Playlist
Show Playlist
Hide Playlist
Colonic Polyps: Diagnosis and Management
-
Slides GIP Colonic Polyps.pdf
-
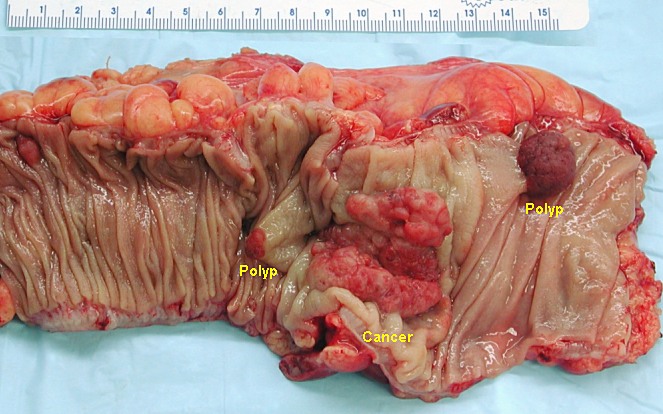
Download Lecture Overview
00:01 When we talk about the pathophysiology for the development of colonic polyps, we're really talking about the same pathways that are operative when we talk about the development of colorectal cancer and you have seen or I will refer you to other areas in the collection of Lecturio lectures that talks specifically about colorectal cancer. 00:21 Okay. The epithelium at baseline has a normal regulated turnover. The cells are born. 00:28 They grow and they die over the course of three to seven days. 00:31 So, you'll get the entire sequence of events that completely replaces the colonic epithelium every week or so. 00:38 If you have a germline mutation in one of the genes such as APC that regulates normal colonic epithelium proliferation, that gets you started down a path that the epithelium is completely normal. 00:54 You may then get a second hit in a similar gene or the same gene. 01:00 So, that means that you have a germline mutation and that gene is non-functional. 01:04 And then, one of the cells happens to get a second hit in the other normal gene. 01:10 And now, you have loss of heterozygosity and that can drive the mucosa to proliferate abnormally. 01:18 Now, we have mucosa at risk. 01:20 With further additional mutations and a proliferating epithelium, you may still stochastically acquire a mutation say, in KRAS or other genes that are proto-oncogenes that drive cellular proliferation from another pathway. 01:38 And then, we are going to develop adenomas. So, these cells have lost some of their normal behavior. 01:46 They are not yet cancers but they are proliferating. They are proliferating in a setting where there may be additional opportunities for mutations and they acquire additional changes. 01:59 So, they may have mutations in p53, the normal gene that's going to identify abnormal chromosome or DNA structure and repair it. 02:11 They may have changes in methylation. They may have changes in cyclooxygenase. 02:16 All these things can potentially drive the acquisition of mutations that will eventually allow these to become malignant. 02:24 The clinical presentation for colonic polyps. How do these colonic polyps present? Well, they may be completely asymptomatic. 02:34 In fact, the vast majority of them are only discovered when you have screening colonoscopy. 02:39 But they may present in other ways. So, they are epithelial proliferations overlying blood vessels and if you erode the epithelium, you may get blood. 02:49 Or you may have a production of mucus because of irritation or because the epithelium is making more mucus and you may see that in the stool. If the polyp is sufficiently large, it may actually mechanically obstruct the bowel lumen. So, the patient may present with constipation. 03:06 On the other hand, you may have local irritation that drives increased bowel motility and patients may have diarrhea. 03:16 And then, with larger polyps beyond just constipation, you may have intussusception. 03:21 You may have the polyp drag as the peristaltic wave goes by, pull the bowel proximally to distally and you have telescoping or intussusception. How do we make the diagnosis? have no manifestations detected by either you or your patient. 03:31 So, let's talk about diagnosis which can be a little bit of a challenge since most of these colonic polyps really don't have much in the way of manifestations. 03:40 So, it's largely by screening colonoscopy or other forms of colon cancer evaluation that we're going to detect polyps early. 03:50 For people who have average risk which is to say they don't have a family history of polyps or of colorectal cancer, colon screening will begin roughly at the age of 45. 04:02 If you have a first degree family member with colorectal cancer at an age less than 60 years where there's a family history of colonic polyps, then, you will get screened beginning a little bit earlier. 04:15 For patients who are at higher risk, so, we know inflammatory bowel disease is a risk for polyps and colorectal cancer and the polyposis syndromes that we had talked about, Lynch and FAP, all of those mean those individuals need to be screened very early. 04:35 And at some cases like FAP where there's 100% risk of developing colon cancer over a lifetime, you may elect to not screen and just remove the colon earlier rather than later. 04:48 So, for patients where you suspect a hereditary polyposis or colorectal cancer syndromes, you may do formal molecular testing, particularly, if an individual has been identified in the family, you will test all first degree relatives. For regular screening, you'd want to look for occult blood and there are a number of tests, including some that you can get through the mail and over the counter that looks specifically for common DNA mutations in the stool. 05:16 And then, finally, the gold standard by which we're going to make the diagnosis and we're going to do the appropriate polyp removal for evaluation and/or prevention of cancer is going to be sigmoidoscopy if you're just looking in the more distal sigmoid or colonoscopy. 05:32 And in fact, I would say, for the vast majority of your patients, you're not going to stop at the sigmoid. 05:37 You're going to want to look all the way around over to the cecum. 05:42 So, with colonoscopy screening, we're going to be able to establish a relative risk of the development of colon cancer. 05:49 So, depending on what we find, we can tell patients, "You have this risk. You have that risk." If there are no adenomas, there is still a lifetime risk of about 3% of developing colorectal cancer but in most cases, that's a good sign. If on colonoscopy, we found one to two adenomas and all of them are less than a centimeter, that's a lifetime risk of colon cancer of about 5%. 06:14 If on the other hand, we find high risk adenomas, a serrated type adenoma or if we can't find villous adenomas, that increases the risk of colon cancers. 06:24 The lifetime risk goes up somewhere between 15 and 20%. 06:28 This is an example of just what you can see when you become your - a world famous gastroenterologist and put the colonoscope up and take a look. So, on the left is a polyp on a stalk, so, called pedunculated polyp. This overall size here, it's hard to estimate, but it's about 1.5 centimeters. So, it's not too - the four centimeter category where we would have a high index of suspicion for malignancy. 06:54 But it's something if we don't take it out overtime will acquire additional mutations and become malignant. 07:01 On the right-hand side is showing multiple polyps in a colon and even though these are small, this raises the specter of a familial polyposis syndrome, so, Lynch syndrome or familial adenomatous polyposis. 07:15 Hyperplastic polyps have just benign epithelial proliferations. 07:20 So, it's just a little outpouching of mucosa and the histology is totally benign and I'm not expecting you as a medical student to say, "Oh, yeah. That's benign. 07:30 I would know of that in a - " No, you don't have to. That's why you send it to me. 07:34 But that's an example of what you can see and note, when we do the biopsy, we're not getting a full thickness biopsy. 07:40 In fact, you don't want to do that because that would mean you perforated the bowel. 07:44 This is just an epithelial biopsy. This is a histology of a juvenile polyp. 07:49 So, this is a benign hamartomatous polyp and it's classically associated with increased mesenchymal elements. 07:56 That's why we have all that spaced out stuff and they're cystically dilated glands. 08:00 So, this is a completely benign hamartomatous process. 08:07 Now, we're going to get into the category however of things that are not so benign. 08:12 So, this is an adenomatous polyp. This is probably a tubulovillous. It's got a little bit of both. 08:18 It's kind of tubular architecture but it's also a little bit kind of fibular or villous. 08:23 On the left-hand side, we're looking at a sessile polyp that's kind of stuck down. 08:29 It looks like a slug there in the colon and then, a tubulovillous polyp on the right cutting cross-section which has big frond-like projections. 08:38 Again, making the distinction between tubulovillous, tubularvillous, etc. is a microscopic finding for the most part. 08:49 And an adenomatous polyp has a greater density of cells. They tend to be more hyperchromatic. 08:55 The nuclei tend to come off the basic membrane. 08:58 The glands may be more dysmorphic and the cells may have some degree of atypia. 09:03 This would be a relatively small adenomatous polyp. 09:06 There's no malignancy in here but if we don't take it out, we're at risk for this eventually progressing to malignancy. 09:14 And now, management. And management really is all about what you find on your first colonoscopy and then, time to the next one. 09:23 So, when we do colonoscopy, we do assume that it's a complete exam all the way to the cecum. 09:29 You can have polyps anywhere in the colon and just stopping in the sigmoid is not going to be sufficient. 09:35 You want to make sure that you have an adequate prep or preparation so that you have cleaned out the colon sufficiently to be able to see all of the real estate. 09:44 And then, we want to make sure the person who's actually doing this is skilled so that they can recognize a polyp when they see one. 09:53 So, a normal colonoscopy is associated with a 0.5% risk of colorectal cancer in the succeeding 10 years. 10:03 There is still a lifetime risk of about 3% but it's a very low risk. 10:07 So, if you have a normal colonoscopy, no adenomatous polyps, even if you have small hyperplastic polyps, you are good to go for about a decade and you'll come back in 10 years and we'll do it again. 10:20 If you have low risk adenomas, so, you have one to two of them. They're less than a centimeter. 10:26 The dysplastic, the changes that make them worrisome in terms of low-grade, high-grade, etc. 10:32 dysplasia, they're all low-grade, you repeat in 7 to 10 years. 10:36 So, almost as good. If they are the sessile serrated type and they're a certain number and they're less than a centimeter, you can repeat that in 5 to 10 years, depending on your degree of comfort. And if there are other findings, so, if there are three, more than three adenomatous polyps even though they're small. 10:56 If there is large hyperplastic polyps, in that case, you would probably repeat in 3 to 5 years and if there is advanced neoplasia or high-risk adenoma, more adenomas, 5 to 10 or sessile polyps, or morphology with greater than a centimeter in size and the histology has a villous component and it's high-grade dysplasia, you're going to want to get that patient back in 3 years. 11:23 And if there are more than 10 adenomas, you want them back in a year. 11:29 You do not want to let them go and at that time, you've plucked out all the adenomas that you saw. 11:35 You didn't leave any behind but they're at risk of developing malignancy if you let them go longer. 11:42 What is being shown on the slide here is a colonic resection for a large polyp. 11:49 So, you may go in on your primary, your subsequent evaluations on colonoscopy, see something that you just can't pluck out. 11:57 That requires then calling your favorite neighborhood surgeon and they will come in and usually do an open procedure to take out the polyp. 12:08 If you see also lymphovascular invasion, that's another indication on histology that you need to have a larger resection to make sure that there is no nodal metastasis. 12:19 With that, we've covered benign and malignant polyps and what to do about them.
About the Lecture
The lecture Colonic Polyps: Diagnosis and Management by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is the most common presentation of a colonic polyp?
- Asymptomatic
- Hematuria
- Hematochezia
- Mucus in stool
- Constipation
At what age should screening colonoscopies begin for average-risk patients?
- 45 years old
- 35 years old
- 60 years old
- 55 years old
- 30 years old
What is the lifetime risk of colon cancer in patients with one adenoma?
- 5%
- 10%
- 15%
- 20%
- 25%
What is the appropriate proximal extent of a colonoscopy?
- Cecum
- Sigmoid
- Ascending colon
- Descending colon
- Rectum
What is an appropriate follow-up plan for a patient with low-risk adenomas?
- Repeat examination in 7 years
- Repeat examination in 3 years
- Repeat examination in 5 years
- Repeat examination in 1 year
- Repeat examination in 15 years
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |