Playlist
Show Playlist
Hide Playlist
Human Immunodeficiency Virus (HIV): Signs, Symptoms & Opportunistic Infections
-
Slides HumanImmunodeficiencyVirus InfectiousDiseases.pdf
-
Download Lecture Overview
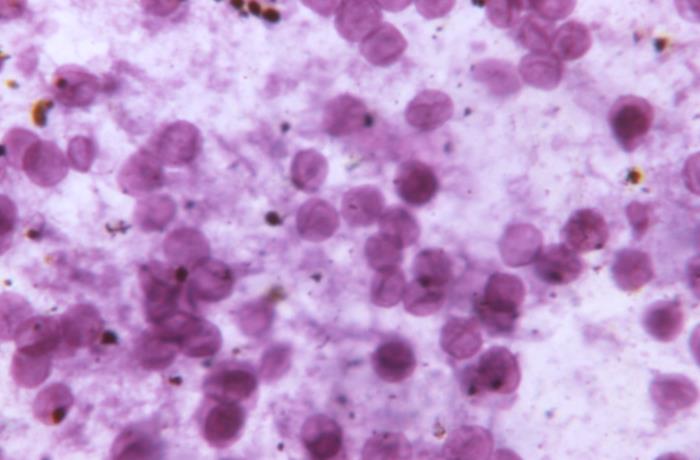
00:01 What results initially is something called the acute retroviral syndrome, which happens 1 to 6 weeks after infection. 00:11 And the most common presentation is an infectious mononucleosis-like illness with fever, rash, pharyngitis, sometimes aphthous stomatitis. Most patients experience myalgias. Some develop diarrhea. 00:29 And if they come to a physician, the physician may not only find lymphadenopathy, but hepatosplenomegaly during this acute retroviral syndrome. 00:41 So in a study of 209 patients who had the acute retroviral symptom, you can see that 200 of them, or 96 percent, had fever. 00:56 A large percentage also had adenopathy, pharyngitis, and rash. 01:03 And as you can see from these declining numbers, only a minority had thrush, or neuropathy, or encephalopathy. 01:12 The encephalopathy, of course, if it does occur, is very serious. 01:17 In the early days of HIV infection, we were actually staging patients using these following stages. 01:27 Stage 1 was considered having a CD4 T cell count of greater than 500 cells per microliter, or a CD4 T cell percentage of more than 29 percent. As far as clinical evidence, there may be none at this stage. 01:47 Stage 2 was a lower number of CD4 T cells, 200 to 499, or a lower T cell percentage. 01:56 But once again, there was no necessary clinical evidence. No AIDS-defining condition. 02:03 Stage 3 was classified as a CD4 T cell count of less than 200 per microliter, which is the definition of AIDS, or a CD4 T cell percentage of less 14 percent. 02:19 Alternatively, a documentation of an AIDS-defining condition, such as opportunistic infection that we would never find in a normal host with lab confirmation of HIV infection. 02:33 The reason this not as important today, although it’s still used is because we are treating everybody. 02:41 It doesn’t matter what class they’re in. Everyone is recommended to get antiretroviral therapy. 02:52 Now, some of the opportunistic infections are worth spending some time on. Here are just four examples. 02:58 Let’s start out with perhaps the most common opportunistic infection that you’d find, and this is pneumocystis pneumonia caused by Pneumocystis jiroveci. 03:11 And patients who get this generally have a CD4 T cell count of less than 200. 03:18 However, I have seen patients whose T cell count was greater than that. 03:25 The way patients present. They will have dyspnea, fever, and classically a non-productive cough. 03:33 And this may have been for the last several weeks to months. 03:39 On exam, they will have tachypnea, rapid breathing, tachycardia, and in some cases, fine crackles. 03:49 But they could have a completely normal exam on auscultation. 03:55 Their chest X-ray may range from normal to the more common bilateral infiltrates that are interstitial in nature. 04:07 The diagnosis is made by special stains of respiratory secretions, and sometimes bronchoscopy is needed to confirm this. 04:16 But what you see are these cysts that are classic for pneumocystis. 04:24 The treatment of this disease is trim sulfa, or alternative clindamycin and primaquine. 04:32 And as an adjunctive therapy, especially in patients who have hypoxia, we would use tapering courses of corticosteroids. 04:42 But we would not use steroids because it’s immunosuppressive, unless they had hypoxemia. 04:51 Cryptococcal meningitis is another common opportunistic infection that we find in HIV-infected persons. 05:01 And it is the most common fungal infection of a life-threatening nature after candidiasis, which is not life-threatening. 05:13 The greatest risk for cryptococcal meningitis would be a CD4 T cell count of between 50 and 100 per microliter. 05:22 And in this case, the patients may present in a real sneaky fashion with just headache, fever, visual disturbance. 05:33 I saw one patient whose only complaint was visual disturbance. 05:39 Their exam may show you meningismus, meaning a stiff neck, Kernig's or Brudzinski’s sign. 05:47 But because they don’t have much ability to produce inflammation with their depressed immunity, that occurs in less than 40 percent of patients. 05:58 You make the diagnosis by examining cerebrospinal fluid. 06:03 And so, a patient suspected of having cryptococcal meningitis should get a spinal fluid examination with protein, cell count, india ink mount. Now, I want to point out the india ink mount shown here. 06:18 India ink is basically a way for us to demonstrate that this is Cryptococcus with its capsule. 06:29 You see, if you just did a simple wet mount, all you would see would be round yeast. 06:34 You wouldn’t know whether they had a capsule because the capsule is transparent. 06:39 So when you put this in a suspension of the india ink, the india ink particles bump up against this transparent capsule and you’re able to see the capsule in relief. 06:52 If you just did a wet mount, you wouldn’t see anything except budding yeast. 06:57 But the india ink brings out the capsule. 07:00 The treatment for cryptococcal meningitis is going to be amphotericin B plus flucytosine for the first 2 weeks, and then fluconazole orally until the cultures have become negative several weeks later. 07:20 Toxoplasma encephalitis is another one. 07:23 And this is generally found in patients with profoundly low CD4 T cell counts. 07:29 And these patients have symptoms of headache, confusion, and lethargy. 07:37 They may present with a seizure in up to 30 percent of the patients. 07:41 So serious manifestations because this essentially produces a space occupying lesion in the brain. 07:49 And so, on exam, you’re gonna have focal neurologic signs in maybe 70 percent of patients. 07:55 And that includes hemiparesis, cranial nerve palsies, ataxia, and sensory deficit. 08:02 And I think you can see from these images that these lesions are not only multiple, but maybe quite large and are common cause of increased intracranial pressure, and possibly even herniation. 08:20 You make the diagnosis by doing a head CT scan or MRI. The MRI is much more sensitive than the CT scan. 08:30 So if you had a positive serology for toxo, it’s really non-specific because a lot of us have a positive serology for toxo. 08:43 But if a patient has these lesions on imaging and their toxo serology is negative, that’s very much against the diagnosis of toxoplasma encephalitis. 08:56 We treat this with pyrimethamine plus sulfadiazine plus folinic acid for at least 6 weeks, and maybe more. 09:06 And the final example of an opportunistic infection I want to present is that of disseminated Mycobacterium avium complex, or MAC infection. 09:16 And these patients too, usually have a CD4 count of less than 50 cells per microliter. 09:25 And the way these patients present. They often present with high fever, marked weight loss, night sweats, abdominal pain, diarrhea. These are very sick patients and they’re often very wasted. 09:39 On exam, they have lymphadenopathy. Most of them have hepatosplenomegaly. 09:45 And because the bone marrow is involved, you’re gonna find severe anemia. 09:51 You’re gonna have an increased alkaline phosphatase. And so, the diagnosis is made primarily by drawing blood cultures. 10:02 And mostly, the blood cultures are going to be found to be positive. Or if you isolate the organism from another normally sterile site. 10:12 This is treated with either clarithromycin or azithromycin, plus ethambutol, plus or minus rifabutin. 10:25 It’s important nowadays to speak to you about the immune reconstitution inflammatory syndrome, otherwise known as IRIS. 10:36 And think about what’s happening. 10:38 We’re giving everybody antiretroviral therapy and some of the patients that we’re treating have opportunistic infections. 10:48 So as their immune system function improves with therapy, they may start attacking the organisms that are causing opportunistic infection. 11:00 And actually, when they were immune-suppressed, they weren’t having as much inflammation. 11:08 Now, we’re providing them with the ability to have inflammation and they’re kind of lighting up these infections as their immune system begins to attack them. 11:18 So what’s happening is, an inflammatory response to the pathogen is triggered by the initiation of antiretroviral therapy. 11:28 We thought we were helping them, but in some cases, we’re actually hurting the patients. 11:33 So let me give you some examples. 11:37 If they had a viral infection and their immune system is coming back, it may worsen. 11:42 If they had a fungal infection, it may worsen. 11:45 Or a bacterial infection like the Mycobacterium avium complex infection we talked about.
About the Lecture
The lecture Human Immunodeficiency Virus (HIV): Signs, Symptoms & Opportunistic Infections by John Fisher, MD is from the course Genital and Sexually Transmitted Infections. It contains the following chapters:
- HIV – Signs/Symptoms
- Opportunistic Infections – Four Examples
- Cryptococcal Meningitis
- Toxoplasma Encephalitis
- Disseminated Mycobacterium Avium Complex Infaction
Included Quiz Questions
Which of the following best describes the common findings in acute retroviral syndrome?
- Fever, lymphadenopathy, sore throat, rash, myalgia/arthralgia, headache
- Cervical, mediastinal, and axillary non-tender lymphadenopathy
- Exudative pharyngitis and hepatosplenomegaly
- Fever, bilateral throbbing headache, blurred vision
- Pneumonia, altered level of consciousness, organ failure
Which of the following is the antibiotic treatment of choice for Pneumocystis jirovecii pneumonia in patients with HIV?
- Trimethoprim-sulfamethoxazole
- Azithromycin
- Clindamycin
- Ceftriaxone
- Levofloxacin
Which of the following types of infection is an AIDS-defining condition?
- Pneumocystis jirovecii pneumonia
- Staphylococcus cellulitis
- Escherichia coli pyelonephritis
- Hepatitis C infection
- Oral candidiasis
What structure does india ink stain allow the observer to see on microscopy?
- Cryptococcal capsules
- Cryptococcal hyphae
- Mycobacteria cell walls
- Toxoplasma nuclei
- Toxoplasma cell walls
Which of the following is the most common method of confirming the diagnosis of disseminated infection caused by mycobacterium avium complex (MAC) in persons with HIV?
- Blood cultures
- Serology
- Abdominal computed tomography scan
- Brain magnetic resonance imaging
- Gram stain
Which of the following refers to paradoxical worsening of a preexisting infectious process following initiation of antiretroviral therapy in a patient with HIV infection?
- Immune reconstitution inflammatory syndrome
- Acute retroviral syndrome
- Acquired immunodeficiency syndrome
- Hyperlactataemia syndrome
- Differentiation syndrome
Which of the following is the imaging modality of choice in the diagnosis of Toxoplasma gondii encephalitis?
- Magnetic resonance imaging
- Compute tomography scan
- Ultrasound
- Thallium single photon emission computed tomography
- positron emission tomography
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I am an RN student, 2nd semester. This lecture is very informative. I like when it describing the opportunistic infection, the lecture provides info from the type of illness, s/s, type of diagnostic tests, and treatments.