Playlist
Show Playlist
Hide Playlist
Hereditary and Acquired Hypercoagulable States
-
Slides Bleeding Disorders and Thrombotic Disorders.pdf
-
Download Lecture Overview
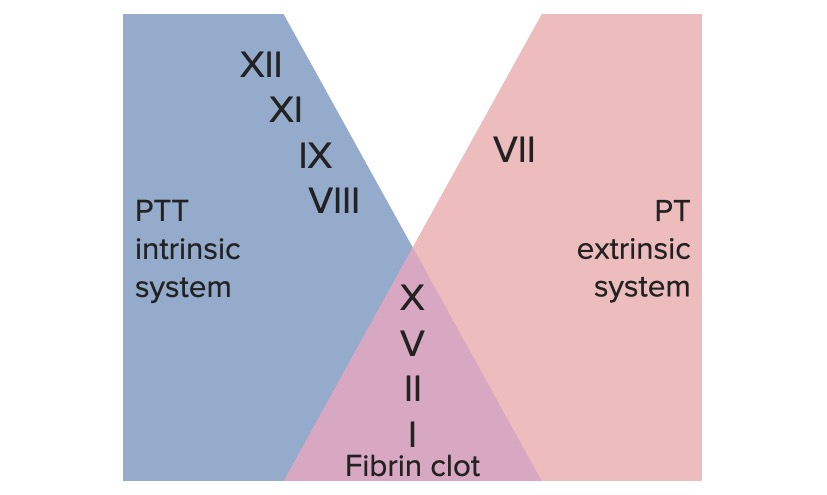
00:01 Let's talk about some hereditary hypercoagulable states. 00:05 In a previous session, we talked about hereditary anticoagulation states or things that led to greater bleeding. 00:13 In this case, we're talking about things that drive more extensive coagulation. 00:18 So shown immediately on the left-hand side, are deficiencies in antithrombin III. 00:23 Recall that, antithrombin III synthesized in the liver, but activated by heparin-like molecules made by the endothelium, are going to be important for regulating and turning down the activity of factors XII, XI, IX, X, and IIa or thrombin. 00:41 So they're all going to be very important, if you don't make adequate antithrombin III, that can because of hypercoagulability. 00:50 Recall also, that, protein C and and protein S, are part of the pathway driven by thrombin, that will regulate the activity of factor VIIIa and if you don't make enough protein C or protein S, again, synthesized by the liver, then you will not regulate that step and you can have, a more hypercoagulable state, you're not turning off the coagulation cascade. 01:17 There's another factor, factor V, that normally interacts with factor VIIa, and that will drive the coagulation cascade and we normally turn that off, using the activation of protein C and protein S. 01:34 There is a form of factor V, that is a mutant form, that is called factor V Leiden, because it was discovered in in Leiden of Netherlands, and got its name that way. 01:45 And factor V Leiden, cannot be inactivated by protein C and protein S activity. 01:52 So, once it gets turned on, it just keeps happily driving, the procoagulation pathway. 02:00 And you can have too much prothrombin, so, a single nucleotide mutation a G to A mutation, in the upstream promoter sequence for the prothrombin gene, can lead to too much prothrombin generation. 02:16 With too much prothrombin, you're actually going to be overall more procoagulant. 02:22 So, the various hypercoagulable states. 02:24 Factor V Leiden, the one discovered in the Netherlands, the mutant factor V, cannot be inactivated by protein C and protein S and 5% of the Caucasian population are heterozygous for this, it turns out that about 20% of the people walking around in the world, who are hereditarily hypercoagulable, have factor V Leiden mutations. 02:47 You can have too much homocysteine, so, hyperhomocysteinemia is a metabolic pathway defect, that leads to endothelial dysfunction, also causes atherosclerosis and has been assigned to perhaps 10 to 25%, of hypercoagulable states in the total human population. 03:08 That mutation from guanine to adenosine in the 20210 sequence, in the prothrombin promoter gene, will drive overproduction of factor II and about 6% of the human population, probably is hypercoagulable on that basis, 2% of the Caucasian population are heterozygous. 03:29 Protein C and protein S deficiencies, these are responsible for inactivating both factor V and factor VIII. 03:36 So, mutants in these have increased, as a consequence, factor V and factor VIII activity and about 4-5% of venous thromboembolisms, VTE, are attributed to defects in those proteins. 03:50 And you can have antithrombin III deficiency, you're not making enough of antithrombin III and a mutation or a deficit in that protein, will lead to excessive activity of II, IX, X, XI, and XII. 04:06 Now, if you're adding up all the percentages, that lead to hypercoagulable states in human population, we're only getting up to maybe 50%. 04:17 So that says that, 50%, of the people who have hereditarily hypercoagulable states, we don't know why. 04:25 So, there are genes, there are proteins, there are regulatory pathways yet to be discovered, that's up to you. 04:35 Acquired hypercoagulable states, so, we were just talking about those that you could get, by virtue of being in the gene pool, what about ones that are occurring because of things that you acquire? So, cancer, is very much a driver of hypercoagulable states. 04:49 Cancer cells make mucin, which is procoagulant, they do crank out excess tissue factor, which is going to drive the extrinsic pathway and that cell-free DNA that's what cfDNA stands for, is a negatively charged molecule, that is going to be something that promotes the intrinsic pathway. 05:06 So, there are a number of things that cancer cells make, just as part of their doing business in the world, that will make patients, who have systemic cancer, much more coagulable. 05:18 Smoking, probably by impacting the production of coagulant and anticoagulant factors, also, by affecting endothelial cell function, has an impact on coagulability. 05:30 Pregnancy and other hyperestrogenic states, will drive increased production of procoagulant factors. 05:38 If you are immobile, you're sitting in coach class on that transatlantic plane flight, to Germany and you don't get up and walk around, you can develop deep venous thrombosis, just because you are having stasis, in your lower extremities. 05:53 Postoperative states, by having endothelial injury and inactivity can also drive hypercoagulable states. 06:01 Trauma, travel greater than four hours and obesity, all will contribute to a hypercoagulable state an acquired hypercoagulable state. 06:11 Nephrotic syndrome, interestingly enough, as you lose proteins, by having a defective membrane, at the in the glomeruli, you will lose antithrombin III somewhat preferentially. 06:24 Lower levels of antithrombin III, will then allow a lot of factors in the intrinsic pathway, to be not regulated appropriately. 06:33 Essential thrombocythemia, so this is too many platelets, we talked about this early on, 30% of patients who have essential thrombocythemia, have a Janus Kinase II mutation and drive the constituent production of platelets. 06:49 That will give you a high platelet count and greater than about 400,000, you can start having a hypercoagulable state. 06:56 And then finally anti-phospholipid antibody. 06:59 This can be part and parcel of a variety of autoimmune diseases, including systemic lupus erythematosus. 07:05 In this setting, you develop antibodies, not so much to phospholipid, but to proteins that interact with phospholipids, that are present on the surface of endothelial cells, platelets and other cells, that are engaged with the circulation and you can end up with arterial or venous thrombosis in that setting. 07:26 And 5-15% of veno thromboembolism, is attributed to anti-phospholipid antibody. 07:34 So, those are our required hypercoagulable states, with that we've talked about various ways, that you can get too much thrombosis.
About the Lecture
The lecture Hereditary and Acquired Hypercoagulable States by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
How does hyperhomocysteinemia cause hypercoagulability?
- It causes endothelial dysfunction.
- It causes overproduction of factor II.
- It inactivates factors V/VIII.
- It leads to excessive II, IX, X, XI, and XII activity.
- It produces cell-free DNA (cfDNA).
What percentage of hypercoagulable states have unknown causes?
- 50%
- 25%
- 75%
- 10%
- 60%
Nephrotic syndrome results in the loss of which factor in the urine?
- Antithrombin III
- Tissue factor
- Factor V
- Factor XII
- Factor VII
Prolonged sitting for several hours is a risk factor for what condition?
- Deep vein thrombosis
- Septic shock
- DIC
- Nephrotic syndrome
- Hyperhomocysteinemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |