Playlist
Show Playlist
Hide Playlist
Hand and Wrist Pain
-
Slides HandandWristPain AcuteCare.pdf
-
Download Lecture Overview
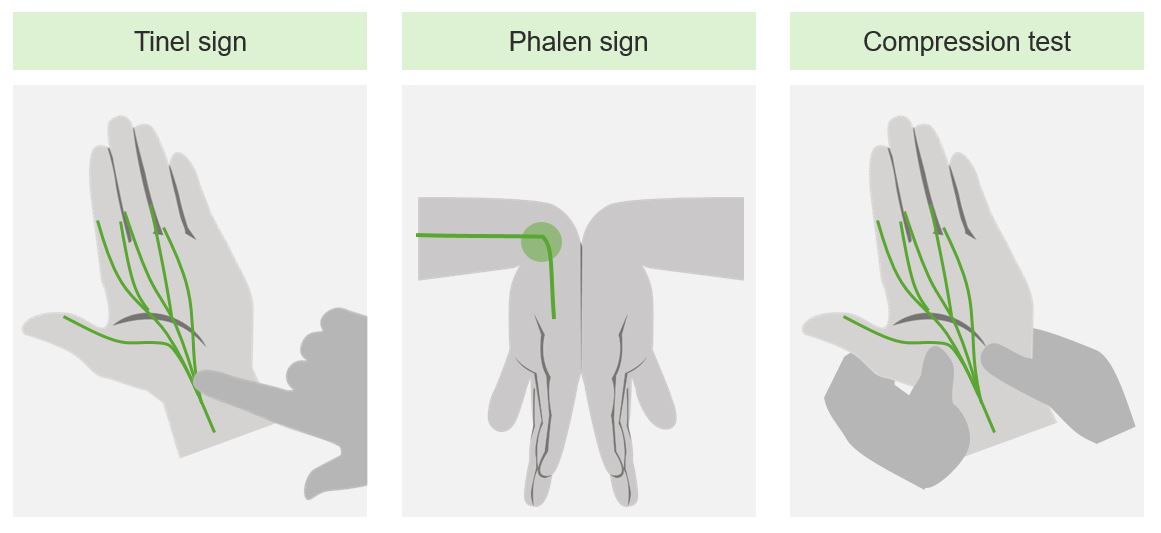
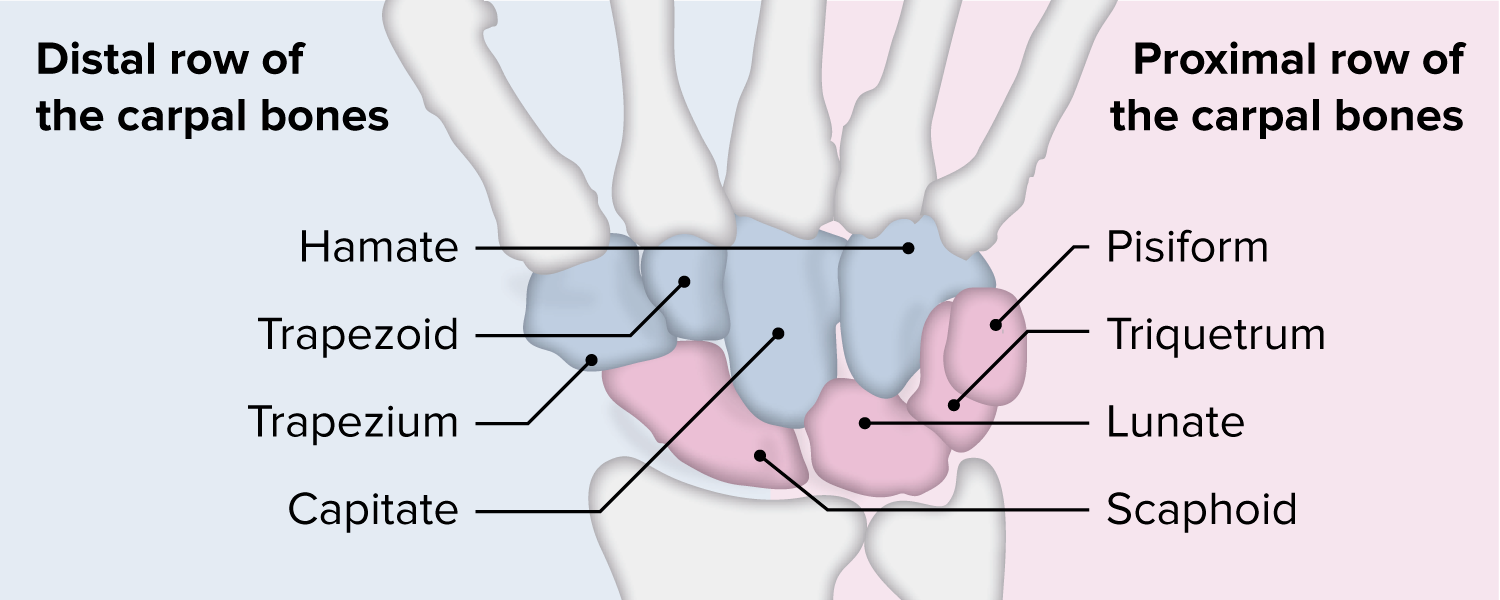
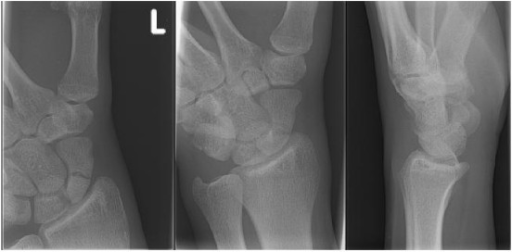
00:01 Ouch. 00:03 Let’s talk about pain of the hand and wrist. 00:05 All right, here we go. 00:07 We’re going to talk about how to distinguish different types of wrist pain, and so – and hand pain. 00:11 So, therefore, we’re going to start with our differential diagnosis. 00:15 The main cause of hand and wrist pain that include osteoarthritis, rheumatoid arthritis, tendinopathies, of which there are several, acute injuries, fractures and sprains, and overuse injuries. 00:26 And we’re going to highlight, I think, one of the most important for you to understand, the ones that can be a little bit difficult to discriminate, and what of course maybe on USMLE exam as we go through. 00:37 So, physical examination, inspection is where you start looking for any gross deformities, looking for swelling, range of motion. 00:46 Especially when you’re talking about range of motion of the fingers, you can easily identify tendon rupture with the inability to either extend or flex the fingers. 00:56 We’ll talk about some provocative tests, such as Finkelstein's that you can use for specific conditions, and then a neurovascular exam is almost always indicated just checking for sensation to light touch at least, if not two-point discrimination, and making sure that capillary refill and the radial pulses are strong. 01:13 And the reason to pay attention in a special way to the anatomic snuffbox is the risk of a scaphoid fracture. 01:19 Now, scaphoid is the most common fractured carpal bone and it's a very common mechanism. 01:25 Fall on to an outstretched hand. 01:27 And you can see in the image there, a fracture of the scaphoid bone. 01:31 It's right through the body of the bone in this. 01:34 So, really you’re going to pay attention to this anatomic snuffbox which is illustrated right here. 01:40 That's the snuffbox. 01:41 Tenderness in this area after a fall makes you have to consider a scaphoid fracture. 01:46 So, in addition to your normal anterior, posterior and lateral views of the wrist, you’re going to want to include a navicular view to help give a special image of that bone. 01:56 And the important thing to understand about scaphoid fractures is that there's a high risk of non-union and there is also a higher risk of avascular necrosis. 02:05 So, this can be a common injury and usually something that heals fairly well with the right treatment into something that's a lot more serious and chronic over time. 02:15 So, it's important to always immobilize the thumb. 02:18 So, when you're unsure as to whether the patient has a fracture or not, make sure they get not just a wrist splint, but a thumb spica splint as well. 02:28 That's going to protect that scaphoid bone from suffering avascular necrosis. 