Playlist
Show Playlist
Hide Playlist
Cold Autoimmune Hemolytic Anemia (CAIHA): Etiology, Pathogenesis and Clinical Pathology
-
Slides Autoimmune Hemolytic Anemia.pdf
-
Download Lecture Overview
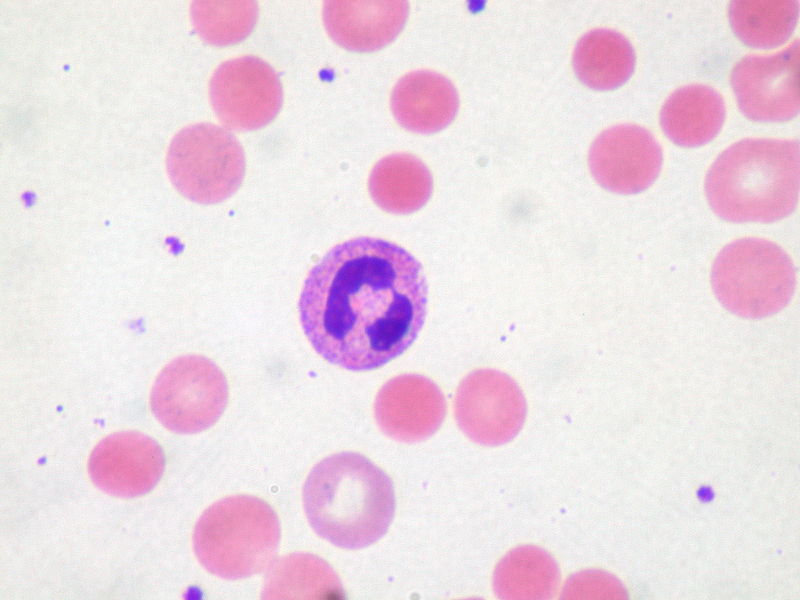
00:01 Let’s go into cold now. 00:01 What's cold? Well, first and foremost, take a look at an association, the big one here will be mycoplasma pneumonia. 00:09 Before we move on, you have to tell me who this patient is, right? So this is a patient that has low grade fever, walking. 00:17 "Everything is great, doc." I'm having a wonderful day today. 00:20 Sure. 00:22 No bed rest at all. 00:23 I’m good. 00:24 You do a chest x-ray. 00:25 Oh wow, that looks rather dangerous. 00:27 It makes me kind of worried. 00:29 Why? Well, it’s because this is a chest x-ray, in which you got scared because you saw the interstitium showing you what kind of pattern on chest x-ray with mycoplasma? A reticular pattern, wasn’t it? A reticular nodular pattern. 00:45 And so therefore, the chest x-ray might look worse than the actual condition. 00:50 So your patient was walking around. 00:51 Low-grade fever. 00:54 What is this? Atypical pneumonia. 00:56 That’s your patient. 00:58 And if your patient with mycoplasma pneumonia is presenting with, well, anemia and this is what it would be. 01:05 Cold autoimmune hemolytic anemia. 01:07 So what is cold? Well, as I told you, if you want to use cold in Michigan, by all means, please do so. 01:13 But here, you'll find IgM antibodies. 01:17 Next, what about these autoantibodies? Well, these will then bind to in cold extremities. 01:23 That’s important. 01:25 Antibody bind causes complement fixation, stop here. 01:28 Why? Complement fixation is a big deal. 01:34 Really? "I was just going to read through this, Dr. Raj." Yeah I know, that’s why I’m here. 01:38 So complement fixation means that -- You tell me. 01:41 There are three major pathways for complement, right? One is the classic, one is the alternative, the other one is lectin. 01:50 Well, let’s go ahead and talk about the classical. 01:52 What is a classical complement pathway? Why do we call it classic? Because it’s the antigen-antibody, antigen-antibody, antigen-antibody complex that will stimulate the classical pathway. 02:07 Why do I keep repeating antibody? Guess what that antibody is that starts off the classic complement pathway. 02:14 Think. 02:15 Oh, it’s the IgM. 02:16 What does an IgM look like? Yup. 02:17 It’s fat. 02:19 What do you mean? It’s a pentamer. 02:22 It has 5 arms. 02:22 It’s a really fat immunoglobulin. 02:26 In other words, it’s huge, huge. 02:30 So the characteristics of a very big immunoglobulin along with that, it’s bound to an antigen. 02:36 No doubt you’re going to kick off the classic complement pathway. 02:40 Keep that in mind. 02:41 That becomes a really important point for us. 02:44 Why? Well then here, here what you’re looking at is if you start off the classic complement pathway, you’re going to rip through your complements. 02:52 Here they come. 02:54 C1, your C3 convertase and you formed lots of C3b, C3b, C3b excessively. 03:04 In your medical education, you may or may not have been taught properly pay attention here. 03:10 You used to be taught that with IgM, that it would then be an intravascular hemolysis because of a complement fixation. 03:16 Not the case anymore. 03:18 So at current day understanding is the fact you’re going to produce. 03:23 And this is true. 03:23 Tons of C3b. 03:26 That C3b is exactly like whom? IgG. 03:32 What was IgG? An opsonin, the chocolate around the RBC. 03:37 And whenever that you bathe your RBC in chocolate or in this case an opsonin, where is the RBC being destroyed? Extravascular hemolysis. 03:50 Is that clear? So cold autoimmune hemolytic anemia is also going to be part of your extravascular hemolysis because of rapid activation of your classic complement pathway leading into C3b production, opsonization, extravascular hemolysis. 04:08 That is a big deal. 04:08 Let’s move on. 04:11 Let’s go ahead and take a look at how to diagnose your cold autoimmune hemolytic anemia. 04:14 Keep in mind, once again, that we are dealing with the IgM antibody. 04:21 Here, once again, it’s the fact that we’re trying to look for RBCs that are coated with the immunoglobulin. 04:26 So generally speaking, when you’re looking for a complex, you tell me what kind of Coombs test you would want to conduct. 04:33 Good. 04:34 A direct Coombs test. 04:36 Here, since it is cold, the diagnosis is made by identifying cold reacting antibodies by direct Coombs test. 04:42 The cold autoantibody are fairly common and transient. 04:46 Think about the condition that we talked about earlier. 04:48 We have M – IgM, M – atypical pneumonia, the common cause of atypical pneumonia being Mycoplasma pneumoniae. 04:58 So here, as far as clinical significance is severity well, warm is a lot worse; SLE, CLL, drugs. 05:09 With cold, it will be IgM, mycoplasma pneumonia and uncommon for them to cause serious clinical consequences.
About the Lecture
The lecture Cold Autoimmune Hemolytic Anemia (CAIHA): Etiology, Pathogenesis and Clinical Pathology by Carlo Raj, MD is from the course Hemolytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following antibodies leads to MOST cases of cold antibody hemolytic anemia?
- IgM
- IgE
- IgD
- IgG
- IgA
Which of the following antibodies can trigger the classical complement pathway?
- IgM
- IgA
- IgE
- IgD
- IgA and IgM
Which one of the following statements regarding atypical pneumonia is false?
- The chest X-ray will show lobar consolidation.
- The chest X-ray will show a reticulonodular pattern.
- The patient will present with a low-grade fever.
- The patient may present with anemia.
- The chest X-ray will appear to be worse than the patient’s clinical presentation.
Which of the following pathogens is the most common cause of atypical pneumonia?
- Mycoplasma pneumoniae
- Streptococcus pneumoniae
- Legionella pneumoniae
- Klebsiella pneumoniae
- Chlamydophila pneumoniae
Which one of the following statements regarding cold autoimmune hemolytic anemia is true?
- In cold autoimmune hemolytic anemia, the complement cascade is activated when RBCs travel to warm extremities.
- In cold autoimmune hemolytic anemia, the antibody agglutination occurs when RBCs travel to warm extremities.
- In cold autoimmune hemolytic anemia, the antibody that causes agglutination is IgM tetramer.
- In cold autoimmune hemolytic anemia, RBCs typically undergo intravascular hemolysis.
- In cold autoimmune hemolytic anemia, the alternate complement pathway is activated.
Customer reviews
1,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
The gibberish that falls out this retards mouth. WIsconsin, what, what?