Playlist
Show Playlist
Hide Playlist
How to Read an ECG: Conclusion
-
Slides How to Read an ECG Conclusion.pdf
-
Download Lecture Overview
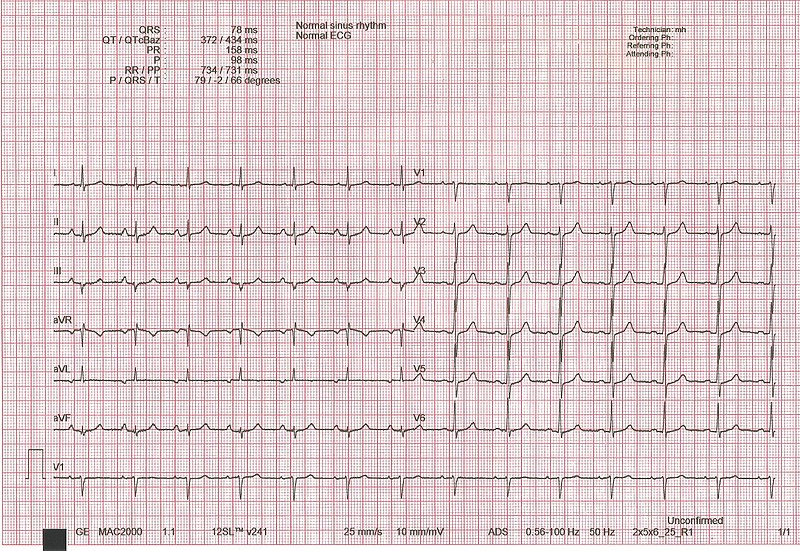
00:01 Welcome back to the ECG lecture series. This is the final one. 00:05 I'd like to review some of the important points that have been made throughout this lecture series. 00:10 And then I'd like you to identify some unknown ECGs. 00:14 You will have seen these ECGs or ones like it before. 00:18 And so, what I'd like you to do is when the unknown ECG comes up, please pause the program, think about the ECG and decide what your diagnosis is before you go to the next slide. 00:31 Because that one will tell you what the correct answer was. 00:35 So, some final thoughts. 00:38 First of all, reading an ECG takes time and practice. 00:42 And it is something that's just like I mentioned before, learning to play a musical instrument, you get better with time and with practice. 00:51 What you will have gotten out of this first series, you know, is a background so that you can start looking at ECGs. 00:59 I recommend you cover over the computer or the cardiologists reading, try and figure it out for yourself, then look and see what the cardiologists got. 01:07 And gradually as you do more and more and more, you'll become more expert. 01:12 Almost all ECGs these days in developed countries are read by the computer. 01:16 But unfortunately as I've said before, the computer is wrong particularly about arrhythmias 10-15% of the time and even sometimes over calls or under calls an acute myocardial infarction or heart attack. 01:29 So, an experienced electrocardiographer, usually a cardiologist should read the ECG - look over the ECG to make sure the computer is correct. 01:39 So, the reading of an ECG is comprised of the first of all, what's your overall impression? Just like with an artwork. And then you do the careful and detailed analysis. 01:52 The computer is usually right in terms of intervals: PR interval, QRS interval, QT interval. 01:57 It's not often write when the ECG has a complex arrhythmia. 02:03 That needs to be done by a human being and overread from - the ECG. 02:11 You need to check the ECG in a systematic process. So what do you do? You look first at the heart rate. You look at the - are there Ps in front of all the QRSs? You look at intervals, PR interval, QRS interval and the QT interval. What's the axis? Is the axis normal - normally directed somewhere down in this direction, +30, +60 or a little bit negative, -10, zero? If it's markedly abnormal, rightward axis or marked left axis that suggests a disease process either in the conduction system or often associated with organic heart disease. 02:51 Again, the computer is usually right about intervals, often wrong about rhythm. 02:57 The ECG does not only contain diagnostic information, but prognostic information. 03:02 Remember I mentioned, the bigger the ST segment in an acute MI, the higher it goes? The bigger is the infarct and the worse is the prognosis. 03:11 When there's ST-T wave changes along with LVH, the high-voltage, that's more serious than if there is no ST-T changes. Here's a cute one. 03:23 The sum of the total upright R wave voltage in all leads is a rough measure of left ventricular ejection fraction. 03:30 The opposite is the important point. 03:32 If you get an ECG that has very little R wave uprights in all the leads, it usually means markedly reduced left ventricular function, for example from cardiomyopathy. 03:42 And of course, the ECGs must be correlated and integrated with other clinical data from the history and the physical exam. 03:51 It's the same thing the radiologist tells you in interpreting the chest x-ray or a CT scan. 03:57 If you give them some clinical information so they know exactly what to look for, in fact, you get a better answer in terms of helping you clinically, and the same is true with the ECG. 04:08 Looking at the cardiogram when you know something about the patient is often more useful than just reading the ECGs blindly. 04:17 Remember that minor degrees of squared off ST segment depression may be important in a patient who's had chest discomfort that you're thinking, "This may have been angina. 04:27 There may be myocardial ischemia." In the exercise test, we like to see at least 1 mm of ST segment depression. 04:33 But if the patient just told you that they had some chest discomfort and you got an ECG and there was a little bit of ST depression, maybe half a millimeter that went away an hour later that's very suggestive of myocardial ischemia even though you didn't get the full millimeter. 04:48 Echocardiography, and by the way, MRI and CT are more accurate at predicting left ventricular hypertrophy that is LVH than the ECG. 04:58 However, when you see LVH on the ECG, it implies a worse and long-term prognosis for the patient. 05:05 So, it's usually more severe LVH than is picked up. 05:08 The Echo and the MRI are very good at picking up mild amounts of LVH. 05:14 ECGs for monitor leads should not be used to draw conclusions about the shape of the QRS or the ST segment. 05:21 I've seen the monitor leads over reads arrhythmias or calling marked ST elevations and so forth when it was just the patients moved in bed or changed their position. 05:32 So, don't use the monitor lead to try and interpret the ECG.
About the Lecture
The lecture How to Read an ECG: Conclusion by Joseph Alpert, MD is from the course Electrocardiogram (ECG) Interpretation.
Included Quiz Questions
When is it appropriate for a cardiologist to assess an ECG with the help of the artificial intelligence read?
- Always
- In the case of tachyarrhythmia
- In the case of bradyarrhythmia
- In the case of myocardial infarction
- In the case of heart failure
Which of the following statements is true regarding ECGs?
- It should be assessed in a systematic way.
- It provides only diagnostic information.
- It cannot be used to assess the prognosis of a diagnosis.
- It should not be correlated with clinical information.
- Monitor leads should be used to assess the QRS and ST segments.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr Alpert did such an amazing job with this ECG series! I've always had such a difficult time truly understanding this material and he did so well breaking it down to make it easy for me to understand. Thank you so much Dr Alpert! I can tell that you truly love cardiology from watching this series!