02:32 And because the initial radiographs can be negative, in a decent proportion of patients with a scaphoid fracture, repeat radiographs are necessary for two weeks. 02:42 If after they’ve been in the splint for two weeks and their x-ray is still negative, there is not going to be a fracture there and then they’re safe to begin range of motion exercises and go through physical therapy. 02:53 A lot of times the patients are going to feel a lot better at that point anyway, two weeks after their injury. 02:59 So, that's high-yield stuff. 03:01 The other thing about the snuffbox is that it is an area for De Quervain's tenosynovitis. 03:06 This is a radial pain that's just limited to that first extensor compartment. 03:12 Patients often have a history of overuse, but not always. 03:17 Sometimes, it just arises from nowhere. 03:21 And the pathology is an inflammation of the extensor pollicis brevis and abductor pollicis longus tendons as well. 03:29 The important thing to know I think for your exam, and also clinically, with this condition, there is a very specific exam for it. 03:37 So, thumb is tucked in here under your second finger and then it’s just a ulnar flexion, and that pulls on those endons and should hurt. 03:47 And sometimes, it really hurts patients. 03:49 And so, pain over the anatomic snuffbox with this maneuver, it’s De Quervain's tenosynovitis, and that's called Finkelstein's test. 03:57 It has a good sensitivity and specificity overall. 04:01 So, the treatment for De Quervain's tenosynovitis, splinting can be helpful. 04:06 I find in my practice a lot of patients don't like to use it because it limits the rest of their function, and especially if they are at work or they are taking care of their kids, they want their hands free. 04:17 Rest, of course, if there's something that's an overuse injury that’s promoting the tenosynovitis, but this is one of those types of conditions they can actually go right to injection. 04:27 Injecting a little bit of corticosteroid, along with lidocaine, right along the tendon sheath can be curative for many patients. 04:34 They can become recurrent. 04:36 Once you have one episode of De Quervain's, you’re much more likely to have another. 04:40 But if it's four to six months later, repeating the injection is a reasonable option for those patients. 04:47 Another common wrist and hand disorder, carpal tunnel syndrome. 04:52 This slide just reviews the distribution of the median nerve, which is the one that's affected. 04:57 So, in the palmar surface, it really includes these three fingers right here plus part – the middle part of this fourth digit, but really it can at times involve the whole hand. 05:11 And if it’s more severe, it can involve not just sensory symptoms, but motors symptoms as well. 05:16 It does not involve the dorsum of the hand, though. 05:18 It’s really the palmar surface that's affected – or ventral surface that’s affected. 05:22 There is a distribution in green that you can expect, but I have seen cases that also involve the entire fourth digit. 05:29 And as I mentioned, there can be a motor component to it as well. 05:34 So, things that we look for is tapping over the medial wrist here, medially like so, and that’s called Tinel sign. 05:45 Holding the wrists in that position like this for 30 seconds and for reproduction of the symptoms and then a direct impression of both sides of the carpal tunnel simultaneously can elicit symptoms as well. 05:59 Just to describe the prevalence, it's really common, 3 to 6% of adults. 06:03 And you can also see it outside that median nerve distribution. 06:07 So, be aware of that. 06:09 These patients often have decreased two-point discrimination. 06:12 That’s where that test can be particularly helpful. 06:15 Thumb abduction, in particular, may be reduced among patients with carpal tunnel syndrome. 06:22 And then if you have those things, there is not much reason to add Tinels and Phalens because they’re not really going to add a lot, but I always do Tinel and Phalen maneuvers on patients with CTS. 06:33 And that might come up in your exam, something along the lines of, you have a patient with wrist pain, they put their wrist together, what do you think the diagnosis – and it reproduces the symptoms, what do you think the diagnosis is? Carpal tunnel syndrome. 06:47 All right. 06:47 So, ways to treat carpal tunnel. 06:50 First of all, you have to address overuse. 06:53 This is a real problem for my patients who use their hands and wrist repetitively and that’s part of their job. 06:59 Can be difficult. 07:00 Splinting, using it for a limited amount of time. 07:05 I like to use it mostly at night. 07:07 And the reason is that I don't want that wrist to freeze up. 07:10 Again, the wrist has a lot of range of motion to it. 07:13 You want to preserve that range of motion, but also give it some time to rest. 07:16 That's why I splint at night. 07:17 Works for a lot of people. 07:18 Adherence is much better than during the day. 07:20 You can use oral corticosteroids for the short-term for very severe cases. You can calm them down, You can use oral corticosteroids for the short-term for very severe cases. You can calm them down, so patients can return to function, NSAIDs are relatively ineffective for this condition. 07:31 And you can also consider injecting for those patients who don't respond well to conservative treatment alone, which is mostly just splinting and rest. 07:39 Injecting with triamcinolone, for example. 07:43 And a small percentage of patients actually need to have that carpal tunnel released or open carpal tunnel surgery. 07:53 So, those are some of the big causes of hand and wrist pain. 07:56 I try to focus on things you see commonly in your clinical practice, but are also high-yield for USMLE. 08:03 Do keep that in mind as you move forward.
About the Lecture
The lecture Hand and Wrist Pain by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Hand and Wrist Pain
- The Anatomic Snuffbox
- Carpal Tunnel Syndrome (CTS)
Included Quiz Questions
A 35-year-old woman who works in a microbiology lab presents with two weeks of numbness and "pins-and-needles" sensation in her right hand, particularly her thumb, pointer finger, and middle finger. She has noticed that symptoms worsen when she does fine work in the lab. She could not grasp the precision knife between her fingers tightly enough to cut the gel agar the other day. The pain and numbness are worse in the mornings when she wakes up and eases when she gently moves her hand and "shakes it out." Physical examination shows no abnormalities. Which of the following is the most appropriate next step in diagnosis or management?
- Splinting
- Magnetic resonance imaging of the neck
- Referral to a hand surgeon
- HgA1c
- Erythrocyte sedimentation rate
A 32-year-old man is brought into the emergency department because of pain in his right wrist after he fell onto his outstretched arm with his wrist in dorsiflexion. On physical examination, he has tenderness in the anatomical snuffbox. Which of the following bones is most likely fractured?
- Scaphoid
- Lunate
- Trapezium
- Ulna
- Pisiform
A 32-year-old man is brought into the emergency department because of pain in his right wrist after he fell onto his outstretched arm with his wrist in dorsiflexion. On physical examination, he has tenderness in the anatomical snuffbox. Neurovascular examination is unremarkable. An X-ray shows no abnormal findings. Which of the following is the most appropriate next step in management?
- Immobilization and X-ray in 10 days
- Short-arm thumb spica cast for 6-10 weeks
- Immediate surgical referral
- Long-arm thumb spica cast for 6 weeks
- Acetaminophen and follow-up in 6 weeks
Which of the following is not a complication of scaphoid fracture?
- Chronic tendinopathy
- Avascular necrosis
- Non-union
- Malunion
- Frozen wrist joint
Which provocative test is used to diagnose de Quervain's tenosynovitis?
- Finkelstein's test
- Phalan's test
- Speed's test
- Compression test
- Hawkins–Kennedy test
Which of the following is the most appropriate step in management of a patient with a clinical diagnosis of carpal tunnel syndrome that has caused no sensory deficits and has not disrupted sleep or daily function?
- Splinting
- Intravenous steroids
- Nonsteroidal anti-inflammatory drugs
- Opiates
- Open surgery
de Quervain tenosynovitis is inflammation of which of the following structures?
- Extensor pollicis brevis and abductor pollicis longus tendons
- Median nerve sheath
- Digital flexor muscles
- The deep fascia of the palm
- Extensor pollicis longus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |