Playlist
Show Playlist
Hide Playlist
Heart Failure: Treatment
-
Slides HeartFailure ChronicCare.pdf
-
Download Lecture Overview
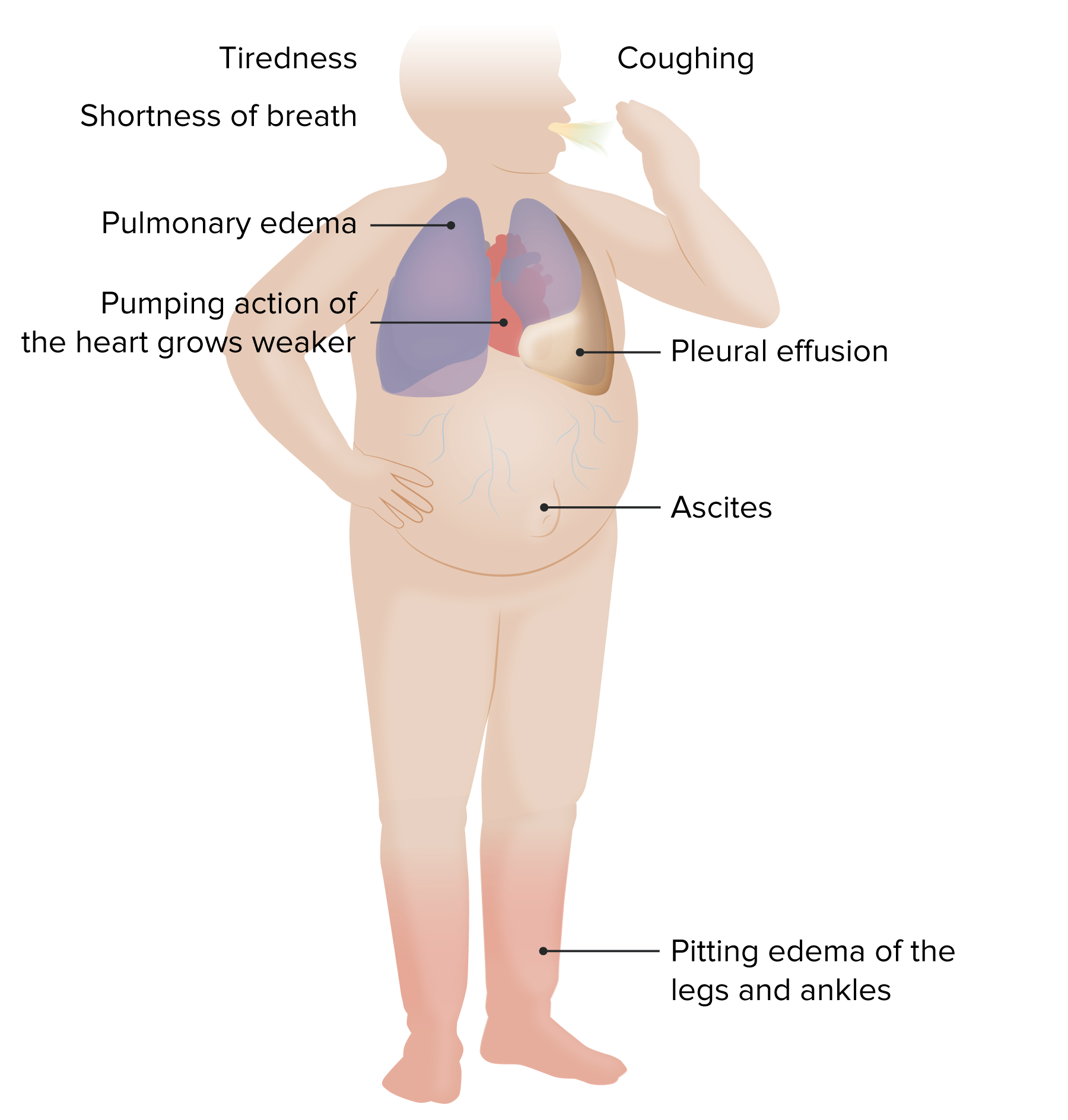
00:00 Let’s talk about treatment for our patient. 00:03 He is currently – if you remember, he was New York Heart Association class III, so significant symptoms, reduced ejection fraction heart failure. 00:11 He’s taking a furosemide 40 mg daily, lisinopril 20 mg daily, and he doesn't have any contraindications to other heart failure treatment. 00:20 So, what is the best choice for the next drug to add to improve this patient's risk of heart failure complications and mortality as well? Is it metoprolol XL, sacubitril/valsartan, spironolactone, or isosorbide dinitrate with hydralazine. 00:37 Metoprolol XL, beta blockers, ACE inhibitors, foundational drugs for heart failure and I will go over that in depth. 00:45 All right. 00:46 So, when we think about treating heart failure, a lot of times we have to think about using diuretics. 00:52 For this gentleman, with his symptoms and his edema, he’s going to – he’s already on Lasix. 00:57 He needs to stay on a diuretic, so that's just to treat symptoms and signs. 01:02 That doesn't necessarily have an effect on mortality, in particular. 01:08 Something else, if it’s left ventricular ejection fraction, it remains below 35% despite having them on OMT, or optimized medical therapy. 01:17 Or if he has a history of significant arrhythmia, he needs an implanted defibrillator. 01:23 Okay. 01:24 So, those span the distance for treatments. 01:27 So, that’s always a consideration no matter where your patient stands. 01:30 These are recommendations from the European Society for Cardiology, but they stand up. 01:35 They make sense in clinical practice. 01:38 Do remember that ACE inhibitors or angiotensin receptor blockers because they work about the same among patients with heart failure, it’s just that the ARBs are associated with less cough than an ACE inhibitor. 01:52 That drug, along with beta blockers, are your foundational drugs and they work most effectively for when they’re increased to at least moderate doses, up to high doses. 02:03 We’re talking about lisinopril 40 mg, benazepril 40 mg, we’re talking about beta blockers such as carvedilol 25 mg twice daily, or metoprolol XL up to 200 mg daily. 02:16 And they also work most effectively for patients with more severe heart failure. 02:21 So, the more severe their symptoms are, the worse their ejection fraction, the more likely they're going to get a benefit with these drugs. 02:29 So, really try to get them on board. 02:30 The challenge is just managing so many different drugs in patients who are usually a little more frail with, say, chronic kidney disease and diabetes and hypertension. 02:41 Now, with those foundational drugs, if the patient is still symptomatic and still has a low ejection fraction, next one to add is probably a mineralocorticoid receptor antagonist. 02:52 A drug like spironolactone is the most commonly used. 02:55 That also reduces mortality outcomes in heart failure. 03:00 If they're doing fine at that point, at any point, stop the polypharmacy and you don't need to add more drugs because, usually, when I diagnose somebody new with heart failure, it's an automatic prescription for at least four to five drugs. 03:14 What would those be? ACE inhibitor, beta blocker and, because of comorbid conditions, oftentimes they’ll need an aspirin and they’ll need a statin. 03:23 I’d be surprised if they don’t have diabetes or hypertension. 03:25 So, there's probably three or four more drugs they’re going to be getting, and that's a lot of burden for the patient to take all those drugs every day and follow-up for potential side effects and go to a lab, it's a lot of work. 03:39 So, while these are all good agents and really improve heart failure outcomes, do keep patient burden in mind as you go through. 03:47 And that's why it’s nice to use this algorithm because it adds drugs on as they’re needed. 03:52 Say, the patient is now on three drugs for heart failure, still symptomatic. 03:57 Well, now you’ve got some options in front of you. 03:59 They might qualify for cardiac resynchronization therapy if they have this wide QRS. 04:07 Instead of using an ACE or an ARB for these patients, it may be time to consider switching to a brand-new kid on the block, the angiotensin receptor neprilysin inhibitor. 04:19 And there's only one of those available right now, sacubitril/valsartan. 04:23 But in the PARADIGM-HF trial, replacing enalapril with sacubitril/valsartan was associated with better outcomes for hospitalization and for mortality – both overall mortality and cardiovascular mortality. 04:36 So, that could be a good option for patients and doesn't add to the patient burden. 04:41 On the other hand, if they really have an elevated heart rate despite that heavy dose of beta blocker, you can add a drug like ivabradine, which has also been associated to help particularly with heart failure hospitalization. 04:54 However, I would caution – for those patients who have a pulse of 80 and they're taking a beta blocker, really look as to whether the patient is actually using their beta blocker because it's hard to get a pulse that high with a moderate to high dose of a beta blocker. 05:13 Usually, it's the opposite and their pulse rate is more like 52. 05:18 So, you can combine those treatments. 05:21 But if there are resistant symptoms, you’re definitely involving a cardiologist at this point. 05:26 You could think about things like isosorbide dinitrate hydralazine, digoxin or even heart transplantation. 05:32 But I think the main thing for USMLE is that centerpiece of what are the foundational drugs, ACE inhibitors or ARBs, beta blockers and then a drug like spironolactone. 05:42 Those are really the three key ones to get on board. 05:47 All right. 05:48 So, what we talked about was some of the keys to diagnosis of heart failure and a lot about the management of heart failure. 05:54 Hopefully, it was really helpful and that algorithm is something that you can use over time. 05:58 Thanks.
About the Lecture
The lecture Heart Failure: Treatment by Charles Vega, MD is from the course Chronic Care.
Included Quiz Questions
Diuretic treatment in heart failure is primarily to reduce which of the following?
- Volume overload
- Mortality
- Risk of myocardial infarction
- Rate of cardiac remodeling
- Risk of arrhythmias
What is the most appropriate management in a patient with severe heart failure who has experienced sustained ventricular tachycardia despite optimal medical therapy?
- Implanted cardioverter defibrillator
- Palliative care
- Bed restriction
- Intravenous loop diuretics
Which of the following is an angiotensin receptor-neprilysin inhibitor?
- Sacubitril/valsartan
- Quinapril
- Cilazapril
- Enalapril
- Valsartan
Which of the following medications are typically given to most patients with heart failure with reduced ejection fraction?
- Angiotensin system blockers, beta-blockers, diuretics
- Angiotensin system blockers, calcium channel blockers, diuretics
- Angiotensin system blockers, beta-blockers, calcium channel blockers
- Beta-blockers, calcium channel blockers, diuretics
- Angiotensin system blockers, beta-blockers, calcium channel blockers, diuretics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |