Playlist
Show Playlist
Hide Playlist
Differentiation of Ulcerative Colitis and Crohn Disease
-
Slides GIP Differentiation of Ulcerative Colitis Crohn Disease.pdf
-
Download Lecture Overview
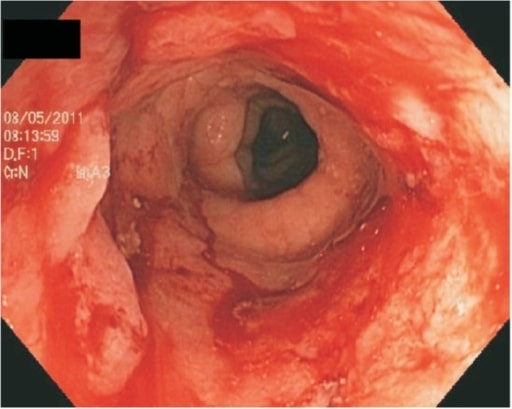
00:00 Welcome. If you've been following along with the other videos, you've probably already watched Crohn's Disease and Ulcerative Colitis separately. 00:11 But for many medical students, it's a little bit confusing how are they similar, how are they different, how do I tell them apart? So, we're going to have just one relatively brief talk that's just about comparing the two, so you can hopefully get them straight in your own mind. 00:26 So Crohn's Disease and Ulcerative Colitis are two separate flavors of inflammatory bowel disease. 00:33 This is chronic inflammation of the digestive tract, a very different kind of distributions, different causes, and sometimes, different manifestations. 00:44 Let's go first to the pattern of involvement because that's a major difference between the two different entitles. 00:49 So, the two different flavors, Crohn's Disease and Colitis have very different distributions. 00:56 Crohn's Disease is characterized by skip lesions that can occur anywhere in the GI tract from mouth to anus. 01:05 Now, they will most commonly involve the terminal ileum and the proximal colon but they can be anywhere. 01:11 Classically, they don't involve the rectum. But in some cases, you may find it there. 01:17 But keep in mind, it's little focal lesions. So, it's not one long segment of bowel. 01:24 On the other hand, ulcerative colitis. 01:27 They are continuous lesions that begin in the rectum and move anterograde, so, kind of backwards. 01:33 And so, initial ulcerative colitis may only involve the rectum. And with time, you may get into the sigmoid colon. 01:41 And then, into the descending colon. And then, the transverse colon. 01:44 And in very severe long-standing disease, you may get all the way over to the cecum. 01:49 Let's talk about the symptomatology because you would think, "Gee, inflammation in the GI tract is going to give you the same outcome. 01:56 Not entirely. So, in Crohn's Disease because it's very focal and it's kind of scattered throughout, you will get crampy abdominal pain because the inflammation causes spasming of the smooth muscle of the bowel. 02:10 So, that would hurt. But it's usually a diarrhea that is non-bloody unless you have a lot of involvement of many parts of the bowel. 02:18 In ulcerative colitis, you get that same cramping abdominal pain. It is again, inflammation causing spasm of the smooth muscle. 02:26 But you'll tend to get more of a bloody diarrhea. Ulcerative colitis causes sloughing of the mucosa, the epithelial layer that ulceration will expose blood vessels right underneath and they will tend to bleed. 02:41 And because they're bleeding in the colon, you may see bright, red blood. 02:46 So it's more of a bloody diarrhea. Both patients may present with mucous. 02:51 It's more common to see mucous production associated with inflammation in ulcerative colitis. 02:57 And again, this has to do with the continuous legions over long frequency or long period of the bowel. 03:04 And the stool frequency tends to be much more voluminous and more frequent with ulcerative colitis than Crohn's Disease. 03:13 And again, this has to do with the fact that the colon, normally would be responsible for absorbing in water, if it's not doing its job, you're going to have a lot of water in the colon that is being evacuated and you'll feel like you have to go much more frequently. 03:30 The extraintestinal manifestations are actually fairly comparable between the two entities and have not separated them out here in terms of ulcerative colitis or Crohn's Disease. 03:41 But there are cutaneous manifestations. 03:42 This is erythema nodosum and pyoderma gangreosum and pictures of that were present in the other talks on the individual diseases. 03:51 You may get inflammation of the eye or uveitis. Apthous ulcers, painful ulcers occur in both. 03:58 Arthritis and osteoporosis may occur in both and the osteoporosis is largely due to a vitamin D malabsorption and/or calcium. 04:10 And then, both may present with anemias although, they don't have to. 04:13 Both entities will get cholelithiasis and nephrolithiasis. 04:19 In some cases in - or many cases, this is due to abnormal absorption of the building blocks for those - or for abnormal absorption of fat. 04:31 I will say that in ulcerative colitis, primary sclerosing cholangitis is more commonly seen than it is in Crohn's Disease. 04:41 The complications of both. Both can manifest with gastrointestinal bleeding. 04:47 As a result of that, you may have varying degrees of anemia. 04:50 Both may give rise to intestinal perforation. 04:53 It's usually a little bit more common in cases of Crohn's Disease where you get a fistula tract formation. 05:01 And with increased bowel spasm or inflammation and scarring, both maybe give rise to bowel obstruction. 05:11 Now, separating left and right. 05:15 On the left-hand side are going to be things that are more commonly associated with Crohn's Disease. 05:21 So, fistula tract, malabsorption, perianal fissures and fistulas. 05:27 So, transmural inflammation is a much more common finding in Crohn's Disease. 05:33 And with that transmural inflammation, you're going to be more prone to getting complete erosion all the way through all layers of the bowel. 05:41 And when that bowel sits up against other bowel, you may get a fistula. 05:45 When it sits up against a bladder, you may get a fistula into the bladder or into the skin. 05:50 On the other hand, the inflammation and the just mucosal involvement that occurs in ulcerative colitis gives rise to the findings seen on the right-hand side. And toxic megacolon. 06:04 So, having a colon that is so diffusely ulcerated that you get inflammation in - not causing spasm but causing a complete dilation of the colon. 06:16 Fulminant colitis where there's inflammation from beginning to end and there's a much greater incidence of malignancy in ulcerative colitis. 06:27 The individual lesion in regional enteritis or Crohn's disease tend to be spotty. 06:31 They come and they go. So, you don't have chronic, ongoing inflammation and epithelial reduplication, replication going on all the time. 06:41 On the other hand in ulcerative colitis, you do. 06:46 And any segment that's involved will have chronic inflammation, chronic epithelial regeneration and the combination of those two is a setup for cancer. 06:56 So, colorectal cancer is much more common, commonly associated with ulcerative colitis. 07:01 The microscopic findings are also classically differentiated. And these may show up on board exams, so pay attention a little bit. 07:09 On the left-hand side is Crohn's Disease and the classic finding that we associate with Crohn's is a non-caseating granuloma. 07:18 We will also see lymphoid aggregates. We will see transmural inflammation. 07:22 We will see some fibrosis. We may see lymphatic dilation. 07:26 But it's the presence of that non-caseating granuloma that you need to keep in the back of your head. 07:32 For ulcerative colitis, it's mostly mucosal inflammation. It doesn't go deep. It doesn't have the fistulas tracts. 07:38 You tend to have increased inflammatory cells within the lamina propria. You will have epithelial erosion. 07:45 That's the ulceration and you may have metaplasia of the epithelial cells but no granulomas and no lymphoid aggregates and no fissures. 07:55 Finally, the treatment. And the treatment pretty much is the same for both. 08:01 So, we will give things that will beat down inflammation, corticosteroids and immunomodulators and anti-tumor necrosis factor agents. 08:10 We will also give antibiotics in both cases because that changes the microbiota and in many cases, that may influence the antigens that are ultimately being presented that are driving the inflammatory process that underlies inflammatory bowel disease. 08:25 For ulcerative colitis, we probably, especially with longstanding severe disease, we probably want to do a colectomy. 08:35 That's because of the increased risk of cancer. For each decade that someone with ulcerative colitis has the disease, there's a 10% risk of malignancy in the involved segment. On the other hand, you wouldn't tend to do a colectomy at all in Crohn's Disease. 08:54 The risk of adenocarcinoma is very marginally increased but when you have areas of stricture or when you have areas of fistula tract formation, you may have to do a focal bowel resection. 09:06 And with that, hopefully, we've clarified some of the differences and some of the similarities between Crohn's Disease and ulcerative colitis.
About the Lecture
The lecture Differentiation of Ulcerative Colitis and Crohn Disease by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
Which of the following is true about Crohn disease?
- Skip lesions may occur from the mouth to the anus.
- Skip lesions may occur only from the esophagus to the rectum.
- Lesions most commonly involve the gastric cardia.
- Lesions most commonly involve the gastric fundus.
- Lesions classically involve the rectum.
Which of the following is NOT a typical presenting symptom of Crohn disease?
- Bloody diarrhea
- Non-bloody diarrhea
- Crampy abdominal sensation
- Pain
- Mucus
Which condition is more commonly seen in ulcerative colitis?
- Primary sclerosing cholangitis
- Cholelithiasis
- Uveitis
- Osteoarthritis
- Anemia
Which complication is more commonly seen in ulcerative colitis than in Crohn disease?
- Colorectal cancer
- Fistula
- Malabsorption
- Perianal fissure
Which finding is consistent with Crohn disease?
- Non-caseating granuloma
- Mucosal inflammation
- Th2 cell proliferation
- Epithelial erosion and ulceration
- Epithelial metaplasia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |