Playlist
Show Playlist
Hide Playlist
Coagulation Screening and Platelet Disorders
-
Slides Measuring Clotting Parameters.pdf
-
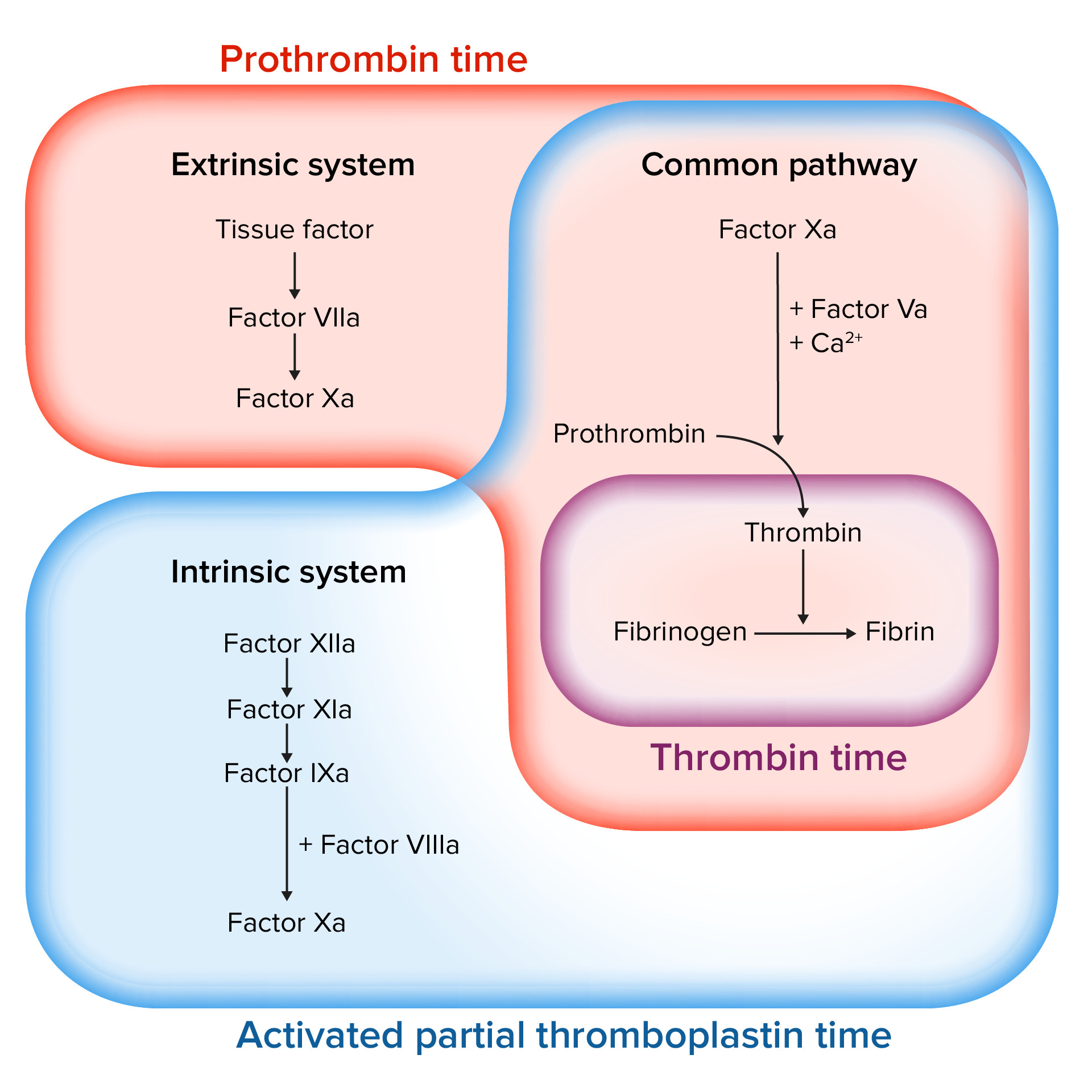
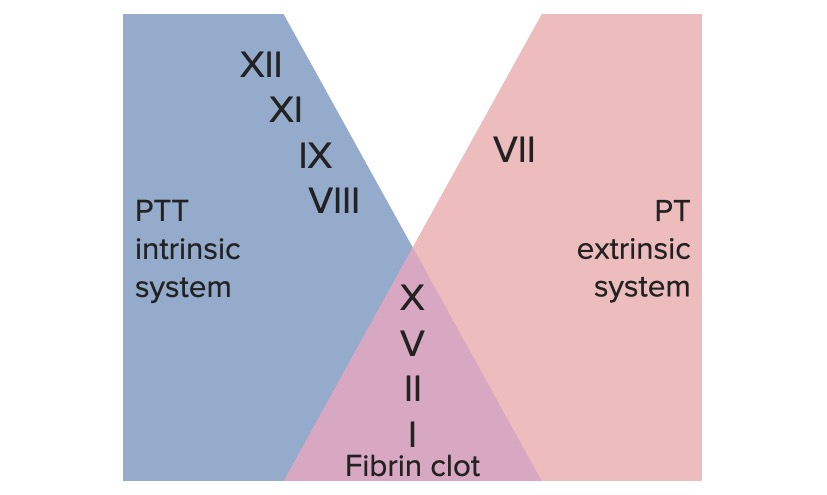
Download Lecture Overview
00:00 Okay, now that we've been through the adventure of talking about normal hemostasis and how we regulate hemostasis, let's talk about how we measure hemostasis because we're going to need to know what's normal, what's abnormal, and whether our therapeutic interventions are getting us to the right point. So, how do we measure this? Here's where we are on our total roadmap. You can see we're about halfway done, so we're getting in to the homestretch. Basic coagulation screening, we first have to look at platelet number and it's not just the number in a complete blood count that's with CBC is, but the quality of the platelets and their normal or abnormal function. So we have to do platelet function testing. 00:51 So, we also want to look at the coagulation cascade as part of our basic assessment. We want to look at 2 times, the prothrombin time and the partial thromboplastin time and the PT and PTT in a moment will become very clear, but we have 2 chemical laboratory measurements. And finally, the D-dimer. Remember as we talked about breaking down a fibrin platelet thrombus through the activity of plasmin and breaking off little fibrin degradation products? We are actually forming something called a D-dimer that we can measure to assess whether or not there is ongoing clotting or fibrinolysis and really important for things like diagnosing potential pulmonary embolization. Okay, so those are the kind of basic screening tests. Let's get down a little bit more into some details. Platelet disorders. So we want to get a connotation on the number of platelets, and in general we want to be above roughly 100,000 to 150,000 per microliter. So, the thrombocytopenia, a decreased platelet count, has many many causes. Everything from marrow failure to consumptive coagulopathy where we're clotting too much everywhere. We could also have too many platelets, thrombocytosis. This can be reactive so it can be due to normal processes. If we have an inflammatory response, the body responds by saying "We're under attack, we need to make more of everything that's going to protect us including more platelets." So a response to infection, injury, illness, or stress will actually cause the liver to