Playlist
Show Playlist
Hide Playlist
GI Bleeding: Management
-
Slides GI Bleed General Surgery.pdf
-
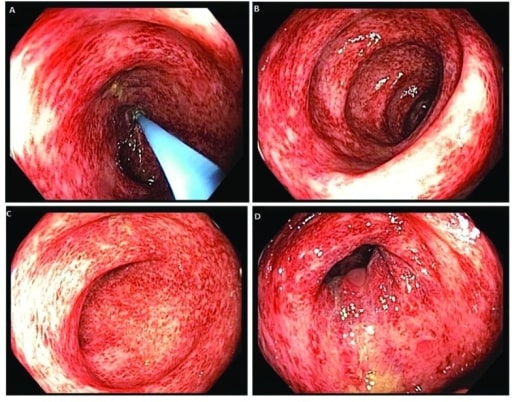
Download Lecture Overview
00:00 What are the initial management priorities in patients with GI bleed? It’s all about stabilizing the patient. 00:07 We stabilize the patient and then we localize the bleed. Stabilize the vital signs by giving fluids, by replacing the blood. Maybe you should consider putting the patient in the intensive care unit or a monitored setting. Like I mentioned, fluid and blood transfusion just to replace the significant blood loss. Don’t forget. Make sure you place two large bore IVs. After the initial stabilization period, the patient is subjected to an endoscopy. Oftentimes, prior to the GI doctors performing the endoscopy, whether it’s upper or lower, we often advise doing a nasogastric tube placement with a stomach lavage. 00:56 The gastric lavage will let you know whether or not the bleeding source is either upper or less likely to be upper. Endoscopy can be done safely under sedation. When patients have large volume hematemesis, considering intubating the patient or putting a breathing tube down to protect the airway. 01:16 Remember, the beauty of endoscopy is it’s much like mesenteric angiography, both diagnostic and potentially therapeutic. Angiographic embolization should be performed if you’re able to localize the bleeding. Keep in mind that intestines may become ischemic after embolization. How will you know whether or not the intestines have become ischemic after embolization? I’ll give you a minute to think about that. That’s right. Patients will likely present with either worsening of the GI bleed or abdominal pain. Now, you’ve exhausted initial stabilization methods. You’ve gone the endoscopy route. 01:59 You’ve gone angiography route. Unfortunately, a portion of patients will still require surgery, although the good news is it’s rarely needed. Most bleeding, up to 80% of patients will resolve their gastrointestinal bleeding without having to see me, a surgeon. Now, how do I decide which surgery to offer? Recall, I mentioned that the ability to localize the source of bleeding is of utmost importance both diagnostically and therapeutically particularly important for surgeons who have to decide which segment of colon to remove. The question then is are you able to localize the bleed with the diagnostic maneuvers that you have? If the answer is yes, I’m able to offer a more localized restricted resection. So for example, if through mesenteric angiography or the bleeding scan shows that the bleeding is the left side of the colon, there’s no need for me to take out the entire colon. What about the situation where despite exhausting your diagnostic maneuvers, you cannot localize the source of bleeding? In that scenario, when surgery is offered, it must be a subtotal colectomy. Subtotal colectomy meaning, remove the entire intraabdominal portions of the colon. Why is that necessary? If one chooses to do a segmental colectomy without localizing guidance, the bleeding risk is very, very prohibitive. We recommend against doing a segmental resection if the bleeding is not able to be localized. The management of GI bleeding relies on the ability to localize the source. I can’t stress that enough. Therefore, if the bleeding stops and the bleeding restarts, we have to start from square one again to try to localize the source. 03:52 Oftentimes in clinical management, our colleagues will tell us both in endoscopy as well as angiography as well as in nuclear medicine that they don’t see any evidence of ongoing bleeding or active bleeding. 04:05 That’s an important fact because without any signs of ongoing bleeding, we have no ability to localize. 04:11 Yet, there’s going to be a certain number of patients who are clearly still bleeding despite the inability to localize the source. High yield information for examination, when is surgery indicated? Surgery is indicated for GI bleeding patient when the patient becomes unstable, the patient can be hypotensive, mental status changes, oliguria or low urine output. Traditionally, if the patient has exceeded six units of packed red blood cell transfusion, although this criteria is one that’s fluid. 04:46 And very importantly, if the patient rebleeds after angiographic or endoscopic management, angiographic embolization or endoscopic, for example clipping. Rebleed almost guarantees that the patient will continue to bleed without surgical intervention. Thank you very much for joining me on this discussion of gastrointestinal bleeding.
About the Lecture
The lecture GI Bleeding: Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is the LAST step in the management sequence of brisk gastrointestinal bleeding?
- Localization of the bleeding
- Monitoring in the ICU for selected patients
- Fluid replacement
- Blood transfusions
- Stabilization of the vital signs
How can gastric lavage performed prior to endoscopy help in the management of an upper gastrointestinal bleed?
- It can aid in better visualization during the endoscopy.
- It may help control the bleeding in some patients.
- The return fluid can be sent to the lab for pathologic evaluation.
- It helps reduce symptoms of nausea in the patient.
- It helps reduce abdominal pain in the patient.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |