Playlist
Show Playlist
Hide Playlist
Diagnosis: Overview – Lung Disease
-
Slides 06 Respiratory Medicine Basics Brown.pdf
-
Download Lecture Overview
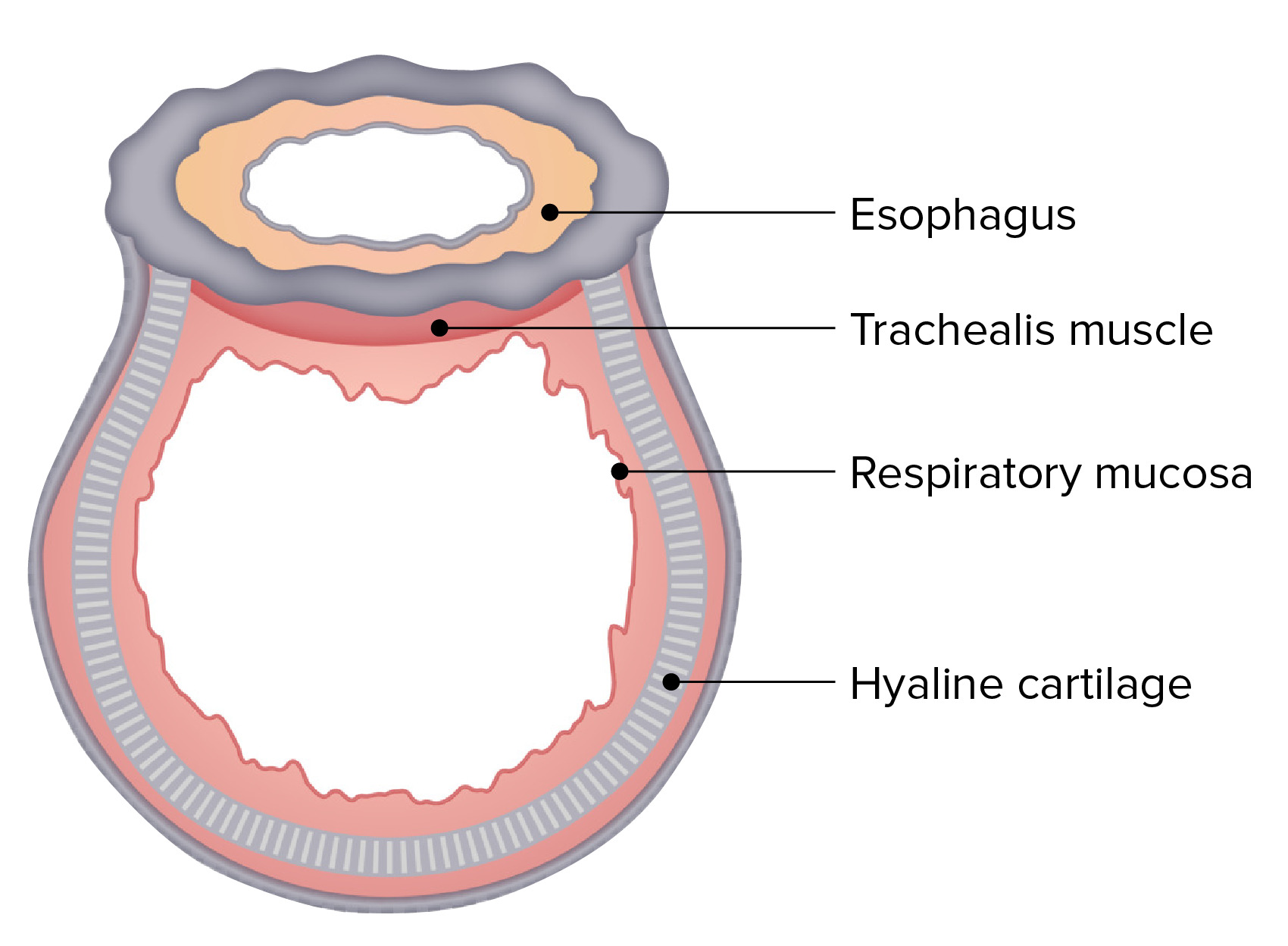
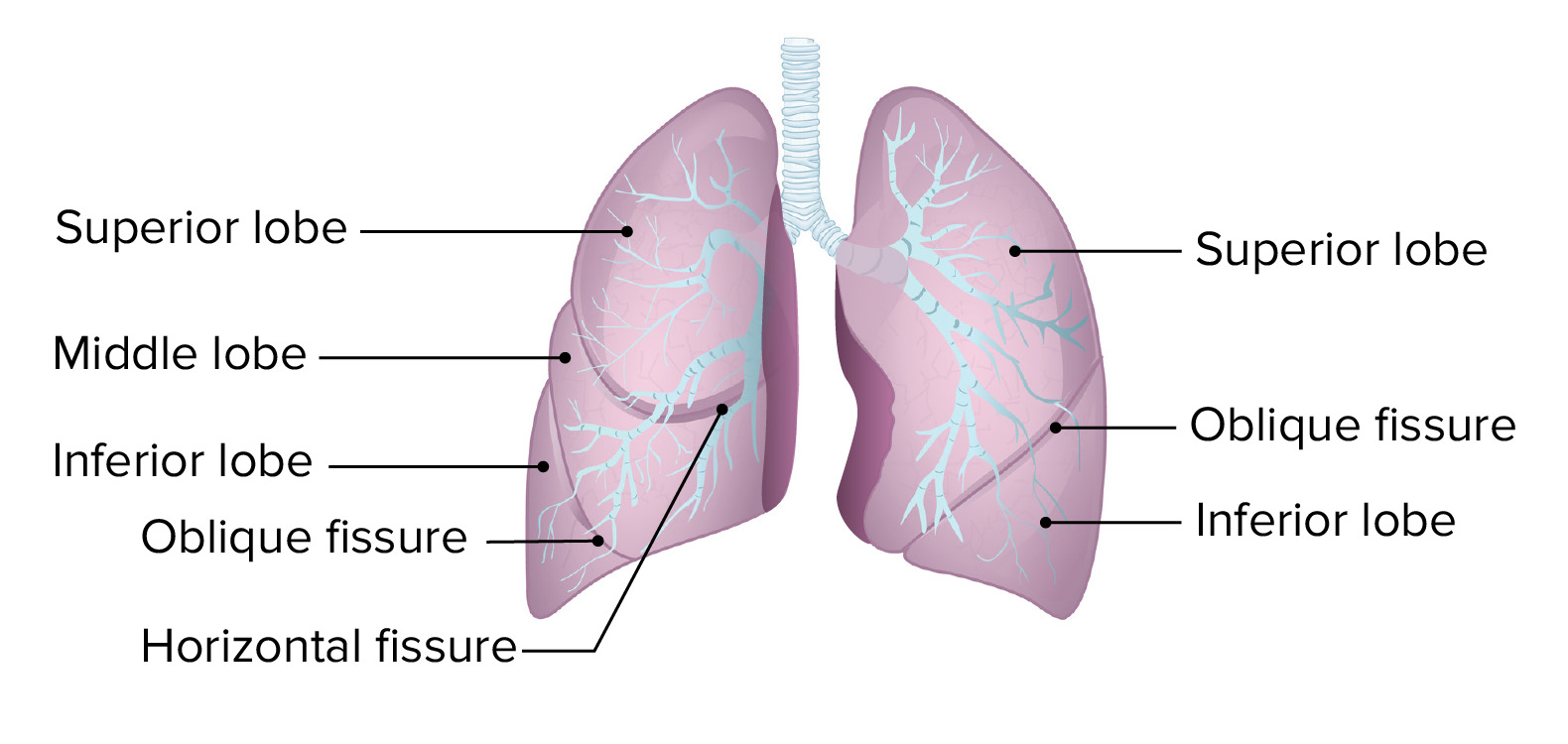
00:01 The subject of this lecture are the investigations that we use for assessing patients who are presenting with potential lung disease. 00:07 And I’m going to concentrate this lecture on the interpretation of how we use lung-function tests to assess patients with respiratory problems. 00:17 Why do we use diagnostic tests? Well, in effect we don’t use diagnostic tests if it’s only mild disease and the clinical assessment makes it clear what the problem might be. 00:25 But with more complex disease, more severe disease we will need diagnostic tests. And we need those for different reasons. One is to confirm the suspected diagnosis. Two is to make sure we’re not missing an alternative diagnosis we hadn’t thought about. The third is to assess how severe that diagnostic is, how badly affected the patient might be by that disease. And fourthly, we use diagnostic testing to establish the baseline data so we can monitor the progression of the disease over time. 00:54 There are some important things that a clinician needs to understand about diagnostic testing before using them. The first is that you need, in your own mind, to define the question that you’re asking the test to answer. 01:10 So, for example, somebody presenting with pneumonia – well I think it’s clinically pneumonia. I do a chest X-ray to see whether there is consolidation present and therefore confirm that they have pneumonia. 01:23 And the choice of which test you do is clearly going to be dictated by the clinical scenario. 01:28 So patients presenting with suspected airways disease, it’s the lung-function tests which are important. But if somebody’s got cancer or potential cancer, it comes down to imaging and obtaining a biopsy of the abnormal area to see whether there is a cancer or not. 01:45 The third factor we need to remember is that interpretation of a test result is dependent on the clinical assessment. 01:54 So this is an X-ray that shows right shadowing. It looks like alveolar shadowing so that is potentially consolidation. And so if somebody is representing with a three-day history of cough, fever and is hypoxic, this X-ray will confirm that they have pneumonia. 02:09 However, if this patient has a several-month history of cough, no fever and not much in the way of hypoxial breathlessness, then this isn’t a pneumonia. This is some other problem. 02:20 And that requires a further different range of investigations than if the patient has pneumonia. 02:27 There are two parameters which we use to describe how good a test is. One is sensitivity and the other is specificity. 02:34 So sensitivity is the proportion of people with the disease who will test positive. That is how good is that test at identifying somebody with that disease. 02:44 Specificity is the proportion of people with positive results who actually have the disease. 02:51 So many tests, you do them and they reflect somebody who has a disease but, actually, they can also be abnormal in people who don’t have the disease. 03:00 So specificity is how often a test, when it’s positive, means the patient has that disease. 03:07 The likelihood the test has actually identified somebody with the disease. 03:10 And, in general, no test is 100% sensitive or 100% specific. And this needs to be borne in mind when interpreting the results. 03:20 And this needs to be combined with the pre-test probability of the disease being present. 03:26 And what I mean by that is that: is it likely from the clinical assessment that that patient has that disease? Because then that makes the test much more useful. 03:38 So, for example, if we have a test which has 95% specificity and 90% sensitivity, that means every time you use the test, for twenty people there’ll be one false positive and there will be two people with the disease where the test is negative. So 10% of patients with the disease will have false-negative results. 04:01 Now, if you apply this test – and you wouldn’t as you can see from the data that’s coming up – as a screening test for a disease in a population of otherwise normal people, the disease may only be present in 1 person in every 10,000. So you test 10,000 people and 1 person will be positive. They’re likely to come up positive with the result because the test will identify them. However, there will be 9,999 × 0.05 false-positive results – people who give a positive result who don’t have the disease. So essentially for every person you identify with the disease, there’ll be nearly 500 people who have a positive results who don’t have the disease. That test is essentially useless as a screening device. 04:54 Right. Now the tests that are available for respiratory disease can do various things. 05:02 One is that we can measure physiological function. And that’s basically the lung-function test but it also includes blood gases, sleep studies and some of the radioisotope scans are really functional assays for the patient. And we often use echocardiograms in patients with lung disease to make sure they don’t have cardiac disease as an alternative diagnosis and to assess for the presence of cor pulmonale etc. 05:23 Two: we can assess the lung anatomy and that’s basically radiology. X-rays, CT scans, ultrasounds, MRI but it also includes the bronchoscopy, which is where we pass a flexible tube with an endoscope on the end down through the windpipe down into the lungs and actually visualise the airways directly. 05:39 Three: we can obtain samples for histological and cytological examination in the laboratory. 05:46 And those samples can be attained by different methods and will give us an opportunity to confirm exactly what the diagnosis is. And these tests are particularly important for patients with lung cancer. 05:57 Four: if somebody’s got an infection, we can look for the pathogen. We do microbiological tests: sputum, blood, pleural fluid can all be cultured to see whether there is a bug present. 06:08 Then we do have various tests for immunological status. Those are normally blood tests or skin-prick testing. And then there are other blood tests for general health. And importantly we can actually measure the level of inflammation present in somebody presenting with potential lung disease using a C-reactive protein, white cell count and the erythrocyte sedimentation rate. 06:31 Sometimes we use genetic testing. That’s for cystic fibrosis, ciliary disorders, alpha-1-antitrypsin deficiency. And actually, increasingly that’s being used directly on tumour samples to get the tumour genetic status. And that’s relevant now before the more specific treatments we have for some of the more unusual tumour types. 06:50 And lastly, we just have to remember that lung disease is only one cause of breathlessness. 06:56 And therefore you may need to have other tests for people presenting with potential lung disease: a blood count to make sure they’re not anaemic; ECG, echocardiogram to assess the cardiac function.
About the Lecture
The lecture Diagnosis: Overview – Lung Disease by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Introduction to the Respiratory System.
Included Quiz Questions
Concerning the sensitivity and specificity of diagnostic tests, which of the following statements is accurate?
- Sensitivity is the proportion of people who have the disease and test positive for it.
- Specificity is the proportion of people who have the disease and test positive for it.
- Sensitivity is the proportion of people who don't have the disease and test negative for it.
- Specificity is the proportion of people who don't have the disease and test positive for it.
Which of the following is NOT a typical symptom of pneumonia?
- Rash
- Pleuritic pain
- Dyspnea
- Fever
- Cough
Regarding the efficacy of diagnostic tests, which of the following better defines sensitivity?
- Ability to detect true positives
- Ability to detect false positives
- Ability to detect false negatives
- Ability to detect true negatives
- Ability to decrease uncertainty
If a test has 90% sensitivity and 95% specificity, what percentage of patients could have gotten a false-negative result?
- 10%
- 5%
- 15%
- 20%
- 25%
All of the following tests are used to assess lung physiology, except...?
- ...CT scanning.
- ...lung function testing.
- ...blood gas measurements.
- ...sleep studies.
- ...PET and VQ radionucleotide scans.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |