Playlist
Show Playlist
Hide Playlist
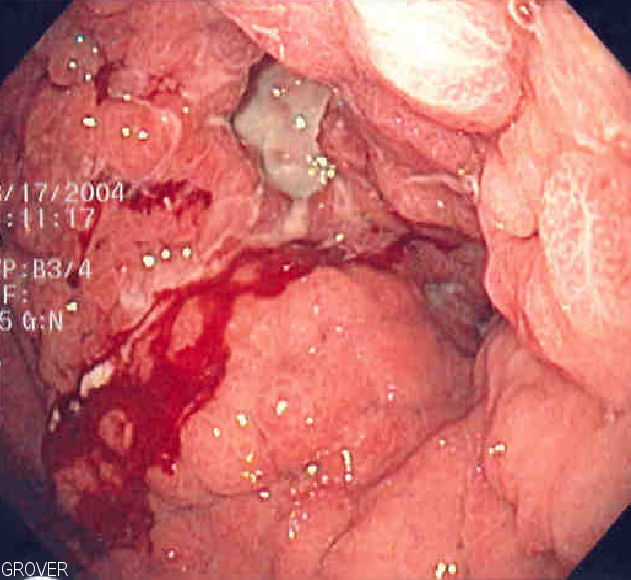
Gastric Lymphoma (MALToma)
-
Slides GIP Gastric Lymphoma MALToma.pdf
-
Download Lecture Overview
00:01 Welcome. 00:02 In this talk, we're going to cover MALT lymphomas. 00:06 This has nothing to do with malted milk or malt in beer. 00:11 This has to do with mucosal associated lymphoid tissue lymphomas. 00:17 So MALT, as I've already said, that's the abbreviation lymphoma are typically quite indolent non-Hodgkin's lymphomas that arise in lymphoid tissue associated with various mucosa. 00:28 And it's usually occurring in the setting of chronic inflammatory states. 00:34 Let's look at some of the epidemiology here. 00:36 So overall, if we look at all non-Hodgkin's lymphomas anywhere in the body, roughly 5%-10% of them are going to be mucosal associated or malt lymphomas. 00:48 The highest incidence for a variety of reasons, some of which I don't understand, are in non-hispanic whites. 00:57 It's primarily seen in older individuals, the median age at diagnosis is somewhere about 65 years of age or the usual social security retirement age. 01:08 It's associated as I've already said, with chronic inflammatory states, and typically chronic inflammatory states associated with various mucosa. 01:18 What is happening is with that inflammation, we are driving in the draining lymph nodes proliferation of the marginals zone B cells that's the appropriate response in a lymph node with a localized area of inflammation. 01:31 But if we drive that over and over and over again, we will eventually acquire mutations that will lead to the formation of a non-Hodgkin's lymphoma. 01:42 So as you might expect, in terms of pathophysiology, autoimmune disease, and chronic infections that never clear are going to be major drivers of these lesions. 01:54 Of the autoimmune conditions, this is just a partial list but Sjögren's syndrome associated with sialadenitis. 02:01 And so you would have mucosa associated with the oropharynx that could develop MALT lymphomas, lupus, relapsing polychondritis, Hashimoto's thyroiditis, again, a partial list. 02:15 Chronic infections, and there's a long list there. 02:17 This is only partial, but the one you should remember is Helicobacter pylori, and that's going to lead predominantly to gastric mucosal MALT lymphomas. 02:30 How is this happening? So we're showing a schematic more or less of the epithelium lining the stomach and kind of grazing over the surface, you see all the spirochetes representing the Helicobacter pylori. 02:44 Deep to that within the submucosa, we are looking at nodal tissue. 02:50 So nascent lymph nodes that are being driven by things an antigen stimulation draining off of the epithelium. 02:59 With prolonged bouts of inflammation here represented by all of the neutrophils and the macrophages and the lymphocytes, we're going to eventually, with that ongoing inflammatory process, have a number of antigens that are going to drain appropriately into the nodal tissue and we're going to get the appropriate immune response. 03:23 And we will get an elaboration within the marginal zones of the B cells that would normally be responsible for fighting off the infection. 03:32 So we get these rather large, very prominent nodal proliferations. 03:38 You see above that we've had some epithelial injury and that may be part and parcel of this, but the epithelium doesn't even need to be particularly damaged just with chronic inflammation. 03:49 There are various markers of the cells that are proliferating, so c-myc and bcl10. 03:55 There may be over time additional mutations that are acquired including translocations. 04:00 And in these proliferating nodes, we will get the development of MALT lymphomas. 04:06 This is just showing you the histology what that looks like. 04:09 It looks like a lymphoma anywhere else except it happens to be in a mucosal bed. 04:14 So the clinical presentation will depend on the underlying etiology whether it's autoimmune or infectious. 04:20 And then some of the other secondary manifestations depending on the size of the tumor, and depending on its location, you may have reflux disease, you may have epigastric pain or discomfort. 04:33 If it get a large enough tumor mass, you may develop as a result of the tumor itself. 04:38 Secondary anorexia, with that may come weight loss, you may have a occullt GI bleeding due to mucosal erosion overlying these rather large nodal proliferations. 04:50 And the symptoms wherever they occur are going to be largely reflective of the local anatomy. 04:57 Making the diagnosis. 04:59 You can do a peripheral blood count and a differential. 05:03 Usually in lymphomas as you're undoubtedly aware, you will not see necessarily in up regulation and the number or even the abnormal behavior of peripheral blood lymphocytes. 05:17 You may see as a result of turnover of the MALT lymphoma and elevated lactate dehydrogenase, so LDH will be elevated. 05:25 You do want to rule out other potential etiologies, such as multiple myeloma. 05:30 So you would do a serum protein electrophoresis to evaluate for monoclonal gammopathy. 05:35 Thirdly, you would want to do imaging. 05:37 CT and MRI to look for the extent of disease and where disease is. 05:41 PET and CT can also be done. 05:44 And then you want to biopsy it. 05:45 Of course, because I'm a pathologist, everything comes down to the biopsy. 05:49 This is no exception, you need to know what you're dealing with. 05:52 Because the specific therapy for MALT lymphomas will be driven by their underlying etiology and the therapy is different let's say for a carcinoma or for a GI stromal tumor. 06:05 The markers for these tumors, the MALTomas are going to be very similar to what's in a marginal zone lymphoma, elevated CD19, and an elevated CD20. 06:16 Those are typical markers of proliferating marginal B cells. 06:22 They're going to be CD23, another marker that's typically seen in mantle zone lymphomas. 06:29 Probably not necessary that you remember that, it is necessary to remember that there are specific markers and that biopsy is how you're going to be able to make the diagnosis. 06:38 How are we going to manage this? Well, in fact, because we know in many cases, these are driven by chronic infections, let's treat the chronic infection and get rid of that inflammatory stimulus that's driving the proliferation of these cells. 06:53 So if if we know or suspect that it's, for example, secondary Helicobacter pylori, we can do eradication therapy with triple antibiotics. 07:03 We can do follow up serial endoscopies to make sure that these tumors can regress and they frequently do once we take away the antigenic stimulation. 07:13 In the cases where they don't regress, then we can treat with radiation or systemic chemotherapy. 07:19 And in instances where we have perforation, uncontrolled bleeding, obstruction, we may actually have to progress to gastric resection. 07:29 The prognostic factor is things that have a worse prognosis. 07:31 So the older you get, the worse prognosis. 07:34 Stage lll and lV disease where you have much more systemic spread rather than just locally within a particular spot in the GI tract. 07:45 Serum LDH levels that are very high, indicating that we have a lot of cellular turnover within the tumor. 07:53 And depending on the various prognostic factors, depending on response to therapy, all of those things, 5-year survival is not terrible. 08:01 And in fact, in some cases where it's more indolent and more localized, it's almost 100% survival. 08:09 So, you've now learned about MALT, lymphomas or MALtomas.
About the Lecture
The lecture Gastric Lymphoma (MALToma) by Richard Mitchell, MD, PhD is from the course Disorders of the Stomach.
Included Quiz Questions
What is the most strongly established risk factor for gastric lymphoma?
- Helicobacter pylori
- Autoimmune conditions
- Borrelia afzelii
- Chlamydia psittaci
- Relapsing polychondritis
What is NOT commonly considered to be a risk factor for gastric lymphoma?
- Epstein-Barr virus
- Sjögren syndrome
- Systemic lupus erythematosus
- Hashimoto thyroiditis
- Achromobacter xylosoxidans
What is the initial management of Helicobacter pylori-positive gastric MALT lymphoma?
- H. pylori eradication therapy
- Radiation
- Observation
- Surgery
- Chemotherapy
For a patient with initial treatment failure, what is the preferred treatment for gastric MALT lymphoma?
- Radiation
- Surgery
- Chemotherapy
- Immunotherapy
- Antibiotic eradication therapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |