Playlist
Show Playlist
Hide Playlist
Clinically Isolated Syndrome: Clinical Manifestations and Classification
-
Slides Multiple Sclerosis Inflammatory Disorders of the CNS.pdf
-
Download Lecture Overview
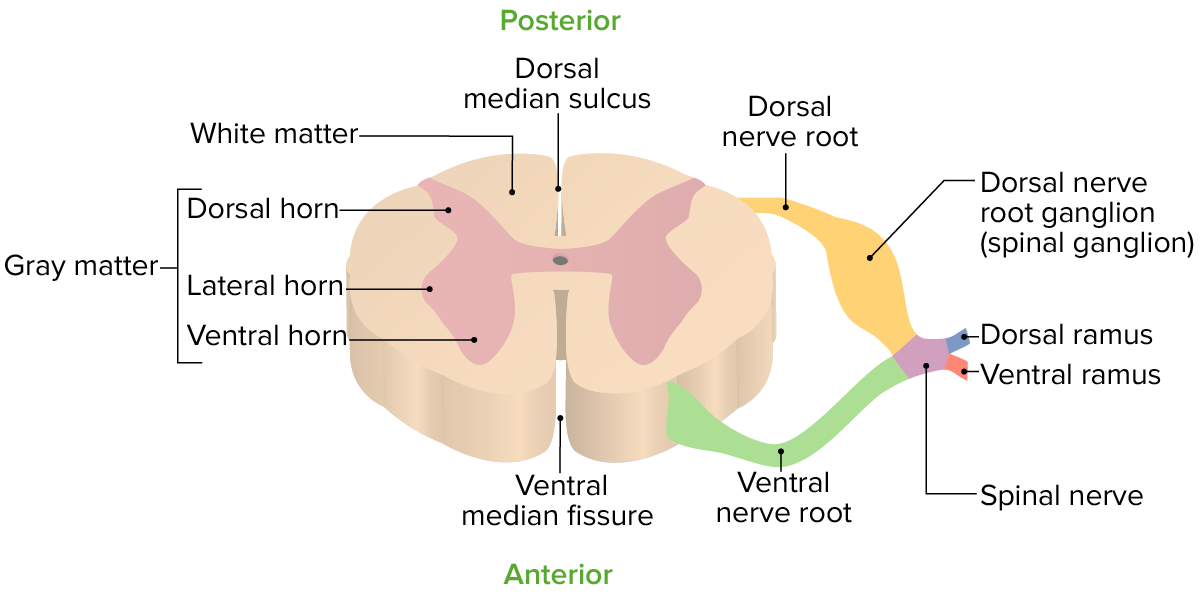
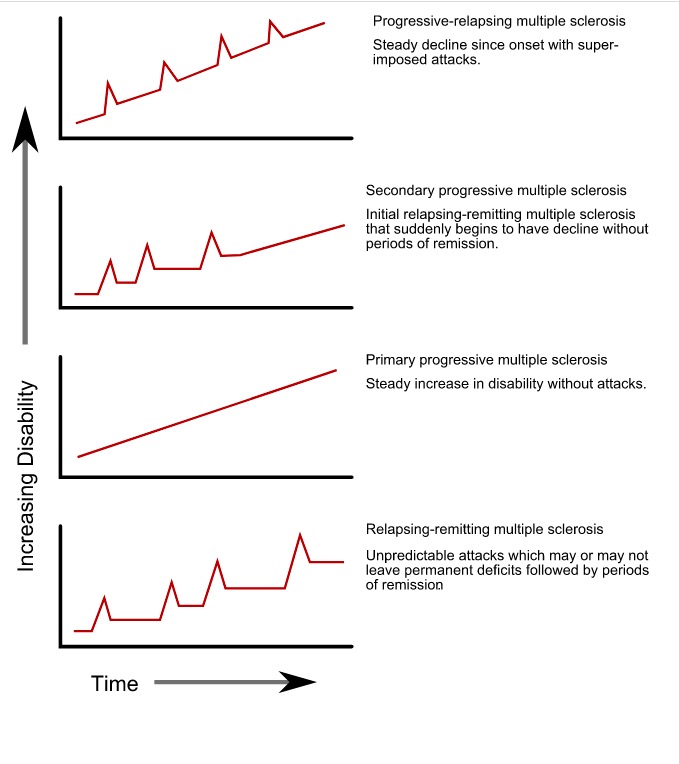
00:01 So let's start with a definition. 00:03 What is clinically isolated syndrome? This term is used to identify a clinical event that has characteristics of a demyelinating episode, such as a transverse myelitis or an optic neuritis. 00:14 But MS cannot be formally diagnosed. It's not recurrent. 00:17 There's not evidence of other events. 00:19 So the definition of clinically isolated syndrome is the first clinical and neurologic event suggestive of a demyelinating attack or MS, lasting greater than 24 hours. 00:31 It's caused by inflammation or demyelination in one area of the nervous system (monofocal) or can be seen in multifocal or multiple areas of the nervous system. 00:42 And types of attacks include optic neuritis, spinal cord syndromes, and brainstem syndromes. 00:48 Importantly, there's not evidence of prior attacks in these patients. 00:53 What are the types of clinically isolated syndromes? Well, inflammation can affect anywhere in the nervous system including the optic nerves, spinal cord, brainstem, and multiple areas in the brain. 01:04 And we can see the breakdown of typical presentations of clinically isolated syndrome. 01:08 Optic neuritis occurs in somewhere around 20-21% of patients. 01:13 Spinal cord syndromes are common and are termed clinically isolated transverse myelitis where a single segment of the spinal cord is affected such as in our patient. 01:24 The brainstem can be affected in a minority of cases and some patients will present with multifocal attacks in 23%. 01:33 Let's break down some of these different clinically isolated syndromes and start with optic neuritis. 01:38 And this is very important to understand. 01:40 It's a common presentation for a CNS autoimmune condition and we want to understand the clinical presentation and evaluation of these patients. 01:49 So some of the common features that we see with an optic neuritis - patients present with vision loss. 01:55 That is often unilateral and monocular. 01:58 And that localization, that presentation is critical for localizing symptoms to the optic nerve. 02:05 Vision loss, is the primary symptom and patients report decreased visual acuity. 02:10 The onset is typically gradual with new onset vision loss and reduced visual acuity over three days to two weeks. 02:17 That sub acute onset. 02:19 Pain is extremely common, and patients will tell you that it hurts when they move their eyes. 02:23 Pain with extra ocular movements. 02:26 And that is a sensitive historical detail for considering optic neuritis. 02:33 We look for an afferent pupillary defect. 02:36 And this is evaluated by a swinging flashlight test. 02:40 Looking at pupillary constriction to a light stimulus. 02:43 When we do that, and we see dilation to the light stimulus that's abnormal. 02:48 And it is suggestive of an afferent pupillary problem or a Cranial Nerve II lesion. 02:55 And patients present with a visual field defect as a result of enhancement, of irritation, of inflammation, of the optic nerve, which we're seeing here on the MRI, zoomed in on the right eye orbit and optic nerve. 03:07 And we see contrast enhancement in the optic nerve. 03:10 Active inflammation as a result of this immune attack that is contributing to this patient's symptoms. 03:19 There are some neat features that we see with the vision loss with optic neuritis and when the early symptoms that patients can report as color desaturation, which is evaluated by the Ishihara plates which you can see here. 03:31 We're looking at contrast of the colors and asking the patient to count or report the number that they see on each of these plates or cards. 03:41 Patients with optic neuritis will have desaturation of colors. 03:44 It's hard to see the contrast between the two colors and to report the numbers. 03:49 Whereas, normally, they're sharp contrast. 03:51 And we can see 45, and 74, and 6, and 42 and report those numbers on the Ishihara plates, which will be difficult to report for patients experiencing an acute optic neuritis. 04:06 There's some other features of vision loss that help localize the patient's symptoms to the optic nerve. 04:11 And in general, we think of vision loss and peripheral field loss is as either pre-chiasmatic or post-chiasmatic. 04:19 And this is an important feature to localize where in the nervous system the lesion may be to contribute to vision symptoms. 04:27 Homonymous visual field loss and homonymous visual field defects as you see on the left here with this left homonymous hemianopia are suggestive of post-chiasmatic disorders. 04:37 And this occurs from CNS brain pathology. 04:40 Posterior to the optic chiasm a tumor, or a stroke, or other lesion in that area of vision information. 04:50 And that compares to monocular vision loss. 04:52 As you see here where there's vision loss and the entirety of the left eye really sparing the right eye which is suggestive of a prechiasmatic problem and point squarely to optic nerve pathology and optic neuropathy and potentially to inflammation of the optic nerve and optic neuritis. 05:10 And when we think about monocular vision loss or an optic neuropathy, we can categorize that as painless or painful. 05:18 And pain in the presentation is important in driving us towards potential differential diagnoses. 05:24 Painless vision loss is supportive of a diagnosis of optic neuropathy. 05:29 A problem with the optic nerve that is not from inflammation. 05:32 And we think about arthritic causes or vasculitic causes, and nonarteritic causes of optic neuropathy. 05:39 In contrast, painful vision loss should point towards the consideration for a diagnosis of optic neuritis. 05:46 Inflammation of the optic nerve contributing to this patient's symptoms and it may have various causes either associated with a systemic inflammatory disorder like Sjogrens or lupus, or a primary CNS autoimmune condition like MS or a clinically isolated optic neuritis. 06:05 What are some uncommon features of optic neuritis? Occasionally we will see bilateral onset of vision loss and optic neuritis. 06:13 And you can see that in the MRI here with avid enhancement of both optic nerves that you can see in the green arrows. 06:19 And this can be seen with a variety of CNS autoimmune conditions other than MS. 06:26 Bilateral optic neuritis is uncommon in MS, but more common in a condition called neuromyelitis optica and occasionally in MOG antibody disorder. 06:36 Painless optic neuritis is uncommon and should point towards a possible other diagnoses which should be evaluated. 06:43 We can see painless optic neuritis in MS and clinically isolated syndromes but should undergo a thorough evaluation of those patients. 06:51 Severe vision loss with no light perception is uncommon in inflammatory conditions and really should warrant exhaustive workup for neoplasms or other potential causes. 07:02 Though occasionally we can see very severe vision loss in optic neuritis. 07:07 And moderate to severe disc swelling, and hemorrhages, and retina retinal exudates should also point towards other potential etiologies. 07:15 We can see papilledema or swelling of the optic nerve, and in some cases of optic neuritis. 07:20 But the swelling is really behind the optic nerve head and in the vast majority of patients presenting with optic neuritis. 07:27 We don't see abnormalities on the fundoscopic exam. 07:33 In patients presenting with optic neuritis, we see reduced visual acuity which is evaluated with the Snellen card or Snellen chart. 07:40 In general, patients are treated and we'll discuss the treatment in just a minute. 07:43 But we expect improvement both spontaneously and more rapidly with treatment, and in general for patients who have vision worse than 20/50. 07:52 Acuity will improve more than three lines on the Snellen chart over the course of six months. 07:57 And this helps us to prognosticate and guide patients as they present with an acute optic neuritis. 08:05 How about other clinically isolated syndromes? Let's talk a little bit about spinal cord syndromes. 08:09 And here we can see a representative MRI of the spine showing an area and a lesion, an area of acute edema within the spinal cord contributing to symptoms and suggestive of a autoimmune attack in the C spine. 08:22 Typical symptoms of spinal cord syndromes are a partial myelitis. 08:26 We can see symptoms of weakness, hemibody weakness, or numbness. 08:29 Sensory symptoms are common. 08:31 We can see Lhermitte's sign. 08:32 And this is when the patient's head is flexed or extended and this results in the sensation of electric shock that extends down the arm and legs as a result of ephaptic transmission, demyelination of the nerves in the C spine results in the potential for automatic transmission down those nerves. 08:51 And it's bending of the neck, activates the nerves, and results in an electric shock like sensation, which is relatively specific to a CNS lesion, in the C spine or spinal cord. 09:03 We can see paraesthesia, as again sensory symptoms are common, erectile dysfunction. 09:07 Bowel and bladder dysfunction can be present in patients with lesions in the T spine may report a band like sensation. 09:15 Something wrapping around or hugging their chest as a result of a lesion in the thoracic cord. 09:20 And since sensory symptoms predominate in many patients and often symptoms are asymmetric resulting from the eccentric location of the lesion within the spinal cord. 09:32 We can also see some uncommon features which again support a workup for other potential etiologies before making the diagnosis of a transverse myelitis. 09:41 Complete acute transverse myelitis is uncommon in clinically isolated transverse myelitis or MS and should prompt a workup for other potential inflammatory and non inflammatory etiologies. 09:53 Radiculopathy is uncommon and this is really a peripheral nervous system problem and transverse myelitis is a central nervous system disorder. 10:01 So evidence of radiculopathy should warrant a workup for alternative causes. 10:07 Areflexia is uncommon. 10:08 We really see hyperreflexia from spinal cord conditions and should see that in patients who present with acute or subacute transverse myelitis. 10:16 And segmental loss of pain and temperature sensation that does not fit a spinal cord level should warrant evaluation for peripheral nervous system conditions. 10:25 Rapid progressive symmetrical paraplegia should raise the consideration for Guillain-Barré that we can also see that rapid ascending paraparesis in patients with transverse myelitis. 10:39 And then what about brainstem syndromes? Here we're looking at atypical lesion in the brainstem. 10:43 And patients presenting with brainstem syndromes though uncommon, should warrant consideration for an autoimmune cause or a clinically isolated syndrome. 10:54 Some of the symptoms that we can see in patients presenting with brainstem syndromes include diplopia or 6th nerve palsy or 3rd nerve palsy problem with a yoking of eye movements. 11:04 We can see an internuclear ophthalmoplegia and that's where the patient is looking/gazing to one side. 11:10 And the affected eye is unable to adduct, unable to medially adduct towards the nose, and that's termed an internuclear ophthalmoplegia, results from a lesion in between the 6th and 3rd nerve nuclei in the brainstem and a suggestive of a lesion in that area and not uncommonly, an inflammatory lesion. 11:33 Ataxia is a symptom that can occur from brainstem syndromes. 11:36 Nystagmus is a result of interruption of cerebellar circuitry and fibers. 11:41 Facial numbness can be seen. 11:44 Unilateral internuclear ophthalmoplegia. 11:47 So other problems with eye movements. 11:49 Facial palsy, a weakness of the face either central or peripheral facial palsy owing from the exiting of the facial nerve within the brainstem. 12:01 Trigeminal neuralgia can be seen and this is not an uncommon presentation for a brainstem syndrome. 12:07 So, all of these are symptoms of brainstem lesions affecting either the white matter tracts or the cranial nerve nuclei as they exit the brainstem. 12:18 Then deafness. 12:19 Deafness is rare to be seen with the brainstem syndrome but is not impossible in these patients.
About the Lecture
The lecture Clinically Isolated Syndrome: Clinical Manifestations and Classification by Roy Strowd, MD is from the course Multiple Sclerosis (MS) and Inflammatory Disorders of the CNS.
Included Quiz Questions
Which statement is true of clinically isolated syndromes?
- They are single demyelinating events with no evidence of prior attacks.
- They present with optic neuritis while multiple sclerosis does not.
- They are monofocal but never multifocal.
- They are defined as each demyelinating attack leading to the diagnosis of multiple sclerosis.
Which clinical finding is suggestive of optic neuritis?
- Color desaturation
- Homonymous vision loss
- Painless vision loss
- Bilateral decreased visual acuity
- MRI findings suggestive of occipital lobe infarct
Lhermitte sign is relatively specific for which clinically isolated syndrome?
- Cervical transverse myelitis
- Lumbar transverse myelitis
- Diabetic peripheral neuropathy
- Optic neuritis
An individual presents to your clinic with a painful sensation on the left side of their face. They describe the pain as electric in nature. Where is the most likely location of the lesion?
- Brainstem
- Cervical spinal cord
- Cerebellum
- Cranial nerve VII
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |