Playlist
Show Playlist
Hide Playlist
Classic Heatstroke: Symptoms & Management
-
Emergency Medicine Heat Illness.pdf
-
Download Lecture Overview
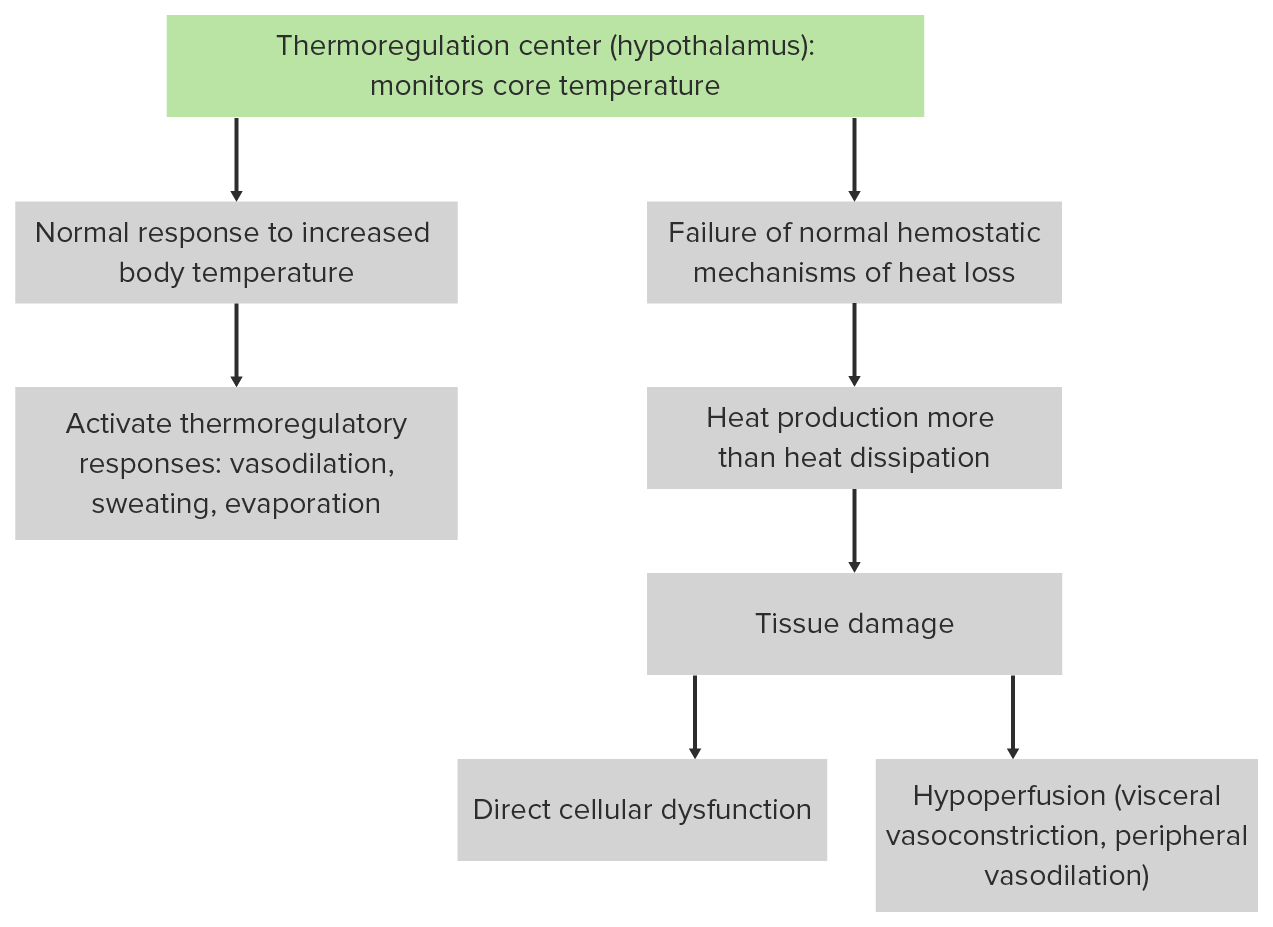
00:01 So let’s talk about a couple of cases. 00:03 So here’s one patient who has a heat related emergency. 00:07 He is a 47-year-old man. 00:09 He was found at home with altered mental status by his family. 00:14 He has a history of schizophrenia. 00:16 He’s on haloperidol and benzatropine and he’s actually pretty well controlled on those medicines. 00:21 It’s August right now and the temperatures have been between 35 and 38 degrees Celsius every day. 00:27 His vital signs include a temperature of 41.4 degrees. 00:32 He’s tachycardic to 132. 00:35 He’s tachypneic and his blood pressure is 98 over 40. 00:38 His skin is hot and dry and he doesn’t have any appreciable axillary sweat. 00:43 He has a normal pupillary exam and he moans and opens his eyes to pain. 00:49 He withdraws his extremities, but he’s not conversant and does not follow commands. 00:54 So what’s the diagnosis for this patient? This is a pretty classic example of classic heatstroke. 01:02 So heatstroke occurs during seasonal heatwaves. 01:05 This is not a disease process that you’re gonna see during the winter months. 01:08 You’re really only gonna see this during the summer and it disproportionately affects people who are debilitated. 01:14 So people who have limited access to fluids, who have limited ability to get to cool environments. 01:22 Unlike the lady in this photo, it’s really gonna affect people who have a hard time caring for themselves and don’t have a lot of control over their environment. 01:31 So risk factors for classic heat stroke include advanced age and immobility. 01:35 Again, patients who are elderly, who have limited mobility, who maybe have dementia, etc. 01:41 have a harder time with the behavioral aspects of getting out of the heat. 01:47 Patients who have psychiatric disease or dementia, patients who live in dwellings that lack climate control and don’t have access to cool environments, and also, patients who are on medications that impair the normal physiologic heat response. 02:02 These include things like neuroleptics, anticholinergics, diuretics, and antihypertensives. 02:08 All of which interfere either with vasodilation or they cause increased heat production in the body. 02:17 Pathophysiologically, heatstroke is caused by failure of normal heat homeostasis. 02:23 So basically, the body is making more heat than it’s able to dissipate and that allows an uncontrolled increase in body temperature. 02:32 This results in tissue damage which affects every single organ system. 02:36 So there’s two mechanisms of tissue damage. 02:38 One is simply heat-related cellular dysfunction. 02:41 So all of the cells in our body are designed to work at a particular temperature optimum. 02:47 And when it’s too hot or too cold, our normal cellular metabolic machinery doesn’t function the way we want it to. 02:55 So that causes direct cellular dysfunction and at the tissue level, can cause organ failure as well. 03:04 We also have hypoperfusion. 03:06 So I mentioned before that one of our physiologic responses to heat stress is to vasodilate. 03:13 The reason that we do that is to bring blood to the surface of the skin and allow dissipation of heat. 03:21 So basically, you take the hot blood from the core, you shunt it out to the periphery and hope that the heat will dissipate away into the environment. 03:30 The problem with that is that in order to maintain the blood pressure, you need to have compensatory central vasoconstriction. 03:38 So you’re shunting blood to the periphery and vasoconstricting centrally. 03:42 And when this vasoconstriction becomes severe, it can actually lead to ischemia of the viscera. 03:47 So you’re shunting all the blood out to the periphery and not providing adequate perfusion for your vital organs. 03:55 So like I said, every organ system can be affected. 03:58 The central nervous system is universally involved. 04:02 Every single patient with heatstroke will have some degree of CNS dysfunction. 04:06 Most commonly, they’ll present with delirium or coma, although, in some cases you can see seizure as well. 04:12 However, any neurologic manifestation is possible. 04:16 So patients can present with focal neurologic deficits and all kinds of different things. 04:22 Though typically, altered mental status is what you’re gonna see. 04:26 From a cardiovascular standpoint, patients will almost always be tachycardic and that’s in part to compensate for the vasodilatory response that we already discussed. 04:36 They’ll often be hypotensive because again, they’re vasodilated and shunting blood into the periphery, and you can also see tachyarrhythmias from hypoperfusion of the heart itself. 04:47 From a respiratory standpoint, tachypnea is very common and it’s associated with respiratory alkalosis. 04:55 It’s not uncommon for patients to be hypoxic as well because of pulmonary dysfunction. 05:00 From a GI standpoint, nausea, vomiting, and in some cases, diarrhea are quite commonly present and you will almost invariably see transaminitis because of splanchnic vasoconstriction and hypoperfusion of the liver. 05:16 Coagulopathy is also quite common. 05:19 Again, related to hepatic dysfunction. 05:21 And you might detect that on laboratory findings or in some cases, you might even see clinical bleeding on your physical exam. 05:27 And then lastly, these patients will often have absent sweating. 05:31 So basically, they have lost the ability to dissipate heat normally and they are no longer appropriately regulating their body temperature so they are anhidrotic. 05:43 They’re not sweating the way that they should be in response to rising core temperature. 05:49 So diagnostic criteria for classic heatstroke include one, you have to have exposure to some kind of external heat stress. 05:58 So again, this is typically gonna be diagnosed during the summer months and especially during seasonal heatwaves. 06:04 Two, you have to have severe CNS dysfunction. 06:08 Usually, delirium or coma. 06:09 Three, you have to have a markedly elevated core temperature which is typically defined as greater than 40 degrees Celsius. 06:16 Four, you have to have hot and flushed skin which is most commonly gonna be dry. 06:22 Again, anhidrosis is very common in these patients. 06:25 And lastly, you have to have transaminitis. 06:27 If you have all five of these things, then, you can diagnose classic heatstroke. 06:32 Now, there is a differential diagnosis for classic heatstroke. 06:36 Patients with thyroid storm can present with significant hyperthermia and some of the other findings of heatstroke. 06:42 Sympathomimetic intoxication, serotonin syndrome, neuroleptic malignant syndrome, malignant hyperthermia, these are all drug related causes of hyperthermia that can mimic heatstroke. 06:56 Patients in sepsis or septic shock, meningitis or encephalitis, or CNS hemorrhage can all present with temperature dysregulation and mental status changes that may mimic a classic heatstroke. 07:10 So the treatment for heatstroke first and foremost is reduction of the body temperature. 07:15 You’ve got to get the temperature down in order to stop this cascade of organ damage. 07:21 So we’re gonna always have core temperature monitoring that’s continuous for our patients. 07:27 We typically place a rectal probe and you can’t use a regular thermometer for this. 07:32 You have to use an extended range device that allows you to measure at the higher levels of the temperature continuum. 07:39 So we wanna monitor the temperature continually and we want to rapidly lower the body temperature. 07:44 So you’ve got a couple of options for how to do that. 07:47 A simple way of doing it is to use water mist. 07:50 So you basically take a misting bottle and spray your patient, and then blow a fan on them. 07:55 That will enhance their evaporative cooling. 07:57 If you have the means of doing so, you can use ice water immersion but that’s actually quite inconvenient and impractical in most Emergency Department settings. 08:06 You wanna monitor your core temperature continuously because you wanna stop actively reducing the temperature once you get down to a core temperature of 39. 08:16 You don’t wanna overshoot the mark and make your patient hypothermic. 08:20 Other treatments that you’re gonna give to your patients are volume resuscitation. 08:25 Remember, these patients are vasodilated but they’re also often dehydrated because they’ve been sitting home with heat stress, with increased insensible losses, maybe with poor p.o. intake for some period of time. 08:39 So we wanna give them volume resuscitation and they might need a large amount but you wanna be judicious and make sure that you reassess their volume status frequently because it is easy to overshoot the mark. 08:51 You wanna avoid any medications that vasoconstrict. 08:55 That’s actually gonna interfere with the body’s ability to dissipate heat and it’s gonna make it harder for you to lower the core temperature. 09:03 So you don’t wanna give any medicines that vasoconstrict. 09:07 And if the patient does have any cardiac dysrhythmias, generally, these are gonna be related to the underlying temperature elevation, and cooling is gonna solve that problem. 09:18 So you really should focus on cooling the patient down rather than using drugs to treat cardiac manifestations of heat stroke. 09:25 Lastly, antipyretics are not indicated. 09:28 So this is not an infectious process. 09:30 It’s not a process that really involves fever. 09:35 It’s a completely different physiologic mechanism, so you don’t wanna give antipyretics. 09:39 They’re not indicated and in some cases, drugs like Tylenol which affect the liver are actually harmful because the liver is already an organ that’s commonly damaged by heatstroke.
About the Lecture
The lecture Classic Heatstroke: Symptoms & Management by Julianna Jung, MD, FACEP is from the course Toxicologic and Environmental Emergencies. It contains the following chapters:
- Classical Heatstroke
- Symptoms of a Classical Heatstroke
- Management of a Classical Heatstroke
Included Quiz Questions
Which of the following drug types does NOT impair heat response?
- Statins
- Anticholinergics
- Antihypertensives
- Diuretics
- Neuroleptics
In heat stroke, the core body temperature is usually elevated above what temperature?
- 40 degrees Celsius
- 37 degrees Celsius
- 38 degrees Celsius
- 39 degrees Celsius
- 41 degrees Celsius
What is the most important aspect in the management of heat stroke?
- Rapid cooling
- Continuous core temperature monitoring
- Fluid resuscitation
- Vasopressor administration
- Adequate oxygenation
In the management of heat stroke, what type of heat transfer is done with ice water immersion?
- Conduction
- Convection
- Radiation
- Evaporation
- Transference
Which of the following statements regarding the treatment options of heat stroke is INCORRECT?
- The core temperature goal in rapid cooling is between 36–37 degrees Celsius.
- Dysrhythmias are managed with cooling in heat stroke patients.
- Antipyretics are not indicated in the management.
- Continuous core temperature monitoring is done with a rectal probe.
- Evaporative cooling can be done via water mist and fan.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |