Playlist
Show Playlist
Hide Playlist
Diagnosis of Tuberculosis
-
Slides 02 InfluenzaATuberculosis RespiratoryAdvanced.pdf
-
Download Lecture Overview
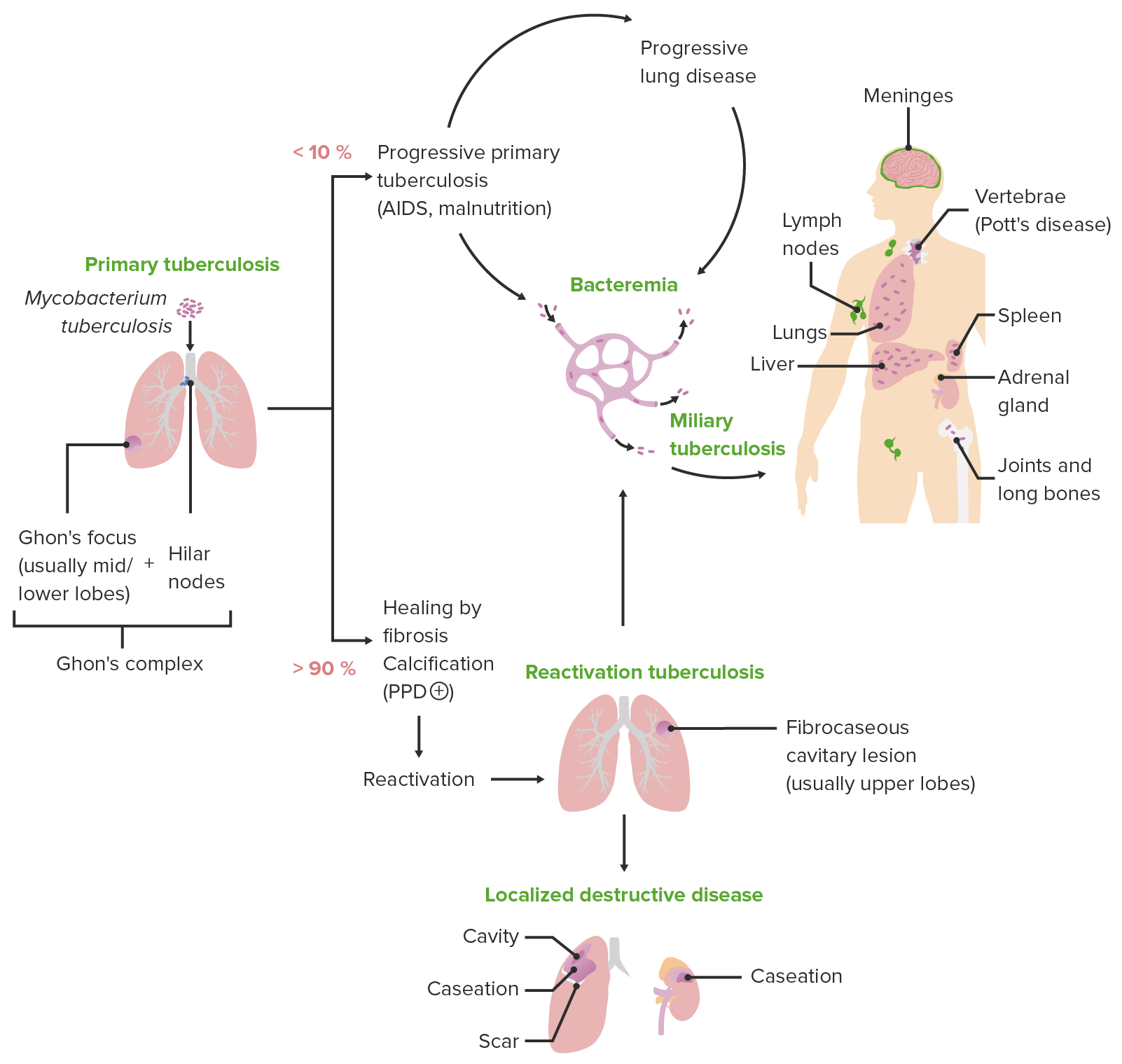
00:01 How do we confirm the diagnosis? Well frequently, the diagnosis is clinical only. If you are in a developing world where you don’t have access to the investigations that we have in the industrialized countries, then you may have to be reliant on clinical diagnosis. Confirm diagnosis requires seeing or culturing the bacteria in a sample from the patient. And for lung disease what we do is to present 3 morning sputums for culture and microscopy. For extra pulmonary disease we may be able to get a sample so for example genital urinary disease, the urine might be positive. Meningitis, the CSF might be positive but we often have to do biopsies of the affected tissue as well because that will give us a sample for culture and also for looking histologically for the characteristic granulomas that I have mentioned earlier. 00:56 So microscopy, what we are looking for is acid fast bacilli, there is a special stain used for mycobacteria, and if they are present they will be positive for that stain and show up on the microscopy. And that shows there is a mycobacteria present in that sample, and sort of 95 times out of 100 that mycobacteria will be tuberculosis, although occasionally it is one of those non-tuberculosis mycobacteria that I mentioned earlier in this talk. 01:24 Culture is very important because it confirms that mycobacterium present in microscopy is M.tuberculosis, and more importantly, it gives you the resistance profile. Whether that bacteria is a sedative M tuberculosis or resistant to some of the drugs that we might use to treat it. The big problem with culture is that it’s slow, it takes 3 to 4 weeks. So you're often left with a patient who has given a sample, no acid fast bacilli have been seen in it and you are waiting now for the culture to occur, and you need to make a decision whether the patient requires treatment for TB, because you're rarely sure that they might have TB. 02:03 For example in one of the examples I showed earlier, the Bengali man he would be treated before we got the culture results back even if he was AFB negative in sputum because the clinical presentation was so clearly going to be tuberculosis. But if it’s not clear, then you are just left waiting. Patients with pulmonary tuberculosis their sputum will be culture positive for the Microbacterium in 60 to 70% of cases at least. However, for extrapulmonary tuberculosis the chance of culture being positive is not so high for some diseases, nodal disease, lymphnode disease, pleural tuberculosis and TB Meningitis. 02:46 The yield from culture is much lower. Recently there is a polymerase chain reaction which has been developed, which is useful for identifying tuberculosis much more rapidly than culture does and that’s actually positive even in patients who are not AFB positive and that has improved our ability to rapidly recognize patients with tuberculosis. We also use biopsies to try and prove that tuberculosis is present. Now this is particularly important for extrapulmonary disease and what the biopsy will show is the presence of Ghon granulomas, which has very specific histological appearance that reflects the immunological response to the presence of Mycobacterium tuberculosis. And in fact with TB there are very specific granulomas which have a central area of necrosis and then that’s called caseating granulomas. 03:38 And we use biopsias of the pleura, abdominal disease, the lymphnodes to confirm the patient may have extrapulmonary tuberculosis. Now the main difference with diagnosis when you have histological show of granulomas is of sarcoid. Now in most clinical circumstances TB and sarcoid are not easily confused, the main exception being the presence of mediastinal lymphadenopathy. The difference between sarcoid and tuberculosis is that the granulomas in sarcoid tend to be not caseating and clearly, you won’t grow the bacteria M.tuberculosis from patients with sarcoidosis. We also use immunological testing, and what we use that for is to identify patients who have previously been exposed to or infected with tuberculosis, and this therefore identifies latent infection. And we have two different methods for testing for that, one is the Heaf test or Mantoux where we inject a mixture of tuberculosis antigens into the skin and in patients who've previously been exposed to tuberculosis that will stimulate their immunological reaction and a painful lump will form there. The other test is more recently developed blood test where essentially we do a very similar thing, you incubate the patient’s blood with a tuberculosis antigen and you see whether the white cells have a response to that, and those are called the Interferon Gamma Release Assays. Their main advantage is that they are not confounded by previous vaccination with BCG. So for example, I have a reasonably strong Mantoux reaction because I was vaccinated with BCG as a child and that means it's very difficult to use that skin test to identify patients who may have been exposed to tuberculosis if they've previously had BCG vaccination. However, the Interferon Gamma Release Assay will only be positive in patients with previous tuberculosis exposure and is not affected by the BCG.
About the Lecture
The lecture Diagnosis of Tuberculosis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Infections of the Respiratory Tract.
Included Quiz Questions
Which of the following is NOT usually used for the diagnosis of tuberculosis?
- Blood culture
- Sputum microscopy
- Sputum culture
- Excision biopsy of the extrapulmonary site
- Aspiration cytology
Which of the following is the most sensitive test to detect tuberculosis?
- Culture
- Acid-fast bacilli smear
- Mantoux test
- Nucleic acid amplification test
- Interferon-gamma release assay
Which of the following stains is commonly used to identify Mycobacterium tuberculosis?
- Ziehl-Neelsen
- Gram
- KOH
- Reticulin
- Silver
Which of the following tests can confirm someone has active pulmonary infection with Mycobacterium tuberculosis?
- Sputum culture and microscopy
- CT of the lungs
- Chest X-ray
- Interferon-gamma release assay
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |