Playlist
Show Playlist
Hide Playlist
Fluid Replacement Therapy (FTP) in Children: Management
-
Slides IVfluids Pediatrics.pdf
-
Download Lecture Overview
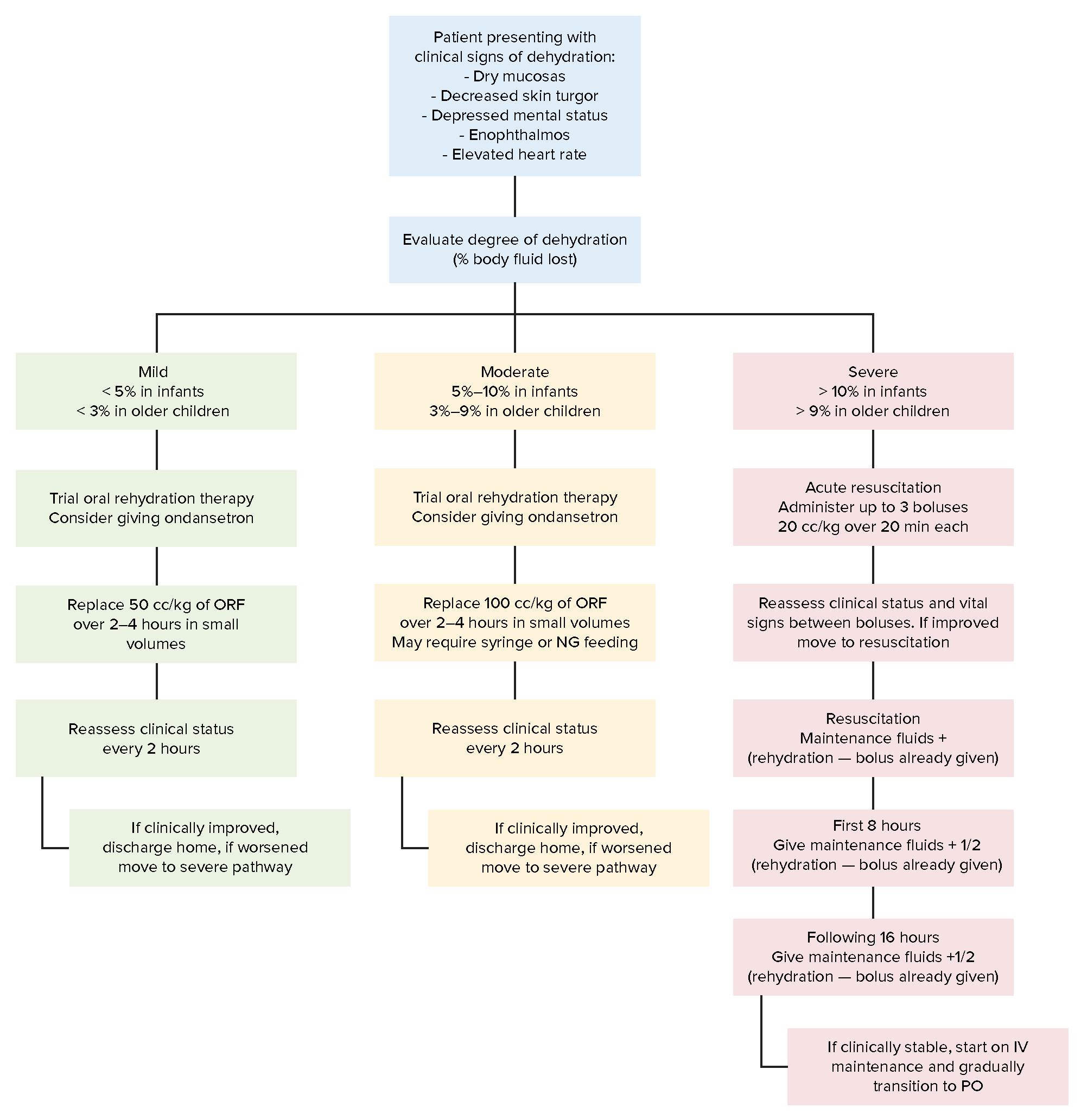
00:01 So, if we have a child who we’re worried about dehydration, we’re going to generally give a bolus of fluid. 00:11 But additionally, we want to typically calculate a child who’s not drinking what their maintenance is. 00:18 Maintenance is how much fluid an average human needs to continue to survive generally per hour. 00:27 And we’re going to add on top of maintenance any ongoing insensible losses that this child may need. 00:34 To calculate maintenance, I want you to use the 4-2-1 rule. 00:38 It’s a little bit easier than the 150-25 rule, which is calculating daily requirements. 00:46 Let’s focus on 4-2-1 from a practical standpoint. 00:49 So, for the first 10 kilograms of a patient, their maintenance is 4 cc per kilogram per hour. 01:00 For their next 10 kilograms, you’re going to add 2 cc per kilogram. 01:05 And for every kilogram of weight after that, we’re going to add 1 cc per kilo, 4-2-1. 01:12 This is confusing to a lot of people, so I’m going to go through a few example calculations just to make it really clear. 01:19 Here is a 4-kilogram child. 01:22 They have less than 10 kilograms. 01:24 So, every single kilogram they’re going to get is going to get 4 per kilogram. 01:29 So, 4 x 4 is 16. 01:32 This child needs 16 cc per hour of maintenance fluids. 01:38 Here’s a child who weighs 16 kilograms. 01:42 For the first 10 kilograms, they need 4 cc per hour. 01:46 That’s 40. 01:48 For the next 6 kilograms, they need 2. 01:52 So, that’s 12; 40 plus 2 is 52. 01:56 So their total requirements are 52 cc per hour. 02:00 One more example to make it perfectly clear, if we have a 37-kilogram child, we do 4 for each of the first 10 kilos, that’s 40. 02:09 We do 2 for each of the first 10 kilos, that’s 20. 02:13 And we do 1 for each of the subsequent 17 kilos, that’s 17. 02:18 Add 40 + 20 + 17 and we get 77 ccs per hour of maintenance fluids. 02:25 The 4-2-1 rule. 02:29 However, IV fluids can have complications. 02:33 We can misestimate the amount of sodium required or the situation that a child has. 02:39 So it was a general rule of thumb we want to try to use the gut first. 02:43 The first thing we’ll try is we’ll simply ask the child to drink. 02:47 No matter how dehydrated a child is, if a child is capable of drinking, they’re probably going to be up to drink themselves back into health. 02:55 So, we’ll get them something to drink. 02:58 We often will choose something like oral rehydration fluid. 03:02 For example, Pedialyte, which is marketed in the United States, or World Health Organization rehydration solution. 03:09 Any of these things are fine. 03:11 These have some salt in them. 03:14 Remember, Gatorade doesn’t have salt in it, it’s just sugar. 03:19 People sometimes think that it does because of a good advertising campaign, but it doesn’t. 03:23 We really want to use oral rehydration fluid, especially in the younger infants. 03:29 Milk and fatty drinks are sometimes what a child wants, but especially in a child who’s vomiting, we like to avoid fatty things because they have a slower stomach transit time, and that child may be more likely to vomit than if they are drinking the Pedialyte. 03:46 Additionally, and especially with vomiting children, we will often add ondansetron empirically, especially in gastroenteritis because it has been shown to improve the odds of success of an oral challenge, and therefore, prevent a hospitalization. 04:02 Don’t give up on the oral route yet if the child won’t drink. 04:06 Especially in younger kids, we can do syringe feeding. 04:10 Here’s what we do. 04:12 We calculate what maintenance is using the 4-2-1 rule. 04:16 Add a little extra if the patient has ongoing losses like diarrhea. 04:20 And then we ask the parent or the provider to divide this amount of hourly into 10 to 20-minute intervals. 04:29 So if the child needs 60 milliliters in an hour, they can get 10 to 20 milliliters every 10 to 20 minutes, and they’ll end up being the same amount. 04:39 Now, we place that into an oral syringe and literally squirt it physically into the child’s mouth every 10 to 20 minutes. 04:48 Within a few times, the child will be used to doing this, and will complain no longer, and oftentimes, this attempt, if you have the time to teach a concerned parent, will prevent IV administration of fluids. 05:03 Lastly, we can also give the patient an NG tube. 05:08 The NG tube is placed into the stomach and is effective even in a vomiting child. 05:15 For a bolus through the NG, we’re going to give 50 to 100 cc per kilogram of Pedialyte over three to four hours by a pump continuously. 05:25 This seems like a lot of fluid. 05:27 If you’re worried especially in the larger kids, I’ll bump it down to 50. 05:32 Then, calculate maintenance and run the childhood maintenance through the NG tube. 05:38 This can be more effective than IV fluids if the child is willing to keep an NG in place. 05:45 Typically, it’s your two or three-year-old that will be ripping out the IG and it may not be worth a bother and you’ll have to go with the IV. 05:53 So we have all else fails, we’ll consider an IV. 05:58 Clysis is not used in most center but is out there, so I wanted to mention it. 06:03 It’s actually an IV that’s placed into the skin often after injection of hyaluronidase, which allows for the skin to absorb fluids. 06:13 You can run maintenance fluids directly into skin. 06:18 We learned about this in veterinary medicine and it actually works in kids and adults too, it’s just not commonly employed. 06:25 When it is employed, we typically use the exact center of the back so the child can’t get to their clysis tube. 06:33 When you decide to give IV fluids, what are you going to use? This is a moving area in pediatrics. 06:46 Previously, students were taught that we might use quarter normal saline in very small children because they don’t need that much sodium. 06:57 This is actively changing in pediatrics, and it has to do with making mistakes and what error are people likely to make. 07:05 It does not change because people feel that children need more sodium. 07:13 Allow me to explain. 07:15 Here, I have a patient who’s receiving hypotonic fluid and a patient who’s receiving normotonic fluid. 07:24 There is a risk in both circumstances. 07:26 If I give all my patients hypotonic fluid like quarter normal saline for those very small children under 10 kilograms, which would be appropriate from how much sodium do I need every day standpoint. 07:41 The problem is I may miss a case of hyponatremia especially in a patient with SIADH. 07:50 So, I worry about unrecognized SIADH and just routinely giving quarter normal saline because that will further drive down their sodium level and put them a risk for seizure. 08:04 If I were to give everyone in the hospital normotonic fluid, there would not be that risk as much of too much fluid in the setting of SIADH. 08:15 But instead, you might say, “Wait, wait, wait, you’re giving too much sodium in a patient who has renal failure.” The thing is that you are much more likely, in pediatrics, to have a patient who has unrecognized SIADH than you are to have a patient with unrecognized end-organ renal failure. 08:36 So, a patient with renal failure is going to be edematous, be sick, be peeing blood, you’ll know that this child has renal failure. 08:45 But unrecognized SIADH is downright common. 08:49 We see unrecognized SIADH routinely in meningitis, pneumonia, gastroenteritis, bronchiolitis. 08:57 Anywhere, there’s a cell that can make SIADH like the lungs, the meninges, the intestines, we can have unrecognized SIADH. 09:08 So because that risk of error is more common, most centers are moving now to using more normotonic fluid. 09:17 We can use the D5 half as a way to make a guess right in between, mitigate both risks. 09:26 But typically, we’ll either use normal saline or half normal saline. 09:30 There is a concern in excessive normal saline use of worsening acidosis because of all the chloride. 09:37 So that’s something to think about in an acidotic patient as well though. 09:42 There is benefit because in the hypotonic fluid case, you’re giving less sodium in the event of unrecognized renal failure, which is very rare. 09:52 But there’s a huge benefit in normotonic fluids because you’re less likely to cause hyponatremic and SIADH. 10:00 I feel like that’s a pretty clear point but one that should be made. 10:03 So we’ve resuscitated the dehydrated child. 10:06 We gave normal saline boluses, 20 per kilo, until that child has recovered. 10:12 And now, we’re selecting a maintenance IV fluid. 10:15 We can’t use the oral tract the child is refusing to drink and he’s going to rip out his NG tube. 10:20 What do we choose? Well, first off, you’ll notice we do D5 normal saline. 10:26 Again, not hypotonic fluid because we’re worried about that unrecognized SIADH. 10:33 The dextrose, I’ll get to in a second, but first, I want to talk a little bit about potassium. 10:38 We’ll typically add 20 milliequivalents per liter of potassium into the IV fluids if the child is NPO and the child does not have renal insufficiency. 10:49 Some practitioners prefer to wait for the child to urinate once before adding potassium. 10:54 That’s really an incredibly rare thing to have unrecognized renal insufficiency, but you might think about it in the critical care setting. 11:02 We always add that dextrose, that D5, which is 5% dextrose to pediatric patients because again, they have lower stores of glycogen in their livers and they’re at grave risk for hypoglycemia. 11:16 You’d be crazy not to add dextrose especially in a child with gastroenteritis. 11:22 For severe dehydration, we’re going to start by giving the bolus, and that bolus again is 20 milligrams per kilo as an IV bolus over 20 minutes. 11:32 And you keep repeating those boluses until the child has stable vital signs. 11:38 When I say keep repeating, we’re talking about maybe three times. 11:43 If you’re entering your fourth bolus, that child probably is not going to respond to further hydration, and you really need an agent like dopamine. 11:53 And excessive overhydration and overbolusing may cause a pulmonary edema. 11:59 So you want to be careful with that. 12:01 For severe hypoglycemia, if a child has a very low glucose, we will typically give 5 cc per kilo of D10 via a peripheral IV. 12:14 That will emergently raise the sugar so they don’t seize, and then we’ll go back to the start and provide them with maintenance fluid. 12:23 So, how do you know if it’s working? Well, the best way is simply to follow the urine output. 12:30 And we have to be careful to weigh every single diaper that comes out of that child. 12:34 Optimal normal output in any patient of any age is more than 1 cc per kilo per hour. 12:42 So, if I have a 10-kilo child and I’ve been watching them for 12 hours, I expect 120 milliliters of water or urine coming out of them in terms of diaper management. 12:55 The problem is if they have diarrhea, you may be also weighing insensible losses and you may be missing the fact that this child is in fact getting dehydrated. 13:04 So we can’t purely rely on urine output, we have to rely on other things as well like the patient’s physical exam and looking for signs of dehydration. 13:14 So, what are the signs of dehydration that we look for? Well, we’re going to continue to follow that normal skin turgor, which is the worst and last thing to change. 13:24 We’ll continue to look for normal mental status, which is a late finding. 13:29 We will watch for mucous membranes becoming dry. 13:33 That is an early finding, and in fact perhaps, the first. 13:36 And last is the normal heart rate, which we will keep an eye on, but remember, these children in the hospital setting are afraid, may be in pain, may not like their IV, and all of these things can artificially raise their heart rate. 13:49 It’s not necessarily true that they have dehydration. 13:53 Watching their heart rate over time is important especially at those times when they’re cuddled in their parent’s arms, so you can really start to see a difference. 14:03 That’s everything I have for you today about dehydration and IV management of fluids in children. 14:09 Thanks for your attention.
About the Lecture
The lecture Fluid Replacement Therapy (FTP) in Children: Management by Brian Alverson, MD is from the course Pediatric Gastroenterology. It contains the following chapters:
- FPT Management: Maintenance Fluids
- FPT Management: Use the Gut
- FPT Management: Maintenance IV Fluid of Choice
- FPT Management: How Do you Know it’s Working?
Included Quiz Questions
A child weighs 17kg. What is his maintenance IV fluid requirement?
- 54 cc/hr
- 34 cc/hr
- 47 cc/hr
- 77 cc/hr
- 60 cc/hr
Which of the following is a known benefit of hypotonic fluids?
- It has less sodium which is good if the patient has an unrecognized renal failure
- It can cause hypernatremia in patients with unrecognized SIADH
- It can cause hypernatremia in the case of a patient who has unrecognized renal failure
- It has less chance of hyponatremia in the case of a patient who has an unrecognized SIADH
- No additional benifit over normotonic fluid
What is the best method for assessing hydration in a child during fluid resuscitation?
- Monitoring urine output
- Monitoring serum sodium levels
- Monitoring pulse and blood pressure
- Monitoring the level of alertness
- Examining mucous membranes time to time
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
One of the best lecture. It makes many things clear. However, I feel there is one part that is missing: the compensation of fluid loss based on the estimated dehydration state. Everything else is great and much better info that I encountered before.
Very good lecture aboud how much serum can administrate in the hospital. Especially in gastroenteritis.