Playlist
Show Playlist
Hide Playlist
Diverticulosis and Diverticulitis
-
Slides GIP Diverticulosis Diverticulitis.pdf
-
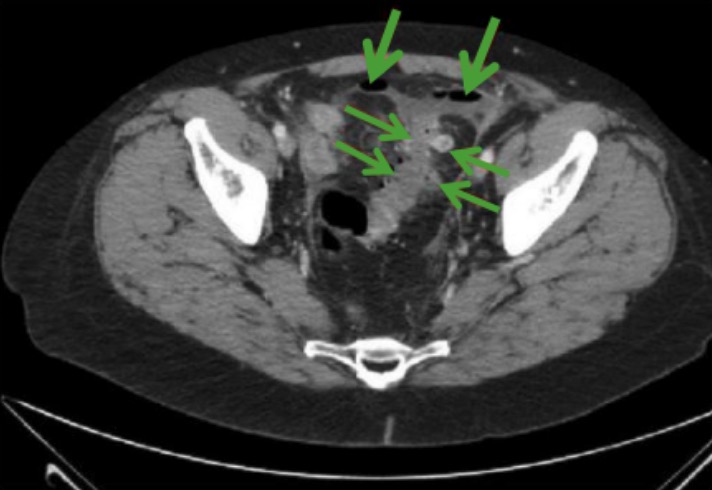
Download Lecture Overview
00:01 Welcome. In this talk we're going to be covering diverticular disease. 00:06 In diverticular disease, for the most part in this talk is going to be referring to outpouchings of the colonic wall. 00:14 When we talk about diverticulosis, it's going to be outpouching of the colon. 00:19 Diverticulitis on the other hand is inflammation of a diverticulum. 00:24 So, together, diverticulosis and diverticulitis is diverticular disease. 00:30 The normal three layers of the bowel are indicated here in a schematic form. 00:36 You have a mucosa lined by epithelium. So, it's on loose connective tissue. 00:41 And then, deep to that is more stiff and more firm submucosa connective tissue. 00:46 And then, there's a muscularis propria in two layers around the outside of the bowel. 00:52 And then, outside of that is the serosa. And finally, we get into the peritoneal cavity on the outside. 00:59 A true diverticulum just to make a point is all three layers of the bowel pouching out. 01:07 And when we talked about esophageal diverticula in other talks, some of those were involved with pouching out of all three layers. 01:15 But if we only pouch out a couple of the layers because of incomplete layering of the, say, muscularis propria, then, we have what is called a pseudodiverticulum. 01:27 This is for people who want to be absolutely specific with their language. 01:33 But when we talk about colonic diverticulosis, we don't usually make the distinction. 01:40 I will say that the vast, vast, vast majority of them, 99.99% are pseudodiverticula. 01:48 Let's do some of the epidemiology. As I said, this talk is going to be mostly about colonic diverticulosis and diverticulitis. 01:57 There's a reasonably high prevalence of diverticulosis, outpouching of the wall, in the colon in the adult population. 02:09 And about 20% or so will have it by the age of 40. By the age of 60, about 60% of people will have some diverticulosis. 02:20 Now, that doesn't mean they're going to have inflammation but it means that they've got the predicate. 02:24 They've got the initial step that can lead to inflammation. 02:28 As is indicated there here, diverticulosis is much more prevalent in countries with a western diet that's associated with constipation and straining at stool and as we're going to see, that's the major kind of structural reason why we get diverticulosis. 02:44 5% of patients with diverticulosis will develop inflammation of the diverticula and once you've had inflammation of that, that will recur with a reasonably high rate, about 20% within the next five years. 03:01 So, the things that are associated epidemiologically with diverticulosis. 03:05 and then, associated also with diverticulitis include obesity, physical inactivity, a low fiber, high fat, high red meat diet and genetic disorders where we have abnormalities of connective tissue, Marfan syndrome, Ehlers-Danlos syndrome, Scleroderma. Smoking is also associated. 03:30 Clearly, there are - smoking is associated with many other things but it is also associated with diverticulosis. 03:39 The pathophysiology. The reason that this happens much more frequently and the reason that we are dealing with the pseudodiverticula is that the inner circular layer of the colon is complete. 03:52 It goes all the way around, it wraps around. The outer longitudinal layer of the colon however, gets reduced not to a continuous layer all the way around but to three strands equally spaced around the colon. 04:05 Those are the so called taenia coli and you see them indicated here. 04:10 So, that means that there are portions of the colon, large segments of the colon around the circumference that don't have that outer longitudinal layer of smooth muscle and those are relatively weak spots where the vessels can come in and that's where the diverticuli will occur. 04:29 So, if we have colonic dysmotility and we have increased intraluminal pressure and/or structural weakness, we will get outpouching. But note, it doesn't have all three layers, so, that's why it's a pseudodiverticulum. That pseudodiverticulum is in a territory, there's lots of bacteria where there's stool and a combination of stool and mucus and sloughed epithelium can all impact at the neck of this diverticulum. And then, more distally, we can't have normal drainage. 05:04 Not only that, the bacteria are happily fermenting whatever was in there and we're getting progressive expansion of that pseudodiverticulum. 05:14 So, a fecalith that impacts bacterial overgrowth will eventually lead to vascular compromise. 05:20 The vessels that are perfusing that part of the bowel get squeezed with the increased intraluminal pressure within the diverticulum. 05:29 And now, you don't get adequate profusion and we get ischemia and potentially, perforation. 05:34 That's what goes on with acute diverticulitis. So, very simple, that is to say, uncomplicated diverticulitis occurs in the majority of people who are going to get the inflammation. 05:44 It just means that the diverticulum is inflamed. We typically can treat that with fluids and antibiotics. 05:50 Complicated diverticulitis on the other hand is associated with an abscess formation which we have frank necrosis with a free perforation or with fistulous tract formation and that's what's being demonstrated. 06:02 So, the upper panel shows an abscess, a big phlegmon associated with a diverticulum. 06:07 And the bottom panel shows a fistulous tract between a pseudodiverticulum and the bladder. 06:14 The clinical presentation for diverticulosis, you don't know you have it. 06:18 Although, if you're 60 years old, 60% of you will have it. So, it's very common but usually, asymptomatic. 06:24 Diverticulitis on the other hand will present with pain in the abdomen and it's more so in the left lower quadrant versus the right lower quadrant. 06:33 Why is that? Well, left lower quadrant is where the sigmoid colon is. 06:37 And in fact, diverticulosis tends to be more common, more distally within the colon. 06:42 So, sigmoid colon has got more diverticulosis typically than does the ascending colon, than does the transverse colon, than does the descending colon. 06:52 That's why you more frequently have the pain in the left lower quadrant. 06:56 Patient may have constipation or diarrhea, fever, nausea, and vomiting, rebound tenderness, all the typical things you associate with inflammation of the bowel. How do we make the diagnosis? So, in terms of a formal diverticulitis, we make the diagnosis with a white cell count with a left shift, elevated inflammatory markers like C-reactive protein. We would do a CT which is a test of choice and we'll show focal colonic wall thickening. Hopefully, we don't see an abscess formation. 07:28 Hopefully, we don't see a fistulous tract. You may see evidence though of microperforation. 07:33 Ultrasound and MRI can also be used and colonoscopy can also be used but CT is the way to go. 07:41 And this is just imagery on CT how we can see the diverticula outpouching in this particular setting. 07:48 And if there was associated edema, associated wall-thickening, then, we can make the diagnosis of diverticulitis. 07:54 The panel on the right-hand side is just showing you the gross appearance of these little outpouchings. 07:59 How do we manage this? So, diverticulosis, there's really nothing to be done. 08:05 You can try to minimize the degree of diverticulosis by changing the dietary habits. 08:10 So, more fiber, less red meat, less fat, more activity, quit smoking, lose weight, the usual litany of things we want our patients to do. But we can't ever revert the existing diverticula. 08:26 Diverticulitis on the other hand, we might want to treat in most cases, the uncomplicated cases, with a clear liquid diet and some antibiotics that usually causes resolution. 08:36 But recall that about 20% of patients, once they've had diverticulitis once will get it again within five years. 08:43 If there's a lot of bleeding associated with the diverticulitis, we can do endoscopic hemostasis. 08:48 We can go up through the rectum to the point where we identify a bleeding site and zap it. 08:54 And in some cases, we may actually have to progress to surgical colectomy where there's just intractable inflammation or intractable inflammation that has led over time to scarring or a fistulous tract, or atresia, or stenosis. 09:09 And in those cases, we have to remove that segment of the colon. And with that, diverticulosis and diverticulitis, the diverticular diseases.
About the Lecture
The lecture Diverticulosis and Diverticulitis by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is the outermost layer of the bowel?
- Serosa
- Muscularis propria
- Submucosa
- Mucosa
What defines a true diverticulum?
- Outpouching that includes all layers of the wall
- Outpouching that includes one layer of the wall
- Outpouching involving only one part of the colon
- Outpouching involving multiple parts of the colon
- Outpouching that persists after treatment
What diet is associated with diverticulosis?
- Western diet
- Gluten-free diet
- High-fiber diet
- Low-carbohydrate diet
- High-protein diet
Where is the most common location of pain from diverticulitis?
- Left lower quadrant
- Left upper quadrant
- Right lower quadrant
- Right upper quadrant
- Epigastric region
What is the management of diverticulosis?
- Dietary changes
- Clear-liquid diet
- Oral antibiotics
- Endoscopic hemostasis
- Surgical colectomy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |