Playlist
Show Playlist
Hide Playlist
Changes in Glomerular Dynamics 2
-
Slides RenalBloodFlow2 RenalPathology.pdf
-
Download Lecture Overview
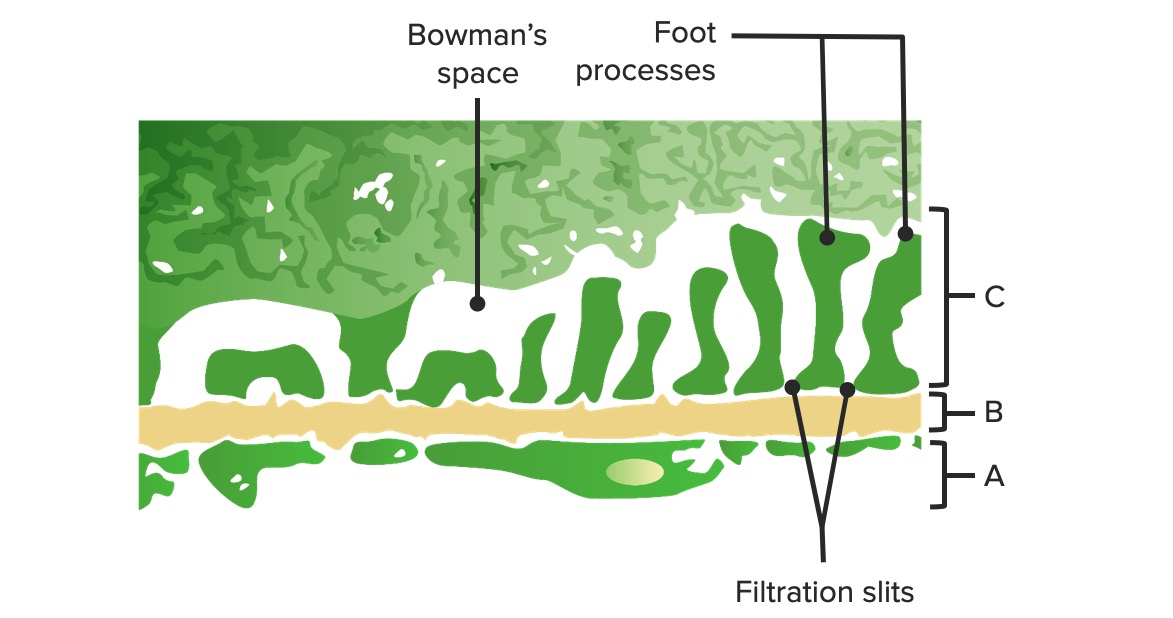
00:02 Continuing our discussion of, clinical application of renal blood flow. We are going to take that information that we have seen prior, with that table and make sure that you then associate it with that picture where for example we looked at Bowman's space hydrostatic pressure being increased with obstruction such as BPH may be a renal stone or there is increase in oncotic pressure in the Bowman's space in those dealing with something like minimal change disease, the most common cause of nephrotic syndrome in a child. Continuing our discussion and putting in a little bit more detail, but just enough where you are able to create a story for yourself. 00:41 Lets take a look at this picture. Now in the very beginning, we talked about the anatomy of renal blood flow. We began by looking at the renal artery headed towards where the hilum of that kidney. Next, the interlobar and you had your interlobular. In other words, that would be your, well, arcuate gives rise to your corticoradiate. This then gives rise to your afferent arteriole. You tell me as to what normally keeps the afferent arteriole open? Prostaglandin. Keep that in mind. Whereas on the efferent side, we continue the blood flow. There is a very important hormone known as angiotensin-II, which then causes preferentially vasoconstriction at the efferent arteriole. There is a balance that is taking place constantly between the afferent and efferent known as autoregulation in which you will then have blood flow well depending, as the range of blood pressure, maybe approximately from 40 to 140 where that blood flow will remain the same so that's your proper GFR. 01:45 Now on the efferent side, we are moving beyond the arteriole, now what's really interesting about this, is the fact the afferent, what is that? That is an arteriole is going to form a tuft of capillaries. Now usually if it's most any other part of the body, you go from arteriole, capillary and you go to venule. Anatomically that is not what is happening here, is it? It is afferent arteriole, a tuft of capillaries, efferent arteriolar. Okay. Now you go down and you travel around the nephron. It's called peritubular capillaries. This is the second set of capillary. What's another name for this? Welcome to vasa recta. Now, vasa recta eventually will give rise to inter.. go backwards now, interlobular veins, interlobar veins out through renal vein really important that you know about your renal vein especially the left side. Tell me about its course. Renal vein, renal vein, renal vein, renal vein. What's up with it? Oh look at that, that's my friend. Who? Left gonadal vein and you move towards what please? Inferior vena cava is that going to come in handy. Oh yeah we'll see. 02:55 Okay now lets add some clinical correlations. There is a prostaglandin. What is it doing? It is causing vasodilation. You take me through this, please. If there is vasodilation, then what happens to renal blood flow or renal plasma flow? Obviously increased. When you increase the amount of blood passing through afferent arteriole, please tell me what happens to hydrostatic pressure. What does P mean? Hydrostatic pressure. What is GC mean? Glomerular capillaries. How important is it for you to pay attention to those abbreviations? It will tell you between where you are. Is the capillary or is it the Bowman space. Here we're at the glomerular capillary. What are you doing? You can use that P for pushing pressure. What's your pushing pressure? Hydrostatic. 03:46 It's increased. What then happens to GFR? Increased. Very good. Now we have afferent arteriolar dilation. You tell me once more what may then remove the prostaglandin. What about that patient who had arthritis? For 10 or 15 years was taking what? NSAIDs. Anti-inflammatory. 04:07 And therefore removed or inhibite the COX a cyclooxygenase and therefore resulted in decreased prostaglandin. That decrease in prostaglandin then causes what, please? A decrease in the diameter of the afferent arteriole. What then happens to renal blood flow? It decreases. It hit the constricted afferent arteriole. What happens to hydrostatic pressure? Decrease. Pay attention to P and GC. What is P? The pushing hydrostatic pressure, pushing up the fluid out of your GC into the Bowman space. That obviously has been decreased in the setting of NSAIDs. What happens to GFR? Decreased. Now you tell me. Hmm. If this continues and that the patient is not paying attention and family medicine doctor is not paying attention, the primary care would have you? What is this patient prone to? Renal failure. Okay, lets move on. Let us now switch over to the efferent arteriole shall we? Efferent arteriole. Here we are going to bring in angiotensin II This angiotensin II works in the efferent arteriole preferentially to do what? Now let me give you the setting. I am always going to do this to you. Because otherwise you are just going to sit here and memorize. We cannot have that. So, we have a patient that has renal arterial stenosis. Yet once again. We will take as if 52-year-old male who has renal bruits and has secondary hypertension. We talked about this patient already. So renal artery stenosis. 05:45 Why was it that the angiotensin-II and the renin system was activated to begin with? That RAAS system. Renin, angiotensin II and aldosterone system was stimulated so that it can then restore some of this blood flow to the kidney because if the GFR dies, as does the kidney. 06:05 So now in the setting of renal artery stenosis, you are going to release renin. Here comes my angiotensin II, what it is going to do? Constrict the efferent arteriole. That is my topic. 06:16 Now close your eyes. May I ask you question by question? You tell me. Ready? If you are going to have efferent vasoconstriction, what is it going to have renal blood flow? It is then going to decrease. If you are going to have efferent vasoconstriction, what happens to hydrostatic pressure? Stop! Wait for me to finish. What happens to the hydrostatic pressure in your glomerular capillaries. It increases. Why did I have you stopped? Because on your exams, you want to make sure that you understand where exactly are they asking you about that hydrostatic pressure. Was it in the glomerular capillary or was it in the Bowman space? It was my question to you. Where was the hydrostatic pressure increased? Here in the glomerular capillaries obviously. When that is increased, what then happens to your GFR? It is increased. Now we go one step further. Early we talked about filtration fraction. What is that equal to? It is equal to GFR/RPF. In the setting of angiotensin II, where vasoconstriction of efferent arteriole, what happens to GFR? It increases. What happens to renal plasma flow? It decreases. What happens to filtration fraction, please? Good, it increases. Excellent! Move on. How might you move that angiotensin II and this will be contraindicated in a patient with renal artery stenosis. Why? This angiotensin II was put here by the body, hormonally, so that it can restore some of that GFR, wasn't it? Why? Because the renal artery stenosis in that patient was causing decreased perfusion. Are you following me? So that angiotensin II was there to protect the kidney. And you. Not you. But a negligent doctor did what? Not that he or she was going to take care of the blood pressure by giving an ACE inhibitor. By giving an ACE inhibitor gone is the angiotensin II, bye bye goes the patient. What happened? Remove the angiotensin II. Aren't you going to exacerbate that renal failure? Yes, you are. ACE inhibitors are absolutely contraindicated and definitely in bilateral renal arterial stenosis, but clinically also with unilateral. Keep that in mind. Lets take a look at this. There is ACE inhibitor and what does it do? Removes the effective angiotensin II. What happen to efferent arteriole? Vasodilation. I just walked you through all this. I am going to walk you through something that could be a little tricky. Watch this. Renal blood flow, efferent arteriolar vasodilation increased. Okay. Here's your question. Next what then happens to hydrostatic pressure? Efferent arteriolar vasodilation. Hydrostatic pressure is going to decrease in the glomerular capillary. Dr. Raj you said that it is increased renal blood flow with vasodilation. How could it be decreased hydrostatic pressure? Because look where the vasodilation is. Way past the glomerulus and when i said way, it is beyond the glomerulus in the efferent arteriole. So you might have increased renal blood flow, I am not arguing that point, but because of vasodilation is not the afferent, you will have a decrease in hydrostatic pressure of your glomerular capillary. What then will happen to your GFR? It will decrease. When would this be contraindicated? One more time, bilateral renal arterial stenosis and as I said clinically even with unilateral you don't get this. You just don't. Okay. Beta-blocker, maybe that might not even be a good idea because in that setting don't you need that angiotensin II? What kind of beta receptor is on your juxtaglomerular apparatus? Good. Beta-1. So therefore by giving a beta-blocker, you might also inhibit the release of renin. So Dr. Raj what am I going to use? Maybe calcium channel blocker. You have other options, you definitely do. Might be a good time for you to take a look at antihypertensive drugs. So all that pathology is just a combination of many things like tentacles, like an octopus and all of it has different arms and branches and it is all different points in which there may be if you are weak in a particular area, you go back and take a review of relevant material. 10:36 Come back though and we will continue our discussion, until we hit another wall. We build and build and build this information until you are confident.
About the Lecture
The lecture Changes in Glomerular Dynamics 2 by Carlo Raj, MD is from the course Renal Diagnostics.
Included Quiz Questions
Which of the following changes would not occur as a result of prostaglandins?
- No change in hydrostatic pressure in the vasa recta.
- Increase in hydrostatic pressure in the glomerular capillaries.
- Increase in renal plasma flow.
- Vasodilation of the afferent arteriole.
- Maintenance of the glomerular filtration rate.
Which of the following changes are NOT seen due to vasoconstriction of the efferent arteriole?
- Increase in the hydrostatic pressure in the Bowman space.
- Increase in the hydrostatic pressure in the glomerular capillaries.
- Renal plasma flow decreases.
- Increase in the glomerular filtration rate.
- Increase in the filtration fraction.
Which of the following causes a constriction of the efferent arteriole?
- Angiotensin II
- Renin
- Angiotensinogen
- Prostaglandin
- Aldosterone
Which of the following sets is paired correctly?
- NSAIDs – Vasoconstriction of the afferent arteriole
- Prostaglandins – Vasoconstriction of the afferent arteriole
- NSAIDs – Vasodilation of the afferent arteriole
- COX-2 inhibitor – Vasoconstriction of the efferent arteriole
- Angiotensin II – Vasodilation of the afferent arteriole.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I wish he was on my Med school as my teacher , But Thanks god lecturio Exists and now he is our pathology teacher