make more thrombocyte-increasing factors and thrombopoietin in particular and that will cause us to have many more platelets. You can also have malignant diseases that are also causing increased numbers of platelets and so these are classified as essential thrombocythemia. It will be lead, obviously when you have too many platelets in this setting you will become hypercoagulable. You have just too many platelets and the potential for for them to be nonspecifically activated is something that you really have to very much be aware of. One of the major mutations that drives thrombocythemia is a Janus kinase, that's JAK2, and you'll hear about this in your patients. It's a tyrosine kinase that causes a constitutive activation of the megakaryocytes in the bone marrow and we constantly crank out too many platelets. So a JAK2, Janus kinase-tyrosine kinase mutation is detected in 30% of patients with essential thrombocythemia. It's not enough just to count how many platelets, too many or too few. We also have to say "Are they working appropriately?" So, even though you have an adequate platelet count, if they don't clot appropriately we have various ways of measuring that, then you will have bleeding problems. And this can be congenital, you can be missing some of the receptors that normally are responsible for platelet aggregation or platelet activation. Or you can have acquired defects. So NSAIDs, you're all familiar with non-steroidal anti-inflammatory drugs such as aspirin, such as naprosyn, such as ibuprofen and those will cause platelets to not function. In fact, we use those intentionally for patients who might be a little hypercoagulable or otherwise have risk for having a coagulation event. We say "Take an aspirin a day" because that will inhibit platelet aggregation. But, if you have taken an aspirin a day and then you suddenly need surgery, we may have to delay a bit until your platelets become functional. Okay.
About the Lecture
The lecture Coagulation Screening and Platelet Disorders by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
What test helps to diagnose a disease that causes uncontrollable clotting?
- D-dimer
- CBC
- Prothrombin time (PT)
- Partial thromboplastin time (PTT)
- Platelet function
Platelet dysfunction and decreased platelet aggregation may be caused by which of the following?
- NSAIDs
- Infection
- Injury
- Stress
- Malignancy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |