Playlist
Show Playlist
Hide Playlist
Distal Convoluted Tubule (DCT): Gitelman Syndrome
-
Slides DCT Pathophysiology RenalPathology.pdf
-
Download Lecture Overview
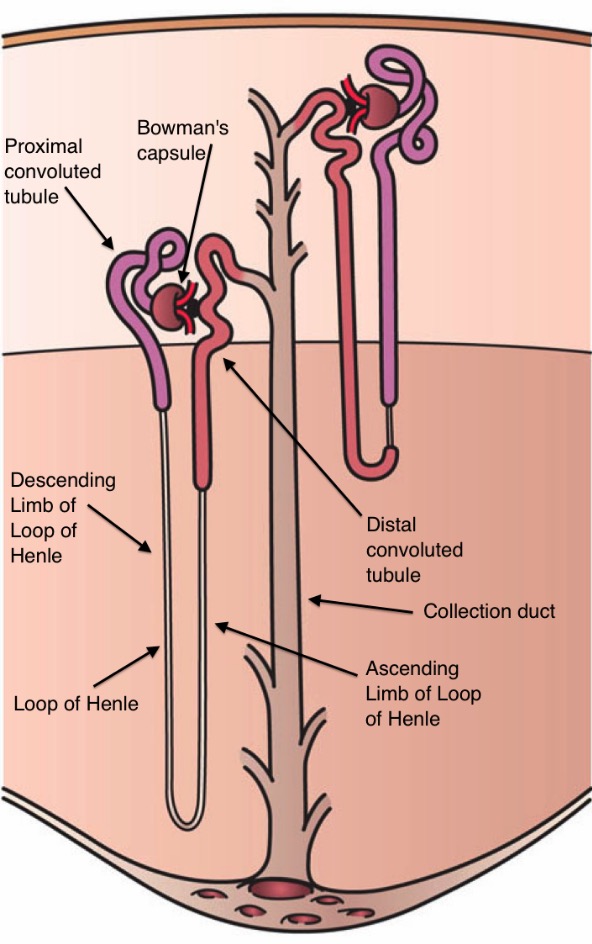
00:01 Okay. Let us talk about Gitelman syndrome here obviously. Distal convoluted tubule, the problem has nothing to do with your sodium- potassium-2 chloride, does it? No. Gitelman will be dealing with your sodium and chloride channel. Now what is interesting about this? Take a look at the name. Hypomagnesemia. Correct Losing magnesium. Hypokalemia, losing potassium correct. However, this is the big thing. 00:27 It is hypocalciuria. Now understand that Gitelman syndrome is much more common than Bartter granted, but know both for any of your exams. So here in Bartter syndrome, there was hypercalciuria and in Gitelman, it will be hypocalciuria. In Bartter syndrome, there is an issue with concentration of your urine and Gitelman not so much, but both will have issues with diluting. 00:56 So these are things that you want to keep in mind when distinguishing one from the other. 01:02 Continue. Autosomal recessive, there is the actual gene, SLC12A3, gene product of NCCT. In other words think about the sodium chloride channel. Thiazide sensitive. T think thiazide at least be able to identify that. You end up having this pretty much the same issue except for one big thing. Hypokalemia present in both Bartter and Gitelman, metabolic alkalosis both in Bartter, in Gitelman, hypomagnesemia both. Hypocalciuria. Whereas in Bartter get hypercalciuria resulting in secondary hypoparathyroidism. Normal blood pressure. It contracts the lateral two findings meaning the calcium and the blood pressure to Bartter and exactly the point that we made. Now Gitelman usually diagnosed until late childhood or adulthood whereas in Bartter childhood we did antenatal. Remember the prostaglandin levels, They're quite high in Bartter more so hence the indomethacin an COX inhibitor. In Gitelman, it is not so much concentrating ability whereas ability to properly dilute. Hence the ADH will be suppressed, but that is pretty much in both. 02:23 Cramps of the arms and legs due to hypokalemia, muscle weakness. What happens to resting membrane potential? One more time it becomes more negative. You are further away from the threshold. So, therefore, more difficult to trigger an action potential. Welcome to fatigue. Maybe perhaps tetany, polyuria, nocturia that is pretty big in Gitelman. Approximately 80 percent of your patients could have nocturia. That is amazing. Now why in Gitelman more so than Bartter? I couldn’t exactly answer that for you, but look for this clinically because we know it occurs. Chondrocalcinosis due to chronic hypomagnesemia interesting concept, unexpected hypertension may present later. Keep that in mind. However, you have enough information now to distinguish between Gitelman and Bartter. Please don't miss these questions. It is all here. Go back and review. I would say if you have never heard of these before that you keep going over them a few times. If you have reviewed and now you should be able to add in little bit more information where you truly able to understand these conditions. Here once again for the most part potassium sparing ACE inhibitor sometimes with Gitelman, you will have increased prostaglandin. I can’t say for sure that you wouldn’t with Gitelman. I would not be doing justice. Clinically speaking both Gitelman and Bartter have shown an increase in prostaglandin, but more so in the Bartter that we talked about. Sites of drug action, we talked about the thiazide. This would be up in your distal convoluted tubule and this would be more about your Gitelman. Remember the name of the gene there with NCCT, sodium chloride and thiazide sensitive type of area. With thiazides, it works in the distal convoluted tubule. 04:16 If both patient populations mean to say you have your African and elderly who have hypertension often times being the main stay of therapy and important, Thiazides behave like PTH. 04:32 So if your patient does have hypercalciuria, what kind of diuretic would you want to avoid? Loop. 04:38 Because loop would make the hypocalciuria worse. Thiazide would be used to perhaps remove the calcium from the urine. Please highlight in your mind. Calcium renal stone formers. 04:51 The drug attaches chloride and by doing so is able to then reabsorb the calcium. 05:00 Now there is a lot more mechanics to it beyond the scope of your exams at this point, but clinically speaking if you are thrown any question about thiazides or Gitelman on the distal convoluted tubule, you shouldn't miss them if you are comfortable with it, welocme it. Thiazide, hyponatremia due to loss of your sodium. Electrolyte abnormality includes your hypokalemia, metabolic alkalosis. Now hypercalcemia is an uncommon complication. Keep that in mind clinically, please. So even though you know thiazides remove calcium from the urine and so, therefore, those patients that you worried about hypercalciuria genetically or maybe due to let us say calcium stones or what not, you are not going to have so much calcium that results in hypercalcemia. I can tell you that comfortably. Uncommon. More likely if the patient has primary hyperparathyroidism for obvious reasons if the patient is already in a state of primary hyperparathyroidism that we talked about and use thiazide. Of course, you might be exacerbating issue that is something that you do want to keep in mind.
About the Lecture
The lecture Distal Convoluted Tubule (DCT): Gitelman Syndrome by Carlo Raj, MD is from the course Diseases of the Nephron.
Included Quiz Questions
Which of the following symptoms is commonly found in with Gitelman syndrome?
- Nocturia
- Mental retardation
- Hyperventilation
- Hypertension
- Sensorineural deafness
Which of the following electrolyte disorders leads to the development of chondrocalcinosis in Gitelman syndrome?
- Hypomagnesemia
- Hypermagnesemia
- Hypocalcemia
- Hypercalciuria
- Hypernatremia
Which of the following features would suggest the diagnosis of Gitelman syndrome rather than Bartter syndrome?
- Hypocalciuria
- Hypomagnesemia
- Hyperprostaglandenemia
- Hypokalemia
- Hyponatremia
Which of the following is common to Gitelman and Bartter syndromes?
- Hypokalemia, metabolic alkalosis, and hypomagnesemia.
- Hypokalemia, metabolic alkalosis, and hypermagnesemia.
- Hyperkalemia, metabolic alkalosis, and hypomagnesemia.
- Hypokalemia, metabolic acidosis, and hypomagnesemia.
- Hypokalemia, respiratory alkalosis, and hypomagnesemia.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |