Playlist
Show Playlist
Hide Playlist
Hypertension: Endocrine & Cardiovascular Causes
-
Slides Hypertension.pdf
-
process of diagnosis - hypercortisolism.pdf
-
Download Lecture Overview
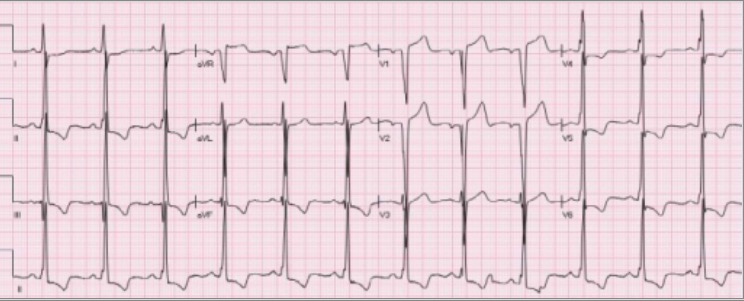
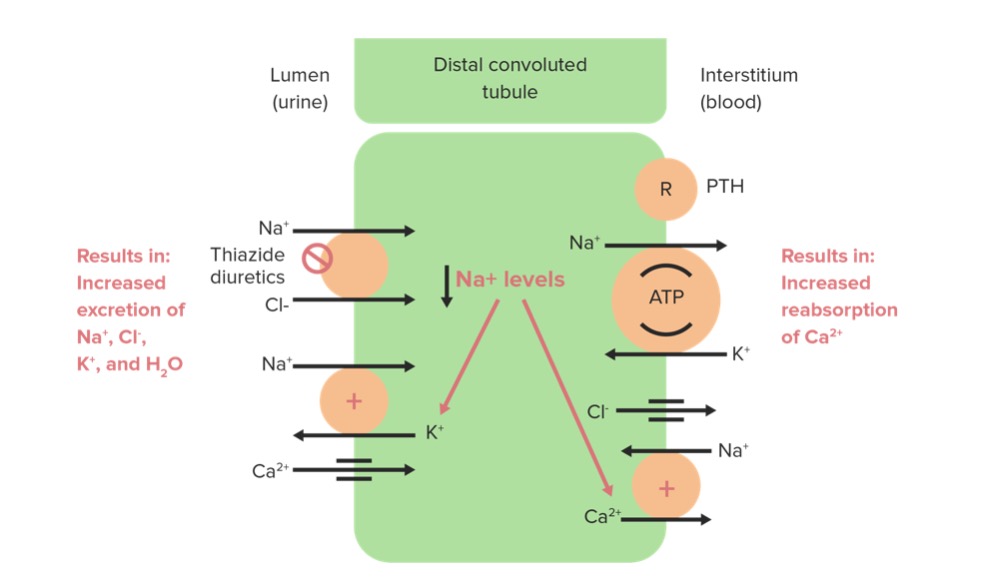
00:01 Our topic continues with secondary hypertension. Here, however, we are in the concept or in the topic of endocrine. What does that mean? Well, remember hypertension crosses all borders. 00:12 At this point, we have completed secondary hypertension when dealing with the renals, when we went through those important differentials. Here under endocrinology, when we are referring to Cushing’s syndrome, now right off the bat, close your eyes and think about all the different sources in which Cushing's could take place. As soon as you hear about Cushing's, take the scene Cushing's please and you know that you have excess cortisol. Excess cortisol. 00:37 Whatever form that maybe, glucocorticoids, prednisone. So here we have Cushing’s syndrome. 00:43 What are the four different causes? As you go through them, tell me as to what is the most important or what is the most common cause of Cushing's? It is actually not even from our body. It is exogenous sources. What is that called, please? Called factitious. 00:55 It is called iotrogenic. It is exogenous. Do you understand anytime that you see those three words, what are they again? Iotrogenic, exogenous or factitious. That to you should mean, that particular drug hormone whatever it maybe is coming from an outside source, is that clear? I hope so. So that is the most common, isn't it? Think about prednisone. All the different reasons as to why patient might be taking prednisone. I am going to give you secondary hypertension. 01:22 Let us move into this. This is Cushing’s syndrome. Where am I? Not in the anterior pituitary. 01:28 How do you know? Because anterior pituitary, would you call this Cushings syndrome? Good. No, you wouldn't. 01:36 You'd call this Cushing’s disease if it was anterior pituitary. "So Dr. Raj what in the heck that you are getting at?" If you had a tumor in the adrenal cortex that is producing cortisol, are you only producing cortisol? No, you might also be producing aldosterone. 01:53 Now you are getting to my point. What is my topic? Secondary hypertension. Remember, please. 01:57 In this case, the pathology, the end game is the fact that you are going to develop increased blood pressure. And that increased blood pressure is coming from aldosterone in Cushing’s syndrome. Take a look at the patient here. The face, moon facies. What are we looking at in this patient's torso? It is the fact that there is truncal obesity and we have striae. What else might you find in the back of the neck perhaps? You are looking at buffalo hump, right? So that your patient in general with Cushing's because of excess corticoid from whatever source. Just to be complete, the other sources included the anterior pituitary and then also your lung. And from the lung, you should be thinking about most commonly, small cell lung cancer. Now my point is this. If you produce too much aldosterone at some point in time, what may happen? You may then cause increase in blood pressure resulting secondary hypertension. Cushing. Now be very careful because our next differential here for secondary hypertension. Take a look. We have removed our patient because this is Conn's syndrome. Conn's sydnrome was not going to have moon facies, buffalo hump and so on and so forth as we just saw. Conn's syndrome is a primary, listen to what I am saying? It is all about verbiage. It is all about terminology and if you are not careful about terminology when you are reading something, it is quite easy for you to miss a question, might be quite easy for you to misintepret your patient. You do not want to do that. So it is primary hyperaldosteronism. 03:14 What does primary mean to you? It means that that particular problem or pathology is actually taking place from that organ. Aldosterone comes from where? Adrenal cortex. What layer? Glomerulosa, the most superficial layer. You have a tumor there that is producing too much aldosterone. This is called Conn's syndrome. This is primary hyperaldosternoism causing what kind of hypertension? You said primary. I am sorry. As much as you want to, please note that this is not primary. It is secondary hypertension. How common is this? More common than what you think. Make sure you know about Conn's. So in Conn's syndrome, it is a primary hypoaldosteronism with a tumor in your adrenal cortex producing too much aldosterone resulting in what kind of hypertension? Secondary hypertension. Is that clear? Now give me the labs here because you are not done. You are going to be given a sheet of labs and you have to be able to interpret as to your patient having Conn's. What happens to sodium? Increase. What does that mean? Greater than 145. What about potassium? You are getting rid of it because you have too much aldosterone. So my potassium is less than 3.5. And then what about hydrogen? You are getting rid of your hydrogen. So what happens to your pH? Increases. Welcome to alkalosis. Is that clear? Welcome to Conn's. 04:28 This is something we have looked at, we will look at and we'll forever look at because it comes up so many different times. Let us continue. Endocrinology, now we have pheochromocytoma. 04:39 Where am I? Where are you? You are still in adrenals, but what part please? The medulla. 04:43 In the medulla, you might have a tumor. You have a tumor that does what? Produces too much of your epinephrine. Remember normally speaking, 80 percent of your epinephrine comes from where? It comes from the adrenal medulla, doesn't it? Eighty percent does. What about epinephrine? Epinephrine works on many receptors, catecholamine receptor, alpha-1, alpha-2, beta-1, beta-2. At lower doses works on what? Beta. At higher doses work on alpha. Works more like an epinephrine. You know that from form, I'll walk through that quickly. Right now let's just focus upon the path. Inferior chromocytoma, you have too much epinephrine and did you have this epinephrine all the time? Is it constitutive? No. It is episodic. You pay attention to the term episodic hypertension. If you have too much epinephrine, at some point in time might you find its metabolites in the urine? Sure you will. What is that called? VMA, vanillylmandelic acid may be metanephrine so much so forth. This episodic hypertension, headaches, diaphoresis, what does that mean? Remember too much sympathetic activity. Would you please tell me how you sweat? It's a sympathetic or parasympathetic influence. Sympathetic. Remember one of the big exceptions, sympathetic muscarinic receptor, diaphoresis, palpitations all the time. No, not like Grave's disease. Is that clear? Give yourself a differential, palpitation, Grave's. Here we have pheochromocytoma. 06:01 Let us continue. Adrenal mass. Where are you? Adrenal medulla. What kind of tumor? It is a benign tumor. What are you going to find? Plasma free metanephrines, urine here it is, VMA, vanillylmandelic acid. What does that mean? It means that these are the metabolites of your epinephrine being broken down. Rule of tens. This is something that we discussed in endocrinology. Ten percent of the time it might be sporadic. Ten percent of the time might be familial. Ten percent of the time might be both kidneys are affected, so on and so forth. What else may result in secondary hypertension when dealing with endocrinology? How about the thyroid gland? If it is hyperthroidism, it might then increase your systolic blood pressure, SBP. And if it is hypothyroidism, then it might be something like increased diastolic blood pressure. That is important for you to know clinically, please. Hyper is the fact that your patient's heart feels how? Oh! It is palpating. And you have hypothyroidism, increased diastole blood pressure, thyroid gland. Continue. What about another endocrine pathology that may result in secondary hypertension, but this is hyperparathyroidism. What is this? This is the fact that you are producing too much what? PTH. Where? Your parathyroids. 07:05 Where am I? Right around the thyroids and you have your parathyroid producing too much PTH. What is that going to do? It is going to run to the kidney. It is going to do what? It is going to reabsorb the calcium. What kind of effect does calcium have on your blood vessels, please? Think about that. Your blood vessel normally is what kind of muscle? Smooth. 07:25 What does smooth muscle mean to you? Think about alpha-1. Are you there? Bring in some biochem here. You've alpha-1 receptors, what does it do? It stimulates your phospholipase. 07:36 What are you going to release? IP3, DAG. What are you going to do next? Release calcium. 07:43 What does alpha-1 do to your blood vessel? You know it causes vasoconstriction. So, therefore, you have the calcium bind to calmodulin, so that you do what? Vasoconstriction. What is that going to do to your TPR and here we will go on and call this PVR. It increases resistance. 07:56 Peripheral vascular resistance is going to be increased. Is that going to increase your blood pressure? Sure it will. What kind? Secondary. Are you following me? Everything that we're going to do here have an explanation, has a story. You relate this to a patient, a presentation what-not, you are in good shape. You cannot be fooled. I don't care who you are. Understand your patient. You won't miss a single question. Next under cardiovascular, still secondary hypertension, we have a condition called coarctation of aorta. As soon as you have coarctation of aorta, close your eyes, think of what please? Think about this patient. Listen to what I am saying. There is webbing of the neck. There might be two cusps of the aortic valve. Interesting. If it is a female, XO and if it is the ovaries may result in something called dysgerminoma ovaries. Who is my patient? Turner syndrome. In this patient, you also noticed that the blood pressure in the carotids might be higher than the blood pressure in the extremities. 08:59 By extremities, I mean down by the feet. Think about the dorsalis pedis. The blood pressure in your upper extremity might be higher than the blood pressure in your lower extremity. 09:09 How does that occur? Remember Turner is a genetic problem with XO being the chromosome. 09:15 Next, what happened? I told you that there was a webbing of the neck. What is that called? It is called lymphangioma. Isn't it? It is the fact that the lymph is becoming dilated and you might actually be able to see this in vitro with an ultrasound in which the back of the neck you see being filled with fluid. That is your "webbing of the neck". Make sure that you know the full understanding of webbing. Number 2, what else did I say? I said that the aortic valve, which normally has now many cusps? It has three cusps normally. But is it possible that your patient might have congenital bicuspid aortic valve? Sure they can because your patient is Turner. And then what about the blood pressure? The differential, coarctation. What is that going to do? I want you to go back to physio and I want you to think about a pipe and a tube and you are going to add a resistor right in the middle. You see that right there. You added a resistor in the middle. When you added a resistor in the middle, what then happen to the pressure proximally? It increased. What happened to the pressure distally? It decreased. What did you do? You added your resistor in a series. Where am I? The aorta and you coarcted. What does coarcted mean? It means constriction. So what happens to the blood pressure in the upper extremity? You've increased it. And what about the blood pressure in the lower extremity? It is decreased. What do you think happens to perfusion of the kidney? Decrease. What kind of questions might they ask you on physio? May I ask you about decreased perfusion to kidney and coarctation, true or false? True. So, therefore, what are you going to release? Renin. When you go through the same concept, secondary hypertension, coarctation. 10:50 Let us continue. Obstructive sleep apnea. Now for this how much do you think of. Maybe in older patient, an obese patient perhaps and it is the fact that there might be obstruction taking place while breathing out. And so therefore around the vocal cords, maybe there is the pharyngeal folds and such and there might be excess muscle. 11:15 There might be excess "flap" and so, therefore, makes it difficult for your patient to properly breathe especially at night. Sleep apnea, maybe for intervals of greater than 10 seconds, there might be lack of proper breathing. That is amazing. That is very scary, isn't it? At some point in time, what is it going to happen? This patient is not breathing properly. 11:35 So if there is improper ventilation taking place, then what is the patient retaining? Because the patient is not able to blow off, what are you supposed to blow off normally? Carbon dioxide. But that isn't a happening in a patient with obstructive sleep apnea. You're literally obstructing the ability to exhale your carbon dioxide. Where is it remaining? Within your blood. What does carbon dioxide mean to you in terms of pH? Carbon dioxide equals acid, doesn't it? Of course, it does. Think about the carbonic anhydrase formula. So you're producing acid, so what kind of acidisosis is this? Respiratory acidosis, isn't it? And at some point in time maybe with obstructive sleep apnea during the day, you might find a little sleepy and the patient might be feeling a little tired and such, so obstructive sleep apnea. 12:20 So now what happens. Obesity, rapid weight gain with snoring, neck size. 12:26 What kind of treatment measures are you worried about in this patient? Well, you need to make sure that you clear up that airway ASAP. Think of CPAP, continous positive airway pressure.
About the Lecture
The lecture Hypertension: Endocrine & Cardiovascular Causes by Carlo Raj, MD is from the course Hypertension: Basic Principles with Carlo Raj.
Included Quiz Questions
What condition related to secondary hypertension is caused by excess cortisol?
- Cushing syndrome
- Primary aldosteronism (Conn syndrome)
- Addison disease
- Alport syndrome
- Pheochromocytoma
Which of the following conditions causes episodic hypertension?
- Pheochromocytoma
- Addison disease
- Cushing syndrome
- Cushing disease
- Primary aldosteronism (Conn syndrome)
What biochemical test is indicated in a patient with suspected pheochromocytoma?
- Metanephrines
- Aldosterone
- Cortisol
- Creatinine
- BUN
What is the most likely mechanism of hypertension in patients with hyperparathyroidism?
- Increased peripheral vascular resistance due to increased calcium levels.
- Increased preload due to increased calcium levels.
- Decreased peripheral vascular resistance due to increased calcium levels.
- Increased peripheral vascular resistance due to decreased calcium levels.
- Increased peripheral vascular resistance due to increased creatinine levels.
What is used in the treatment of obstructive sleep apnea?
- CPAP
- Diuretics
- Beta-blockers
- Calcium channel blockers
- NSAIDs
What condition is associated with higher blood pressure in the upper extremities than the lower extremities?
- Coarctation of the aorta
- Cushing disease
- Primary hyperaldosteronism
- Pheochromocytoma
- Hyperthyroidism
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
3 |
| 1 Star |
|
0 |
The best thing about Dr Raj is that his way of teaching is very dynamic and this keeps you in the lecture and makes you stay focused during the lecture. He is an excellent guy. I don't like plain and simple lectures, they are very boring. Also after I listened to his lectures, I don't just memorize, I learn. Best regards
I think that this is the kind of teacher that every med school should have. Personally, I like how he integrates all the information that it is given across the whole carrer. As a fifth year student from another country I would like that every class of lecturio be like the classes of Dr. Raj. Seriously, the integration is everything when you are in a rotation in front of a patient.
I do not have a major problem with the material he teaches, although sometimes he just points out to the facts and skips explanations. My major issue is with the overall demeanor of Dr. Raj while he is teaching. He tries to come across as someone cool and the George Clooney of the lecturio and it's very annoying and distracting. At least for me. For those who haven't noticed, look at his facial expression when delivering a lecture. I wish he would just lecture plane and simple without resorting to " hey you know I'm cool, right?". I try not to look at him and just stare at the slides to minimize this effect.
Excelent teacher , Very well organizated , All the people that are complaining that he speaks too fast maybe they need to study " Faster" haha , Carlo raj is one of the best teacher in lecturio