Playlist
Show Playlist
Hide Playlist
Colorectal Cancer Screening
-
Slides ColorectalCancerScreening PreventiveMedicine.pdf
-
Download Lecture Overview
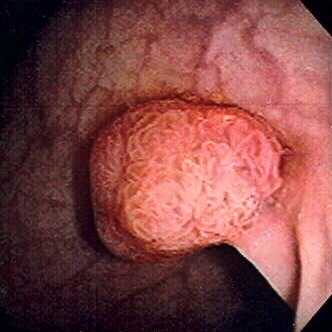
00:01 All right, so let’s talk about colorectal cancer screening and I personally think it’s a real shame that colorectal cancer screening doesn’t get the attention that it deserves in the United States. 00:10 I’ve been in practice now for 20 years, I mostly see older adults who should receive colorectal cancer screening and I can’t remember once where the first thing that a patient told me when they came in is, “I’m here to get colorectal cancer screening.” Not once, thousands and thousands of patients. 00:26 And that makes sense because if you look at who should be screened in the United States, less than half of those individuals who should be up-to-date on their colorectal cancer screening are up-to-date on their screening. 00:37 So we have a long way to go. 00:38 Let’s talk about some of the modalities that can be used and screening intervals that are recommended. 00:45 And so we’re going to do a case to illustrate this issue. 00:48 We’ve got a 51-year-old man, who is at average risk for colorectal cancer. 00:54 Based on recommendations from the United States Preventive Services Task Force, what screening modality is acceptable for him? Is it a FIT test, a Fecal Immunochemical Test alone, or FIT plus sigmoidoscopy, or colonoscopy, or D, all of the above? There are options here and there are options based on where your patient is coming from, what they want out of screening, and therefore, you should be ready to discuss all these options with your patients. 01:25 But what’s incontrovertible is that colorectal cancer is the third most common cancer in the US among both women and men. 01:34 There is a significant number of colorectal cancer deaths in the United States every year, but that number is getting better over time. 01:43 And always think about modifiable risk factors for colorectal cancer. 01:48 So it’s not just a family history, smoking increases the risk, obesity increases the risk. 01:53 And those, you can’t do much about your family history, you can certainly do something about those latter two issues. 01:59 So when to start and stop colorectal cancer screening? The American College of Gastroenterology recommends screening at age 40 for higher risk individuals, that includes Black adults, and certainly patients with higher risk, with the familial polyposis syndrome, maybe screened even earlier than that. 02:19 For most adults, the vast majority, other adults, the screening should begin at 45 years of age. 02:26 When to stop? There’s insufficient evidence to recommend screening beyond 74 years. 02:31 Again, that might be something where you want to use shared decision-making. 02:35 Look at your patient in terms of their quality of their life, their general life expectancy, and choose what you want to do. 02:43 How to screen? So as I mentioned, USPSTF recommends FIT annually. 02:48 FIT annually, in and of itself, can reduce the risk of death due to colorectal cancer. 02:55 Flexible sigmoidoscopy has also been widely studied in its effects on colorectal cancer detection as well as mortality and it is effective as well, and it’s usually combined with a FIT test every several years or even annually. 03:14 And then the other option is the colonoscopy, which is the more complete test but the more expensive test every 10 years. 03:21 So in a way it’s maybe confusing because there are options that might be acceptable. 03:27 In another way this allows you a menu that you can give to your patients and say, “Okay, pick one of these,” because doing something is at least better than nothing, that’s for sure. 03:39 So the American Gastroenterological Society prefers colonoscopy, they recommend the alternative to colonoscopy as an annual FIT, and there’s another option, which is CT colonography and that can be acceptable every five years as an alternative. 03:57 So let’s look at a patient who went through the colonoscopy and then has some results. 04:03 So the patient we mentioned previously, he goes through a colonoscopy, he’s diagnosed with two tubular adenomas, they’re both greater than 1 centimeter in the descending colon Now, when should you schedule his next colonoscopy? And this kind of a challenging question because there are a lot of different options but we’re going to go through those options in a second. 04:23 The answer is three years, and that has to do more with the size of his adenomas versus the type of adenomas. 04:30 Tubular adenomas, the most common adenoma, they comprise about 80% of adenomas and they really have the lowest malignant potential, but at the same time, his adenomas were greater than a centimeter in size. 04:45 Size does matter in terms of the risk of future cancer, and therefore, he got an advanced -- this patient is getting an advanced screening in only three years. 04:55 So as I mentioned in normal exams, and we need to do our job, by the way, in sticking to these screening intervals and these recommendations, so do pay attention. 05:04 Normal screening interval is 10 years. 05:07 Hyperplastic polyps less than 10 millimeters don’t really have any malignant potential, therefore, 10 years. 05:14 One to two tubular adenomas that are smaller, 5 to 10 years. 05:19 A sessile serrated polyp less than 10 millimeters, serrated polyps associated with a higher malignant potential that’s still small, no evidence of dysplasia, five years. 05:30 A larger number of tubular adenomas up to 3 or 10 is a three-year screening interval. 05:39 And when the tubular adenoma or serrated polyp is larger, that also mandates automatically a three-year screening interval. 05:47 Villous adenoma, these have a higher malignant potential, or any finding of high-grade dysplasia, three years. 05:54 That serrated polyp with dysplasia, three years. 06:00 And larger serrated adenomas though that aren’t sessile can be screened every 5 to 10 years. 06:07 Many, many adenomas, that’s kind of a judgment call but it’s going to be under three years. 06:13 If there is an attempt to do a piecemeal resection of a large adenoma, the screening interval should be less -- is generally less than one year, but again, that’s going to be up to the operator again. 06:24 And status post a curative resection for a colorectal cancer, screening at one year, and then three, and then five years after detection. 06:32 And it’s worth noting that the risk of developing polyps in a lifetime is about 70%. 06:38 So it’s normal for somebody, most patients actually will fall somewhere on this list, but it’s usually going to be on this list with a more benign type of polyp or more benign adenoma. 06:50 All right, moving on. 06:53 That’s really what I wanted to impart today. 06:54 Just understand that we are underusing colorectal cancer screening because even -- something that’s fairly simple and straightforward such as FIT testing on an annual basis can be effective. 07:08 And for those patients who obviously have a positive screening on FIT, then you really have to advocate for them strongly to get a colonoscopy because their risk for some type of colorectal cancer or advanced polyp are much higher. 07:22 But recommend something and really engage your patients as to what their preferences might be, and then we will have success in finding more colorectal cancers preventing more deaths. 07:33 Thanks.
About the Lecture
The lecture Colorectal Cancer Screening by Charles Vega, MD is from the course Preventive Medicine. It contains the following chapters:
- Colorectal Cancer Screening
- Screening – When to Start and Stop
- Next Colonoscopy
- Intervals for Following Colonoscopy Results
Included Quiz Questions
Which of the following is the third leading cause of cancer-related deaths in adults?
- Colorectal cancer
- Prostate cancer
- Breast cancer
- Lung cancer
- Skin cancer
What is the preferred age of colorectal cancer screening in African Americans according to the American College of Gastroenterology?
- 45 years
- 50 years
- 55 years
- 60 years
- 65 years
What is the recommended frequency of fecal immunochemical testing in the United States for colorectal cancer screening?
- Annually
- Every 5 years
- Every 3 years
- Every 10 years
- Every 6 months
All except which of the following are screening methods for colorectal cancer?
- Rigid sigmoidoscopy
- Colonoscopy
- Fecal immunochemical testing
- Flexible sigmoidoscopy
- Computed tomography colonography
What is the recommended screening interval of colonoscopy in patients with hyperplastic polyps < 10 mm?
- 10 years
- 10-15 years
- 5-10 years
- Within 1 year
- 1-3 years
All except which of the following colonoscopic findings require colonoscopy surveillance in 3 years?
- Hyperplastic polyps less than 10 mm
- Villous adenoma
- Sessile serrated adenoma ≥10 mm
- Sessile serrated adenoma with high-grade dysplasia
- Tubular adenoma ≥10 mm
Which of the following types of polyps is appropriately matched to the interval for colonoscopy surveillance?
- Villous histology - 3 years
- Tubular adenoma ≥10 mm - 5 years
- Sessile serrated adenoma with high-grade dysplasia - 10 years
- High-grade dysplasia - 5 years
- Two hyperplastic polyps <10 mm - 5 years
An 80-year-old patient has undergone regular colonoscopy screening for colorectal cancer from the age of 50 years. All screening has been normal. He wants to know how long he has to continue screening. What is the best reply?
- There is no clear evidence to continue screening after the age of 74 years. You can choose to stop or continue screening.
- You can continue to have screening for as long as you wish.
- You can stop the screening for colon cancer.
- It is best to continue screening for colon cancer.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It is a very important matter. Profesor teached very clearly and simple. Focused in the patient and statistics. Congratulations.