Playlist
Show Playlist
Hide Playlist
Hemorrhoids
-
Slides GIP Hemorrhoids.pdf
-
Download Lecture Overview
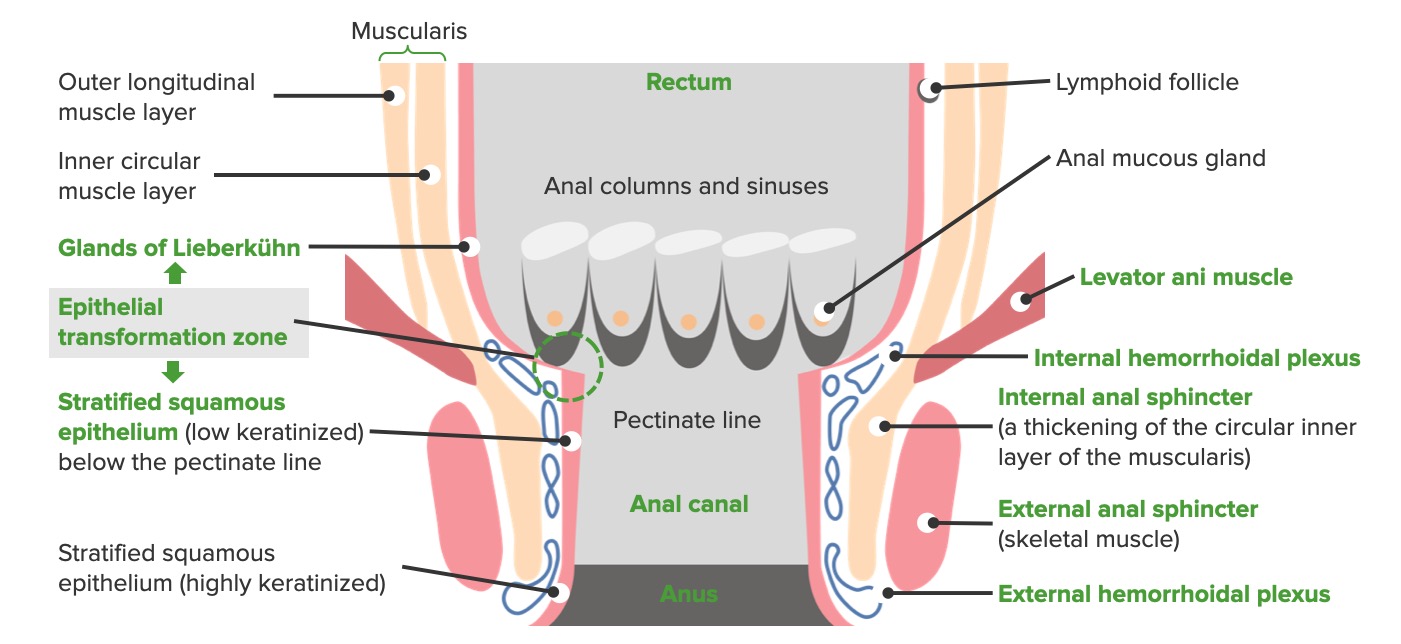
00:01 Welcome. In this talk, we're going to cover a very common malady that involves the GI tract, that is to say, hemorrhoids. 00:09 Hemorrhoids are simply dilated vascular structures in the anal rectal canal and they may be internal or external and they will have slightly different symptomatic presentations but it's all the same process and all the same complications. 00:25 The epidemiology of this is that it's really common. You will certainly encounter it in your patients. 00:31 You may encounter it in yourself, particularly, as you get older. Although there is no known sex predilection, because of the association with pregnancy, an increased intraabdominal pressures associated with carrying an infant to term, women do have a significant risk of developing hemorrhoids. 00:51 So, basically, it is a decreased venous return. 00:54 There's an obstruction, whether it's mechanical or functional, there is an imposition on the venous return. 01:04 This can happen as a result of straining recurrently during defecation, so, just increasing pressures in that way. 01:12 There's the pregnancy-related anatomical compression which I have already explained. 01:16 And then, the reason that this probably occurs in more older individuals is that there's a weakening of the pelvic support structures so that there can be dilation of the venous return. 01:29 Clearly, also, portal hypertension with portal systemic anastomosis with anorectal varices will be associated with hemorrhoids. 01:42 Other risk factors, so, many of these kind of fall in line with what we've already talked about, chronic diarrhea, constipation, colonic malignancy by causing a proximal obstruction. 01:52 Inflammatory bowel disease by causing increased inflammation, obesity, things that impact the ability to defecate, spinal cord injury, rectal surgery, previous episiotomy. 02:05 So, there've been an interruption associated with the birth of a baby and a cut and you can compromise with healing subsequent venous return and anal intercourse is also associated with hemorrhoids. 02:21 The pathophysiology is actually reasonably straightforward as I've already said. 02:24 It's a mechanical or a functional obstruction to venous return. 02:28 We're looking here at the internal veins and the external hemorrhoidal veins. 02:33 These are above, internal or below, external, the pectinate or dentate line. 02:41 The normal blood flow from this area is from distal to proximal, obviously, and there's usually a nice collection of blood through the postcapillary venules that accumulate into a vein. 02:55 And to keep things moving in one direction, there are valves. 02:59 And those valves, if competent, allow blood to go up and then, not to regurgitate. 03:06 However, with increased pressures from all the things that we talked about, we can cause dilation of that segment of the vein and then, we have an incompetent valve that prolapses. 03:18 And now, we have an increased propensity to have stasis of the blood and dilation of the vein, more distal to the damaged valve and that will lead to varicose veins which will be then manifest as hemorrhoids. 03:36 External hemorrhoids are covered by a squamous epithelium and there are going to be pain receptors in that like most stratified squamous epithelium throughout the body. 03:48 So, the pudendal nerve, sacral plexus will all have afferent pain inputs from this area. 03:56 So, when the skin gets distended, as the veins distend, they distend the skin and there will be pain. 04:02 So, external hemorrhoids are typically quite painful. 04:04 On the other hand, the internal hemorrhoids do not have a somatic sensory innervation and they're usually painless unless they prolapse. And then, you can have secondary inflammation. 04:15 The clinical presentation, so, a trigger warning, this is not a pretty picture. 04:19 But this is an external hemorrhoid, typically associated with painful rectal bleeding with bowel movements. 04:28 Clearly, the epithelium over the surface of these dilated veins is very thin. 04:33 It takes very little to erode it. And then, you can get bleeding. 04:37 So, you'll typically see hematochezia, bright red blood in the stool. 04:41 There may be a very painful perianal mass described by the patient or elicited by you on physical exam. 04:49 And then, so called irritated skin tags, heaped up areas of epithelium that overlie an external hemorrhoid. 04:57 Internal hemorrhoids as I said are usually painless. 04:59 You do get bright red blood associated with bowel movements and what's being shown here is a prolapse internal hemorrhoid. 05:07 So, this is coming from above the pectinate line and prolapsing as the veins becoming bigger and bigger and bigger. 05:14 Because this is now over lined by typical epithelium that lines the GI tract, so, a columnar epithelium making mucus, there will be mucus discharge. 05:25 There may be itching. That's a secondary manifestation of inflammation. 05:29 Because of the kind of distention of the bowel or of the anus by these prolapsed vessels, you may actually have fecal incontinence. 05:41 You may not be able to squeeze the anal sphincter appropriately, so, there may be leakage. 05:46 How do we make the diagnosis? Well, it's not a hard diagnosis, and even now, you as a first or second year medical student, you can do this. 05:54 It's a physical exam, so, we're looking for fissures. 05:56 We're looking for inflammation of the skin, dermatitis, skin tags indicating that we have heaped up regions of epithelium and you may even have a palpable thrombosis of these hemorrhoids, so, you can actually feel what feels like a hard core. 06:13 That's a thrombosed hemorrhoid. Signs of infection or abscesses, much more redness, like, kind of a fluctuant mass so that there's a larger area of necrotic debris. 06:25 With prolapse, you'll actually see these bluish veins extending into the external space, around the anus. 06:34 And then, internal hemorrhoids, you put on a glove finger, you may be able to feel those, especially, when they're thrombosed. 06:41 The formal diagnosis may be made on external exam just as described there. 06:46 But for internal hemorrhoid sigmoidoscopy or colonoscopy but mostly, sigmoidoscopy is going to be indicated. 06:55 How do you manage this? So, you want to reduce the amount of pressure that is causing the expansion of these veins. In general, they're very common. 07:06 We said four percent of the population overall will have these. 07:10 So, you don't usually - you don't treat everyone with hemorrhoids but you treat the ones who are symptomatic, who have pain or bleeding. 07:16 You can try to make the stool softer and it's easier to do with either laxatives or increased fiber. 07:24 Warm baths will relax the anal sphincter and therefore, reduce the venous pressures. 07:30 And also, it just feels good for the patient. For vessels that are very prominent and/or bleeding, you may do electrocoagulation, literally, zap them and obliterate them. 07:42 And then, for those that are refractory to all those other administrations, then, you would do surgery and resect them. 07:51 And with that, we've come to the end of hemorrhoids.
About the Lecture
The lecture Hemorrhoids by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What defines a hemorrhoid?
- Dilated vascular structure in the anorectal canal
- Constricted vascular structure in the anorectal canal
- Dilated nerve in the anorectal canal
- Atrophied muscular structure in the anorectal canal
- Hyperplastic muscular structure in the anorectal canal
What are the risk factors for hemorrhoids? Select all that apply.
- Straining during defecation
- Pregnancy-related anatomical compression
- Age-related weakening of pelvic support structures
- Orthostatic hypotension
- Scleroderma
Which statement regarding hemorrhoids is correct?
- External hemorrhoids are painful due to somatic pain receptors.
- Internal hemorrhoids are painful due to somatic pain receptors.
- Internal hemorrhoids are painful due to autonomic pain receptors.
- External hemorrhoids are painful due to autonomic pain receptors.
- Neither external nor internal hemorrhoids are painful.
What is required for the diagnosis of hemorrhoids?
- Physical examination
- CT scan with IV contrast
- CT scan without IV contrast
- MRI
- CBC and CMP
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |