Playlist
Show Playlist
Hide Playlist
Crohn Disease
-
Slides GIP Crohn Disease.pdf
-
Download Lecture Overview
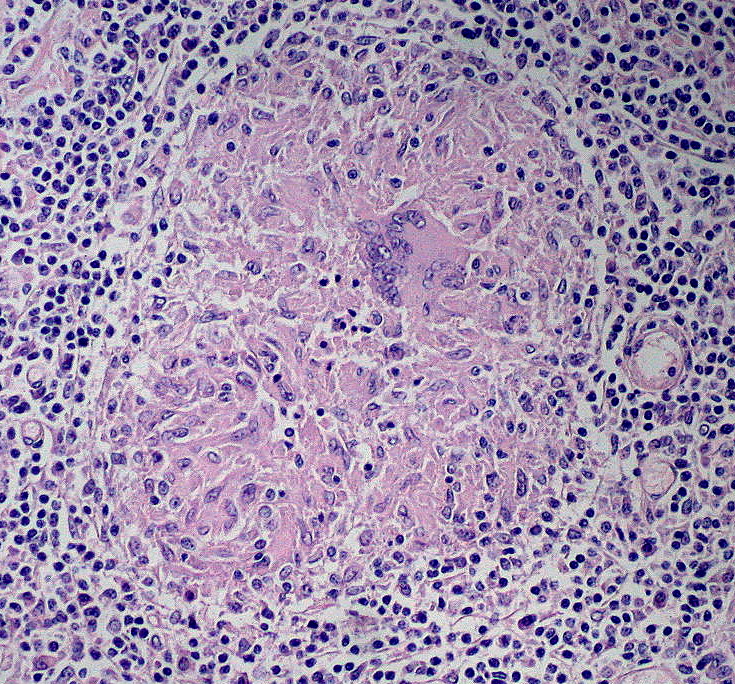
00:02 Welcome. In this talk, we're going to discuss one of the forms of inflammatory bowel disease, Crohn's Disease. 00:08 Crohn's Disease, and you'll see it abbreviated CD on the slides, is inflammatory bowel disease than can affect any portion of the GI tract. 00:18 It's also called regional enteritis but anything from mouth to anus can be affected by Crohn's Disease. 00:26 The inflammation in Crohn's Disease or regional enteritis is classically a granulomatous inflammation, suggesting that there are certain types of pro-inflammatory mediators driving a type 1, a Th1 helper phenotype. 00:41 There is transmural inflammation and importantly, there's the formation of fistulous tracts connecting bowel to bowel, bowel to bladder, bowel to skin. 00:51 And those distinguish this Crohn's Disease from Ulcerative Colitis. 00:57 The epidemiology. So, the incidence is not high. But if you have it, you know you have it. 01:06 About three to 20 per 100,000 adults per year. 01:09 There is a bimodal distribution with late teenage years and early adult years, and a smaller peak later on in life. 01:17 The frequency between men and women is comparable. 01:20 Risk factors include smoking, although, smoking is associated with a lot of other things and it's just a epidemiologic association. 01:29 We don't truly understand why. If there's a family history of inflammatory bowel disease, that does increase your risk. 01:36 And as we'll see, there's a very strong genetic component. 01:39 In fact, the twin concordance rate, identical twins, if one twin has it greater than 50% of the time, the other twin will have it as well. 01:49 And interestingly, 15% of patients who have Crohn's Disease, will have an affected first-degree relative, brother, sister, mother, father. 02:00 The genetics show an association epidemiologically with HLA-B27 and also with pleomorphism in the NOD2 genes that's involved in immune regulation. 02:13 Pathophysiology. It's really fairly straightforward. 02:19 Although, the reasons that any particular individual has dysregulation of immune response are not completely understood. 02:26 But once the immune response is dysregulated, we understand it pretty well. 02:31 We're looking at normal epithelium here shown in the small bowel because we have a Paneth cell that is present. 02:38 The normal epithelium is a tall columnar epithelium. It makes a - it has a villous layer and microvilli on the surface. 02:46 It makes mucus. There are tight junctions that keep the luminal contents within the lumen and the extra luminal contents like blood and connective tissue out of the lumen. 02:57 Within the extraluminal space within the laminar propria, there is a normal conversation going on between macrophages and dendritic cells that are sampling in many respects what is in the luminal contents. 03:13 So there will be bacteria there. 03:15 Dendritic cells and macrophages being antigen presenting cells are sampling that and they are in most cases turning on the formation of regulatory T-cells, not pro-inflammatory but T-cells that are going to say, "Oh, those contents - no, those bacteria in the GI tract, they're cool. 03:34 Leave them alone." And we will get expansion of the regulatory T-cell population. 03:38 So, that's how we have this commensal relationship with most of the bugs, the microbiota that live within our GI tract. 03:46 That's the normal situation. In patients who have Crohn's Disease, there will be a variety of mutations and the NOD2 mutation which is going to be involved in innate immune responses is a classic one. 04:02 But in all cases, what we have is a primary dysregulation of a variety of things at the level of the epithelium or at the level of the inflammatory response. So, you may have dysregulated tight junctions. 04:15 You may have dysregulated mucin production. You may have dysregulated paneth cells. 04:22 And in all those settings, we may have an ability for the microbiota to transverse the epithelium. 04:31 In association with that, we also have a defective regulation of tight junctions and we have changes potentially in the microbiota. 04:31 Those come across and are processed and presented. 04:31 Those come across and are processed and presented. 04:36 And in individuals who are going to be prone to having inflammatory bowel disease, we will regulate or upregulate, induce the production of pro-inflammatory T-cells. 04:47 Predominantly in Crohn's disease, Th1, T helper 1 variety. 04:52 That expansion then gets us many more of the Th1 helper T-cells, not regulatory T-cells but pro-inflammatory T-cells that will drive the inflammatory process. The clinical presentation. 05:05 The GI manifestations are related to malabsorption and inflammation. 05:12 So, there will be chronic, intermittent diarrhea. 05:14 It's usually non-bloody but it can be bloody depending on the degree of invasion and the degree of injury to the epithelium. 05:23 There's crampy abdominal pain because of the malabsorption. 05:26 What we're getting is nutrition, nutrients not being appropriately absorbed, and then, bacteria fermenting those. 05:33 But you can also have because of inflammation, the bowel spasming, smooth muscle contracting. 05:39 There may be, depending if you have disease that involves the upper GI tract, odynophagia, pain on swallowing or abnormal difficult swallowing, dysphagia. 05:49 There may be flatulence and bloating associated with fermentation of poorly absorbed nutrients. 05:55 There may be fecal incontinence because of spasming of the small bowel, particularly, within the rectum and anus. You may evacuate stool contents inappropriately. 06:06 And depending on the degree of involvement and where the involvement is in the GI Tract, you may have signs of malabsorption. 06:12 You will also, because again, this is a pro-inflammatory process, tend to have a low-grade fever. 06:19 You may have other signs related to the elaboration of pro-inflammatory mediators like TNF, Tumor Necrosis Factor and interleukin-1, you may lose your appetite. With malabsorption, you're going to have weight loss. 06:32 You may have anemia, again, because of malabsorption of important nutrients for normal red cell and red cell development. 06:40 In children who have this, they may have failure to thrive or growth retardation. 06:46 The extraintestinal manifestations are multiple. 06:50 And they may be due to a general pro-inflammatory environment within these patients, maybe secondary to the malabsorption or maybe due to local mucosal effects in other areas of the body. 07:05 So, aphthous ulcers, painless oral ulcers may be part of this. 07:09 You may get gallstones because you don't have normal bile acid reabsorption from the GI tract if that's where it's affected. 07:16 Kidney stones will happen because there's decreased fat absorption and it gives us increased excretion of calcium oxalate within the blood stream and the kidney. 07:27 And pyoderma gangrenous which is a painful papule and pustules in the skin. 07:32 Other extraintestinal manifestations, erythema nodosum, a pro-inflammatory erythematous nodule typically on skin, eye inflammation, you may have arthritis and ankylosing spondylitis and osteoporosis will also occur. 07:50 The later because you have malabsorption and not absorbing calcium appropriately. 07:55 Making the diagnosis in the primary setting. Part of this involves seeing how serious the malabsorption is. 08:03 So, we'll do a CBC. We'll be looking for elements of anemia and what kind of anemia, microcytic or macrocytic. 08:09 We may be looking for leukocytosis, we may be looking for thrombocytosis. 08:13 All those are pro-inflammatory markers. We'll look for electrolyte imbalances. 08:18 We will specifically assess for iron or vitamin B, B12 or folate deficiency. 08:24 An elevated erythrocyte sedimentation rate or elevated C-reactive protein are important kind of systemic pro-inflammatory markers and will be elevated in Crohn's Disease. 08:35 We want to exclude other causes. So, we're going to exclude infection. We're going to exclude Clostridioides difficile toxin. 08:43 We will look for the presence of blood. Blood can be present in inflammatory bowel disease or may not be present. 08:53 But if we have a lot of blood, that's going to suggest another cause perhaps. 08:57 CT is going to be in some respects, somewhat helpful if you see focal areas of bowel thickening or induration. 09:05 But ultimately, it's going to come down to colonoscopy and biopsy. And that's where the pathologist comes in. 09:12 This image is what we would see classically on endoscopy. 09:15 We have a lesion of focal ulceration and then, when we biopsy that zone, we see markedly increased inflammation with non-caseating granulomas. 09:26 Now, importantly, just as kind of a take home message, you won't always see the non-caseating granulomas in a Crohn's biopsy. 09:34 In fact, only about 50% of cases will have that. 09:38 However, the presence of a non-caseating granuloma is very highly supportive of that diagnosis and not for example, ulcerative colitis. 09:49 On imaging, so, we have opacified all of the bowel but with a barium ingestion. 09:59 That can demonstrate fistulous tracts. It can demonstrate focal areas of bowel wall thickening due to inflammation. 10:08 The management. So, we need to make sure that we cover out bases in terms of metabolic derangements. 10:17 If there is a vitamin B12 or a vitamin D insufficiency due to malabsorption, we need to make sure that we cover that. 10:26 We need to give anti-diarrheal patients so that the patient, the poor patient, isn't sitting all day on a toilet. 10:33 We may do targeted medical therapy. 10:35 So, in some cases, antibiotics are quite helpful by changing the bacterial milieu within the lumen. 10:44 Anti-inflammatory agents such as corticosteroids or immunomodulators such as azathioprine or mesalamine. 10:51 Or specifically, anti-cytokine therapies, anti-tumor necrosis factor therapies like infliximab or adalimumab. 10:59 And then, if we have fistulous tracts, that may require that there be surgical intervention. 11:07 So, we may have to take out portions of the intestine. 11:09 There is with chronic inflammation in any epithelium that's regenerating, a risk for cancer and we will have to constantly monitor in patients who have long-term reactive Crohn's Disease. 11:24 We'll have to monitor them for the development of adenocarcinoma. 11:27 And with that, we've reached the end of Crohn's Disease.
About the Lecture
The lecture Crohn Disease by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
At what age are patients often diagnosed with Crohn disease?
- Bimodal: 15–25 years old and 50–70 years old
- Bimodal: 25–35 years old and 50–70 years old
- Bimodal: 15–25 years old and 60–80 years old
- Bimodal: 5–15 years old and 50–70 years old
- Bimodal: 15–25 years old and 30–40 years old
Which of the following is an alteration in the intestinal epithelium as a result of Crohn disease?
- Defective regulation of tight junctions
- Decreased permeability
- Decreased antigen uptake
- T cell inactivation
- Squamous metaplasia
Which of the following is an extraintestinal manifestation of Crohn disease?
- Aphthous ulcers
- Pancreatitis
- Erythema
- Bladder hypomotility
- Benign prostatic hyperplasia
Which of the following is NOT an extraintestinal manifestation of Crohn disease?
- Pancreatitis
- Gallstones
- Kidney stones
- Pyoderma gangrenosum
- Erythema nodosum
Which histologic feature is highly supportive of Crohn disease and not ulcerative colitis, even if present in only 50% of cases?
- Noncaseating granulomas
- Cholesterol clefts
- Xanthoma cells
- Laminated whorls
- Numerous mast cells
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |