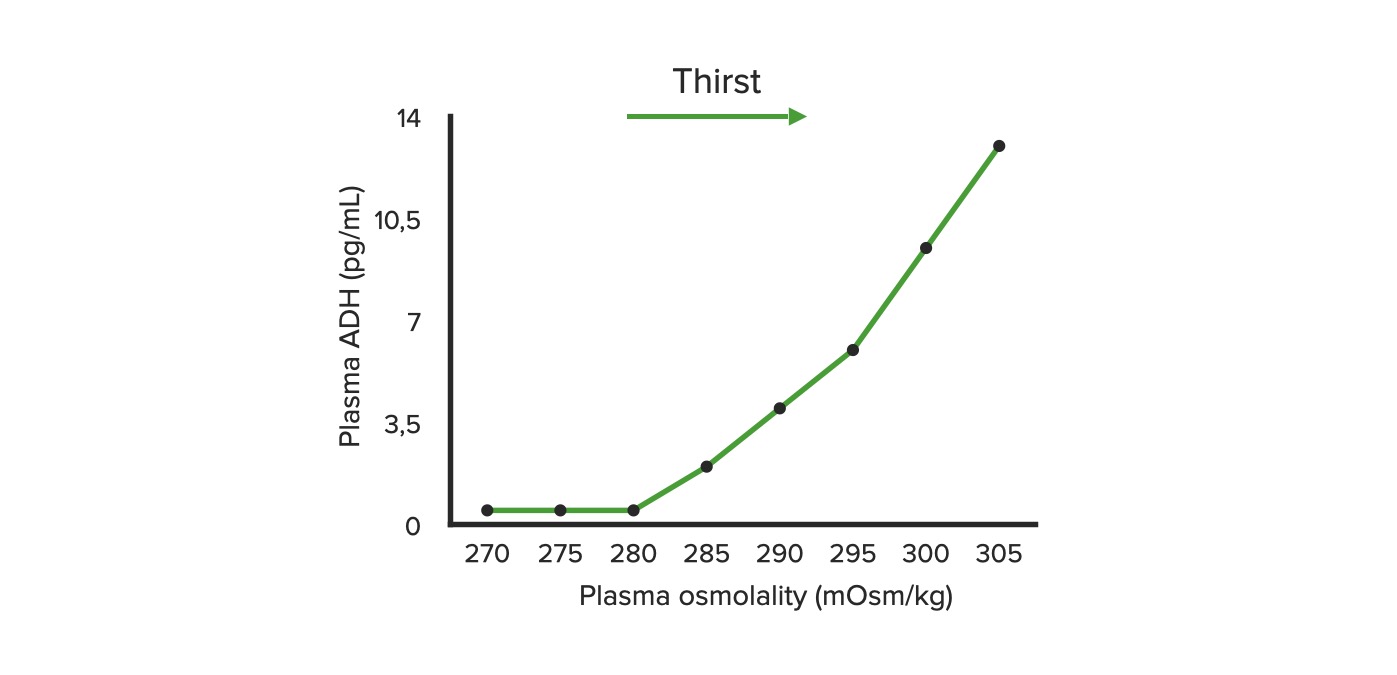
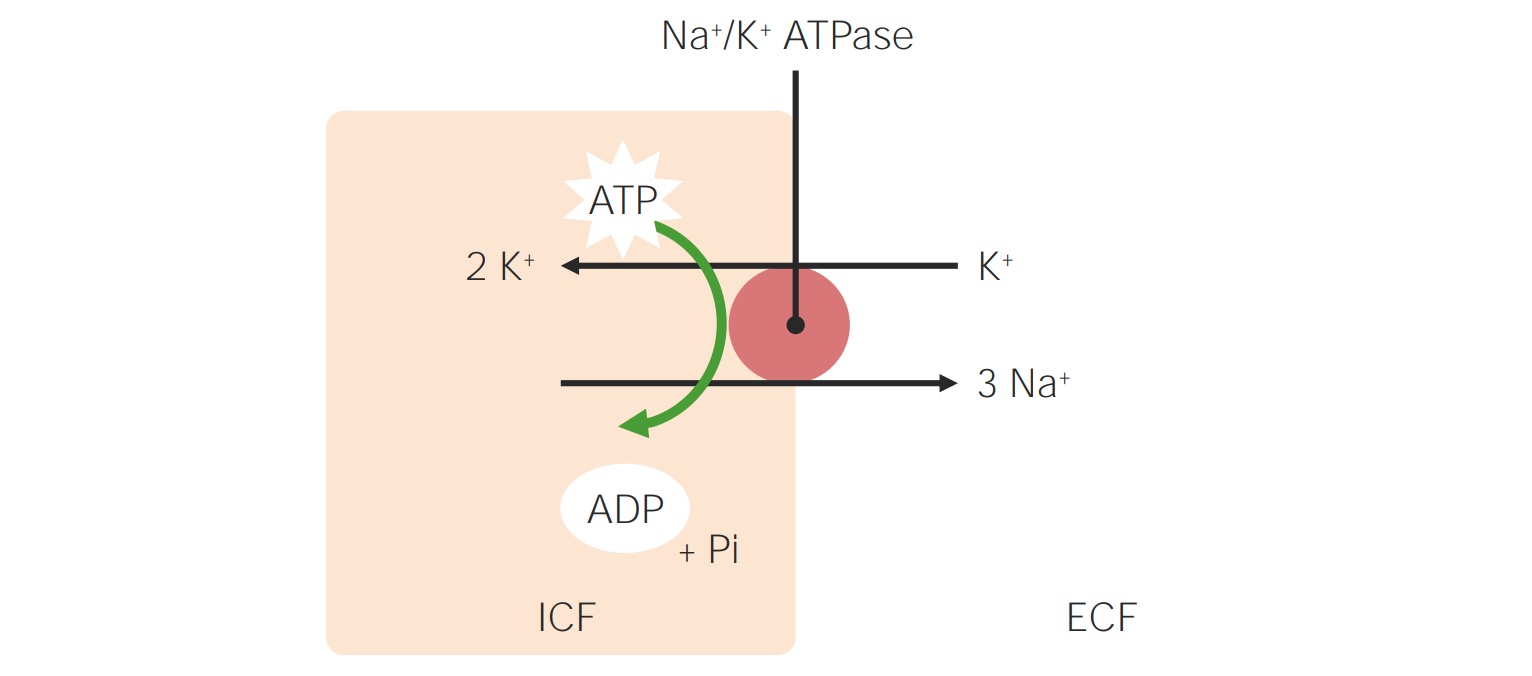
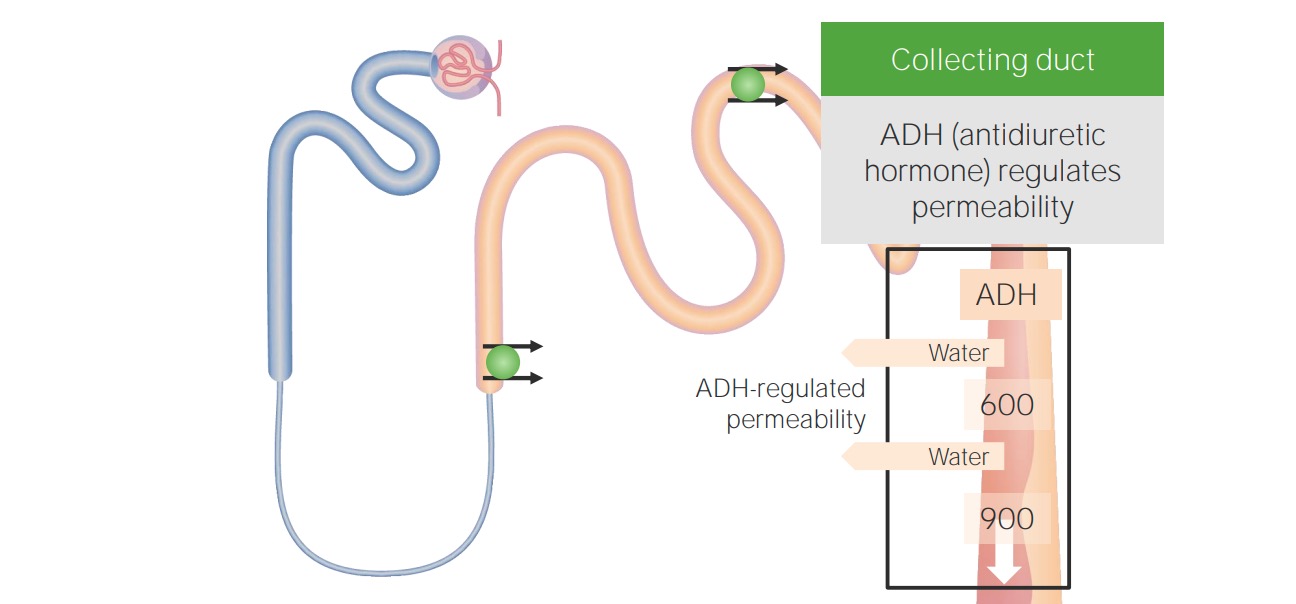
00:01 Let's move on to hypernatremia. 00:03 Hypernatremia is clinically defined when the serum sodium is greater than 145 mEq/L. 00:09 This means we have a loss of free water. 00:12 Rarely, it's due to administration of hypertonic sodium solutions. 00:16 And this affects about 9% of patients in the ICU setting, about 7% developed during their hospital course. 00:24 So, when patients are hypernatremic, there's a rise in plasma osmolality, which will stimulate the release of ADH that minimizes water loss. 00:35 And then thirst is also precipitated, so patients will increase water intake. 00:40 Now, even in the setting of something like diabetes insipidus with marked polyuria and water loss is due to reduced ADH effect, patients can still maintain a near normal serum sodium by increasing their water intake from thirst alone. 00:55 So, hypernatremia therefore is gonna result in patients who cannot express thirst normally. 01:01 Those are going be elderly patients or infants, or those who don't have the access to free water. 01:07 So, hospitalized patients in the ICU, for example. 01:11 When we think about the etiology of hypernatremia, it could be due to pure water losses. 01:17 These are patients who are hypodipsic, meaning that they have a decrease in their thirst mechanism. 01:22 It could be because patients have decreased free access to water or it could be the fact that patients will have insensible losses, dermal or respiratory losses. 01:33 And it can also be due to diabetes insipidus. 01:37 So, diabetes insipidus is essentially a decrease in ADH action at the collecting tubule, either due to a neurogenic cause, meaning that they have a decrease in ADH production or release, or a nephrogenic cause, meaning that they have a decreased effect at that collecting duct. 01:55 So, central diabetes insipidus, meaning that it's a neurological cause, is insufficient release of ADH in response to an increase in serum sodium or osmolality. 02:07 It can either be partial or complete impairment. 02:10 So, lesions of the hypothalamic osmoreceptors or supraoptic nuclei, or the superior portion of the supraoptichyophyseal tract, either with trauma, surgery, or tumors can result in this particular central diabetes insipidus. 02:27 In nephrogenic diabetes insipidus, this can also be partial or complete, and this is going to be due to a reduced action of ADH at that collecting tubule, either from a mutation in the V2 receptor or aquaporin channel, or it can be from medications like lithium. 02:44 So, what's critical to know, patients perhaps who have bipolar affective disorder, if they're on lithium, because they can absolutely manifest with a partial diabetes insipidus, and they should always have free access to water. 02:56 So, another category of hypernatremia are patients who experience hypotonic fluid loss. 03:03 That means that they have both sodium and water losses, but the solute concentration, that's the sodium plus potassium, is hypotonic to the plasma osmolality. 03:13 If they don't have free water replaced, they end up with hypernatremia. 03:19 So, the causes here to think about are gonna be skin losses. 03:22 Again, insensible losses and sweating. 03:25 GI losses, stool and gastric output. 03:28 Renal losses, so this can be things like osmotic diuretics, or things like glucose urea, urearesis, or mannitol, and then intrinsic renal disease where it impairs the concentrating ability in the distal collecting tubule. 03:46 Finally, our last category to think about is very uncommon, but you can have a hypertonic sodium gain. 03:54 So, this could be due to the administration of hypertonic sodium solutions. 03:58 We might see this from systemic absorption from somebody who has an intrauterine hypertonic saline administration for hysteroscopy. 04:06 We can also see this with salt poisoning. 04:09 So, surreptitious intentional salt poisoning is a form of child abuse. 04:14 If you think about it, one teaspoon of salt can actually increase the serum sodium by about 17 mEq/L in a 10 kg child. 04:22 We can see this in conditions like Munchausen by proxy, now referred to as factitious disorder imposed on another. 04:29 And then finally, salting, which is a cultural custom of scrubbing a newborn's skin with salt for up to one hour. 04:37 Now, when you do that, you can have systemic absorption of salt through the traumatized skin. 04:41 Again, these are very uncommon, but we do have to think about them. 04:45 So, the way patients clinically manifest when they're hypernatremic is typically with lethargy, seizure, or coma. Now, remember how smart our body is. 04:57 We have these adaptive mechanisms that can help us so that those neuronal cells don't shrink from having too little water. 05:03 So, what happens? We have movement of ions. 05:06 Remember that sodium potassium chloride which could move into the neuronal cells, and when they do that, water will follow, bringing again that cell volume to the normal level. 05:16 Now, if the hypernatremia lasts for more than 48 hours, we have more permanent adaptive mechanisms, and that includes osmolytes. 05:24 So, we collect more osmolytes that move into that intracellular compartment, again restoring that cell volume to the normal level.
About the Lecture
The lecture Hypernatremia: Etiology by Amy Sussman, MD is from the course Water Balance: Hypo- and Hypernatremia.
Included Quiz Questions
Which of the following is the most likely cause of hypernatremia in patients with bipolar disorder?
- Lithium-induced inhibition of the effect of ADH on the renal tubules
- Lithium-induced inhibition of the supraoptic nucleus in the hypothalamus
- Defective thirst regulation
- Decreased free access to water
Which of the following patient groups is at an increased risk for hypernatremia?
- Infants who are exclusively breastfed
- Patients with heart failure
- Patients with hypertension who are on ACE inhibitors
- Patients with hypothyroidism
- Patients with Fanconi syndrome
Which of the following is associated with hypotonic fluid loss?
- Excessive sweating
- SIADH
- Adrenal insufficiency
- Hepatorenal syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |