Playlist
Show Playlist
Hide Playlist
Diarrhea: Pathophysiology and Clinical Presentation
-
Slides GIP Diarrhea.pdf
-
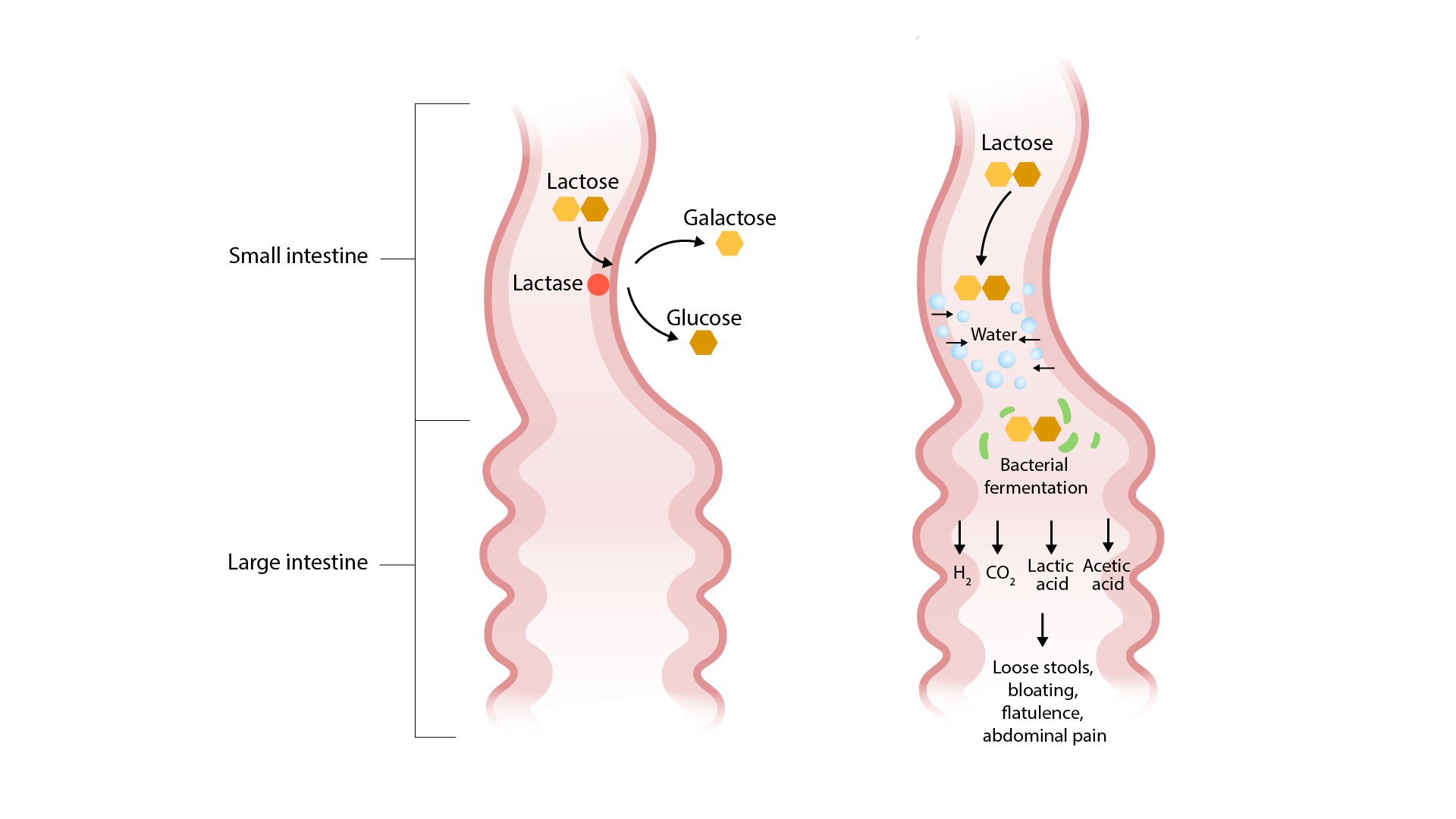
Download Lecture Overview
00:01 Let's get into some of the pathophysiology. So, when we're talking about inflammatory or invasive diarrhea, we're talking about a particular infectious organism that has learned the trick about how to invade into and beyond the epithelium of the GI tract This is just a schematic. They kind of give you a sense of what's going on there. 00:22 We have our particular invasive organisms sitting out in the lumen. 00:26 It can then invade across, can infect, and then invade across the epithelium. 00:33 And once it gets into the subepithelial mucosa into the lamina propria, will elicit a very profound inflammatory response that involves neutrophils and macrophages and T-cells. 00:45 With the initial invasion, we often get killing of the epithelium and the inflammatory cells will also cause some additional damage. 00:55 So, there's a lot of collateral injury that associated - is associated with that. 00:59 And then, in the setting of these organisms, we get mucus, blood, and lymphocytes detectable within the stool. 01:06 Of the non-inflammatory/non-invasive infectious diarrheas, what's happening are the pathogens don't invade But they make, for example, enterotoxins that will cause the efflux of ions water and can also primarily cause the epithelium to become malabsorptive, it cannot absorb nutrition appropriately. 01:27 In this setting, most of these lead to a watery diarrhea that typically lacks leukocytes and blood. 01:35 So, we haven't damaged the epithelium. We've just made it dysfunctional. 01:39 And examples of this include cholera, and giardia, and rotavirus. 01:44 This is just an example. In other places within the series of pathology talks, we cover, for example, cholera in particular. 01:54 But this is just the schematic. So, we have bacteria that are in the gastrointestinal lumen elaborating toxins not otherwise specified. 02:03 Those toxins can be translocated into the cytosol of the epithelial cells. 02:10 In that location, those toxins, which can also include viruses, certain medications can do this, serotonin can do this, will influence the production, for example, of secondary signals such as cyclic AMP. 02:27 The cyclic AMP in turn then will impact or act on the CFTR, the cystic fibrosis transmembrane conductance regulator. 02:36 And now, we'll get an efflux of chloride. 02:38 That chloride ion as it's being pumped out of the cell will then suck along with it in a para-cellular way, sodium, because we have to have ionic balance. 02:50 But then, sodium chloride being pumped out will lead to then an osmotic pull of water. 02:56 And now, we'll have a watery diarrhea. Note, the epithelium, perfectly intact. 03:01 No inflammation is being involved here. But we are getting a rather profound secretory diarrhea. 03:08 So, we understand for the kind of secretory diarrhea that's associated with infections why we're getting a watery diarrhea. 03:16 But water can also be drawn into the intestinal lumen if we are not absorbing certain substances. 03:22 So, for example, in lactose intolerance, we cannot break down the lactose. It can't be absorbed. 03:30 And that lactose acts as an osmotic force to draw water into the lumen. 03:35 In situations such as that, the stool output is pretty much commensurate with the amount of unabsorbed material. 03:43 Importantly, not only are we pulling water into the lumen, but all that unabsorbed material, that's a fertile kind of environment for bacteria to expand. 03:55 So, when this is happening, we will often get secondary bacterial expansion and fermentation creating gas. 04:05 So, the important thing about recognizing this form of malabsorption or osmotic diarrhea is that we fix it by getting rid of the offending agent. 04:18 So, for example, lactose intolerance, celiac disease caused by a gluten sensitivity and certain peptides called gliadin, short bowel syndrome where we're not able to absorb certain nutrients. 04:33 We can – if we recognize that as a cause, we can often intercede and fix it. 04:41 This is just giving you a schematic of what this looks like. 04:44 So, this is an example of lactose intolerance in an individual that lacks lactase, you cannot break the lactose down into a galactose and glucose which is a necessary step to get absorption. 04:55 The lactose stays in the lumen. It pulls water in osmotically and bacteria go, "Yum, lactose." And they metabolize it. That fermentation leads to the production of hydrogen ions, carbon dioxide. 05:09 It can also make methane. 05:11 So, everything that you would expect to happen with bacterial fermentation and you get very loose stools. 05:17 You get a lot of bloating. You get flatulence. You get a lot of secondary manifestations of the bacterial fermentation. 05:25 Okay. Of the inflammatory or exudative forms of diarrhea, these would be the ones associated with inflammatory bowel disease, Crohn's and Ulcerative Colitis. Inflammation, a primary auto-immune inflammation leads to intestinal mucosa damage. 05:41 Clearly, if the intestinal mucosa is not happy or is not present, you're going to get impaired absorption. 05:47 In this setting, because you've damaged the mucosa and you have lots of inflammation, we will again see mucus and blood, and leukocytes. 05:55 So, simply finding blood, mucus and leukocytes doesn't equal an infectious diarrhea. 06:00 There can be a primary, for example, autoimmune diarrhea. This is just now a schematic of what this can look like. 06:08 So, here, we have our normal epithelium. This is representative of small bowel epithelium with Paneth cells. 06:14 Paneth cells are not present in other places in the GI tract other than small bowel. 06:20 We have on the lumen, we have normal microbiota. 06:26 Because of the inflammation that's associated with the inflammatory bowel disease, Crohn's or Ulcerative Colitis, we are getting an inappropriate activation of pro-inflammatory T-cells. 06:40 So, activated macrophages and activated dendritic cells will stimulate T-cells, will present antigens, stimulate T-cells, so, they become activated, elaborating more mediators, cytokines, reactive oxygen species, etc. 06:55 which will lead to further activation of macrophages and dendritic cells. It gets to be a vicious cycle. 07:00 The inflammatory mediators that get made by these cells will then cause defects in the epithelial cell interactions and will also cause loss of the normal villar architecture so they're not getting good absorption. 07:17 All of these things will lead to a profound diarrhea but also with leakage of inflammatory elements into the lumen. 07:27 Final category of increased motility. So, again, this kind of makes sense. 07:32 Everything could be working just fine and there's no other problem. 07:37 There's nothing infectious but if we're just moving too fast from top to bottom, we don't have enough time for adequate absorption. 07:45 And examples of this include hyperthyroidism and irritable bowel syndrome. The clinical presentation. 07:52 Again, thinking about whether it's acute or persistent or chronic. 07:57 So, we'll need to kind of separate things into those categories because we think differently deepening on which of those we're talking about. 08:04 We're also going to need to think about the type of diarrhea. 08:08 Is it watery? Does it got bulky, slimy, fatty, foul-smelling stools? Bloody? Is it watery? Does it got bulky, slimy, fatty, foul-smelling stools? Bloody? Is it watery? Does it got bulky, slimy, fatty, foul-smelling stools? Bloody? Which makes it likely to be inflammatory. Is it mucoid? Likely to be inflammatory. 08:20 Are there systemic manifestations? So, fever tends to suggest that there is going to be something pro-inflammatory. 08:28 It might be infectious or primary inflammatory bowel disease. 08:31 Abdominal pain and cramping will tend to suggest that there's more either inflammation, or we have metabolism and fermentation of material within the GI tract. 08:42 Flatulence and bloating definitely suggests that we have an abnormal content of material within the lumen that bacteria can ferment. 08:52 Nausea and vomiting can happen with all variety of diarrhea causes but especially, Nausea and vomiting can happen with all variety of diarrhea causes but especially, associated with infection or toxin-mediated diarrheas. Tenesmus which is straining at stool. 09:06 So, you just feel like you have to go and you strain and nothing comes out It can suggest various entities. 09:14 Secondary manifestations. So, dehydration. If you pull up the skin normally on a person, that skin goes right back down. 09:21 I am well-hydrated. But in your patient who is dehydrated, you pull it up and the skin stays tented. 09:28 They will also have dry mucous membranes. They will likely be tachycardic. 09:33 Again, because they are volume depleted. If there's malnutrition because of malabsorption, then, you would expect vitamin deficiency. 09:43 They may be anemic either from folate B12, or iron, and clearly, there will be weight loss.
About the Lecture
The lecture Diarrhea: Pathophysiology and Clinical Presentation by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
Which type of diarrhea is often associated with nausea and vomiting?
- Infectious
- Vitamin deficiency
- Steatorrhea
- Bacterial overgrowth
- Pseudomembranous colitis
What signaling molecule increases in diarrhea mediated by a toxin?
- cAMP
- cGMP
- EGFR
- ATP
- MGMT
What is a symptom of dehydration?
- Tachycardia
- Anemia
- Nausea
- Vomiting
- Tenesmus
What is the most common cause of acute diarrhea?
- Infection
- Vitamin deficiency
- Bacterial overgrowth
- Electrolyte loss
- Pseudomembranous colitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |