Playlist
Show Playlist
Hide Playlist
HIV in Children: Pathology, Clinical Presentation & Diagnosis
-
Slides HIV Pediatrics.pdf
-
Download Lecture Overview
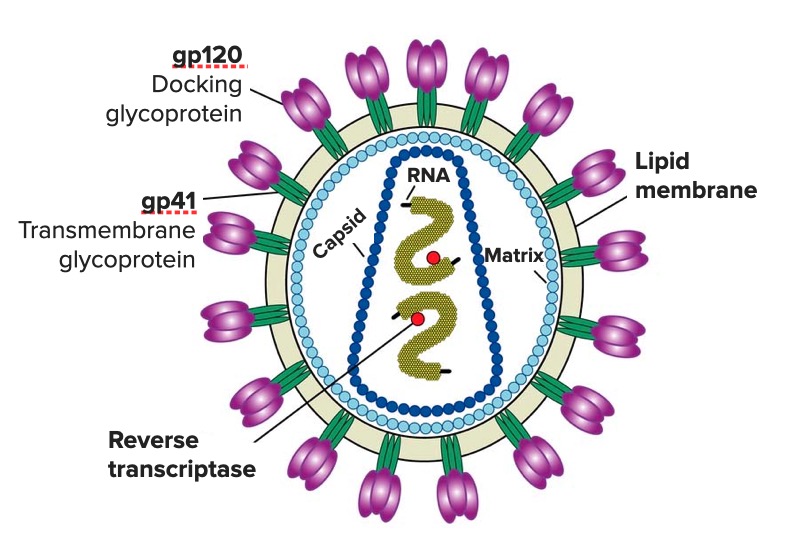
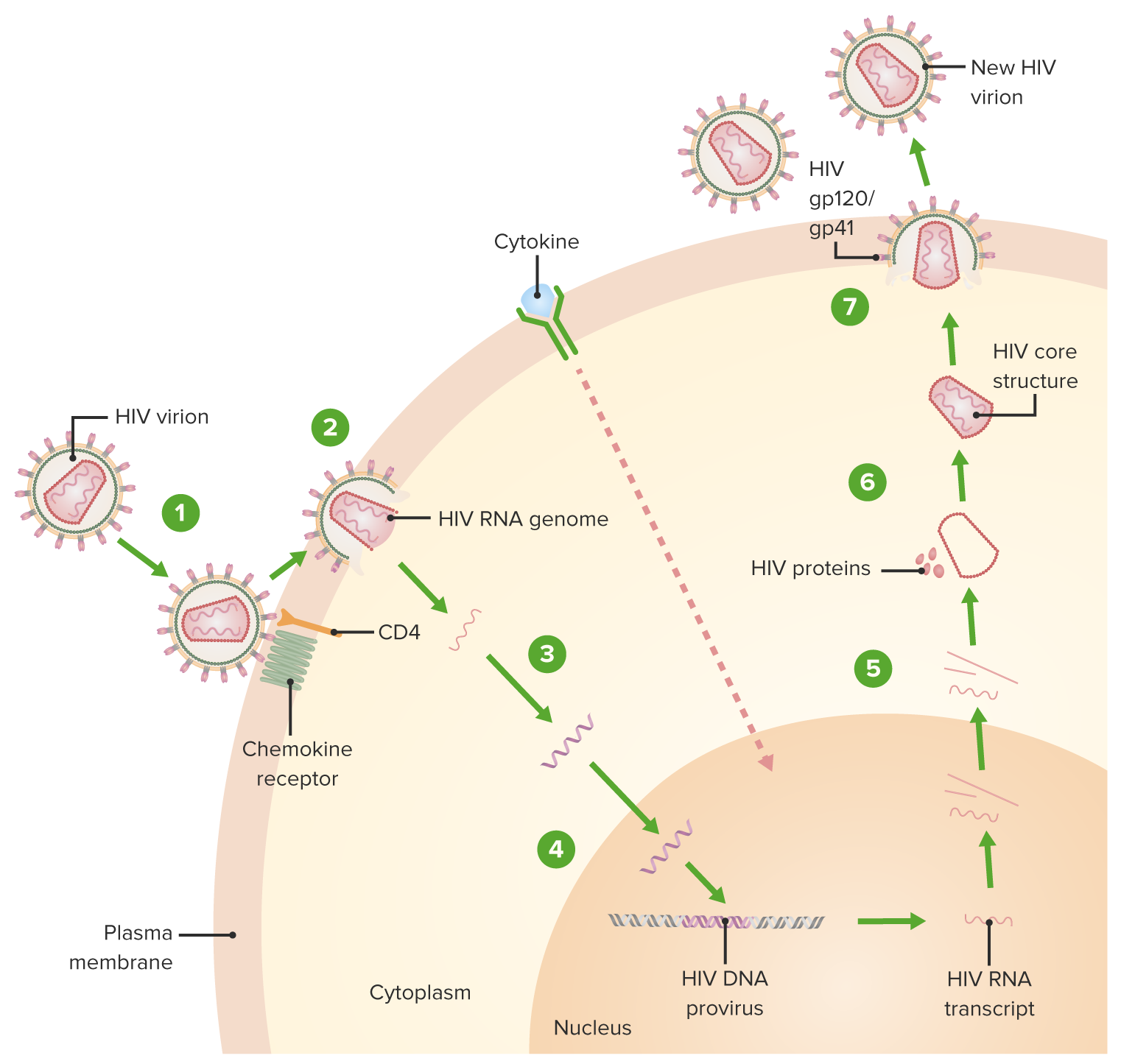
00:00 In this lecture, I’m going to review the basics of HIV or Human Immunodeficiency Virus. So, right now, here’s a map of approximately how many people around the world have HIV. You can see that North America is not at all the most prevalent area where this disease has progressed. 00:21 However, in the United States, we have very comprehensive care for HIV patients, and I’m going to review mostly what happens in the United States about HIV care. So, let’s remember, HIV is a positive single-stranded RNA retrovirus. It primarily affects humans. In pediatrics, we think about 2 main modalities of shedding the virus from 1 person to another. One is vertical transmission. 00:49 It’s important to understand that vertical transmission is a major cause of development of HIV in children. Roughly speaking, if a woman is unaware of her diagnosis, 1 in 4 babies will be transmitted the virus through either in utero experience, through the birth experience, or through breastfeeding. This is to be compared to only 6% of children if we are aware of the mother's status at the time of birth. We can reduce the likelihood of transmission to that baby through immediately placing the child on antiretroviral medications. Flipside, if we’re aware that the mother is HIV positive and we can treat her while she is pregnant, we can reduce that transmission rate to a very low rate of less than 2%, depending on how high her viral load is at the time of delivery. Alternatively, patients can be transmitted the virus through horizontal transmission. 01:46 This is through unprotected sex, sharing drug needles, or somehow sharing blood. In general speaking, 80% of women in the United States right now are receiving this virus who get it through horizontal transmission through unprotected sex. So, we have to remember that women who get HIV, it’s not all because they use IV drugs. In fact, that’s the minority of cases. Also, this is a pediatric problem. A huge percentage of cases in the United States are horizontal transmission in adolescents and young adults. So, remember, for vertical transmission, this is mother-to-infant transmission, it’s generally transplacental, it can be intrapartum, which is by far the most common, or it can be via breastfeeding. For horizontal transmission, it is through penetrative vaginal or rectal sex without a barrier method and can be transmitted also by needle sharing or through blood sharing. Who is at increased risk? Well, adolescents are. That is because they tend to have unprotected sex, IV drug use is reasonably high in this population, and it’s also an increased risk among men who have sex with men. So, infants with HIV are generally much more rapid in terms of the rates at which they acquire final end-stage AIDS and tend to have a more severe disease than in adults. So, this is generally true. An infant with HIV who has acquired it during the birth process and the practitioners are unaware of the diagnosis, will get very sick very quickly. This is different from adults where there is a long period during which the virus is growing inside the body, but the patient is relatively asymptomatic. There are different types of responses to the HIV virus. Unlike in adults, the vast majority of children, 85%, are rapid progressors. This means they go from the initial inoculation of the virus to HIV and end-stage AIDS much quicker than in adults. These patients present with opportunistic infections like pneumocystis. They may present with failure to thrive. The increased metabolic demands of fighting off the HIV virus mean that they have a harder time spending their energy actually growing. Oftentimes, infants will progress to an encephalopathy and they can do that by 4 months without any treatment. And, usually infants who are untreated will die by the age of 2 to 4 years, which is a much faster progression than in adults. A small percentage of infants will be slow progressors. This is about 15%. For these children, the mean onset of symptoms is around 6 years of age and they often can live into adolescents without treatment. I am not listing it here, but there is a very tiny progression of children who we would call non-progressors. These infants have the virus but do not get a low CD4 count and generally are symptom-free. So, let's look at the difference between HIV in infants and in adolescents. In infants, they present with poor weight gain, developmental delay, severe thrush, and bacterial infections. In adolescents, they may be asymptomatic until their CD4 count falls. 50% of them will have a primary infection at the time of acquiring the virus. This is sort of like a flu-like illness. These patients may have candidal infections, which is unusual after 1 year of age in a healthy infant, and they often present also with bacterial infections. Here is the graph of how we think of adults who are acquiring this HIV virus. Let’s follow the red line first. This is the number of viral RNA copies on a quantitative PCR. You can see these patients will start off after acquiring the virus and have a rapid spike in the amount of virus that’s present. The immune system is able to somehow corral this viral load down and they'll have a prolonged period, virtually years, when they have a low level of viremia. Then, as their immune system losses the ability to fight the virus any longer, it spikes up. Meanwhile, when we count up their CD4 positive T-cells, which are one of the victims of viral invasion; likewise, with that initial rise in virus, there is initial drop in the number of CD4 cells. This then goes up a little bit and then there is a lifelong low CD4 count, which gradually eventually comes down below about 200 and that's about when patients start developing symptoms of end-stage AIDS. HIV will present usually through evidence of opportunistic infections. So if you see an infection such as <i>Pneumocystis jiroveci</i>, you should be concerned that this is possibly HIV. A rapid viral test is cheap and extremely accurate. We should be using these more and routinely in adolescents who present for care. Because so many adolescents in the United States do not have primary care providers or have providers but do not feel like disclosing sexual activity or drug use activity with those providers, it's important that at all phases of health care including the ER and the hospital setting, we routinely do rapid viral testing. Another test opportunity is the ELISA test. This is becoming less common now because the viral testing that’s rapid is so cheap and effective. However, regardless of what kind of test we do, we usually do followup testing that is now the PCR. We are not going to the Western Blot so often. Remember, false positive rapid testing and ELISA in infants under 18 months of age happens. This is because if the mother has the disease, her antibodies against HIV are going transplacentally and that child will have those antibodies for up to 18 months persisting in their blood. That doesn't mean they necessarily have the virus. So, diagnosing HIV in a newborn may be a bit tricky because the rapid viral testing is difficult. We can do quantitative PCR and that will help answer that question. There are other lab findings in acute HIV infection. A CBC may show leukopenia, lymphopenia, anemia, or thrombocytopenia. These all happen in HIV. Additionally, patients may develop proteinuria from an HIV nephritis. That is usually a little bit later on. 08:51 Patients may also have elevated ALT and AST.
About the Lecture
The lecture HIV in Children: Pathology, Clinical Presentation & Diagnosis by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of HIV
- Clinical Presentation of HIV
- Diagnosis of HIV
Included Quiz Questions
Which of the following statements is TRUE about infants with HIV?
- They tend to have more rapidly progressing and more severe disease.
- They rarely present with opportunistic infections.
- They rarely present with failure to thrive.
- Encephalopathy in untreated patients typically occurs around 4 years of age.
- It may be fatal in untreated patients by the age of 15.
Which of the following populations are NOT at high risk for HIV transmission in the USA?
- Children who undergo a blood transfusion
- Adolescents with multiple sexual partners
- Adolescents who have unprotected sex
- IV drug abusers
- Men who have sex with men
Which of the following is an example of horizontal transmission?
- Rectal intercourse
- Transplacental
- Intrapartum
- Via breastfeeding
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very comprehensive. I particularly liked the differences between adult and pediatric presentations, also the different courses of the disease.