Playlist
Show Playlist
Hide Playlist
Case: 34-year-old with Dizziness
00:01 In this lecture, we'll talk about the approach to vertigo. 00:05 And let's start with a case. 00:07 This is a 34-year-old woman with dizziness. 00:10 She presents to the clinic urgently for evaluation of her dizziness. 00:15 The patient reports that she is awoken each morning for the past week, feeling very dizzy when sitting up, rolling over in bed or turning her head. 00:24 This comes and goes but seems to be provoked by moving or turning her head. 00:29 She says that the dizziness feels like the room is spinning. 00:33 She closes her eyes when this happens, and it slowly subsides. 00:37 She denies problems with weakness, numbness, tingling. 00:40 She has a history of borderline hypertension, which is being managed with diet and lifestyle. 00:46 And she's only on a multivitamin. 00:48 She has no allergies and denies a personal or family history of symptoms that prompted the presentation. 00:55 Neurologic exam shows normal finger-to-nose and heel-to-shin. 00:59 She has no primary position nystagmus but when you turn her head, she develops torsional nystagmus and becomes severely dizzy. 01:08 So what's the most likely diagnosis? Well, when we're approaching this case, as with any patient who presents with dizziness, step one is to look at the patient description. 01:19 Is this dizziness described as vertigo, the room spinning or spinning about the room? Is the description more in line for disequilibrium. 01:28 Imbalance or disbalance, or problems with the drunkenness? Or does the sound like syncope or presyncope? Lightheadedness or feeling of being faint? Hear the patient's description sound squarely like vertigo. 01:41 The patient describes that the room is spinning. 01:44 Our next step is to look at the timeline of onset. 01:48 If we're dealing with a vertigo problem, a problem with the vestibular function. 01:52 One of the helpful features will be its timeline of onset. 01:56 This patient describes an onset over about a week. 01:59 That's not acute onset over a day or chronic onset over months, this is subacute over this one week. 02:06 We know that acute pathology are things like stroke, trauma, and some intoxications. 02:12 Chronic pathology or things like neoplasms degenerative conditions, or metabolic deficiencies. 02:18 In the subacute phase, we worry about other things and this will help us to hone in on the right diagnosis. 02:24 The last are provoking factors and this can be very helpful when evaluating a patient with episodic or paroxysmal vertigo. 02:33 Here this patient's symptoms are provoked by head turning and sitting up, and moving her head. 02:39 And that's very important in establishing the diagnosis for this patient. 02:44 So what is the most likely diagnosis? Is this cardiogenic syncope? Labyrinthitis or vestibular neuritis? Post-infectious cerebellitis? A brainstem stroke? Or BPPV, Benign Paroxysmal Positional Vertigo. 03:01 Well, this doesn't sound like cardiogenic syncope. 03:03 Again, the patient's description is really more consistent with vertigo than syncope or disequilibrium. 03:09 Not all cases are so clear. 03:11 But in this case, the description squarely points us towards a vertiginous pathology. 03:18 What about labyrinthitis or vestibular neuritis? That causes vertigo. 03:22 But typically those patients present with the acute vestibular syndrome. 03:26 That's acute onset of vertigo and this was subacute in onset. 03:30 It is vertigo, and it is a cause of persistent vertigo. 03:34 Patients just don't describe episodic waxing and waning of symptoms. 03:39 The vertigo begins and is persistent until the time of presentation. 03:44 This patient presented with episodes. 03:46 This was coming and going over the last week and induced by head turning. 03:50 So this is inconsistent with a diagnosis of labyrinthitis or vestibular neuritis. 03:55 How about post-infectious cerebellitis? Those things can occur at any point in time in our subacute and onset. 04:02 That tends to be a cerebellar problem. 04:04 This patient had normal finger-to-nose, and heel-to-shin. 04:07 We didn't see those other physical exam findings that suggested an underlying cerebellar abnormality. 04:14 This also doesn't sound like a brainstem stroke. 04:17 Strokes are acute and onset, and this patients onset with subacute. 04:21 Brainstem strokes can cause vertigo, but we often see other findings. 04:26 Long track findings like weakness or hyperreflexia, Crossed findings like facial droop on one side and weakness on the other. 04:33 And we have no other associated neurologic deficits. 04:36 So this patient is most likely suffering from Benign Paroxysmal Positional Vertigo, or BPPV. 04:43 That condition is exactly what it sounds. 04:46 It's benign. 04:47 It is typically self-limited though it can recur. 04:50 Its paroxysmal. 04:51 It occurs in episodes where it comes and goes over the course of a week or several weeks as in this patient. 04:57 It is positionally provoked. 04:59 So patients with turning their head or sitting up out of bed, or lying down in bed will induce a severe episode of vertigo that is severe during the episode and then resolves over time. 05:10 And importantly, it's on the differential diagnosis for vertigo, not disequilibrium or syncope. 05:16 So this is a pretty classic presentation for BPPV.
About the Lecture
The lecture Case: 34-year-old with Dizziness by Roy Strowd, MD is from the course Vertigo, Dizziness, and Disorders of Balance.
Included Quiz Questions
Which statement is the most accurate?
- Labyrinthitis can cause acute vertigo.
- Strokes usually have a subacute onset.
- Metabolic disorders usually have an acute onset.
- Neoplasms usually have a subacute presentation.
- Strokes do not cause vertigo.
Which statement is the most accurate concerning benign paroxysmal positional vertigo?
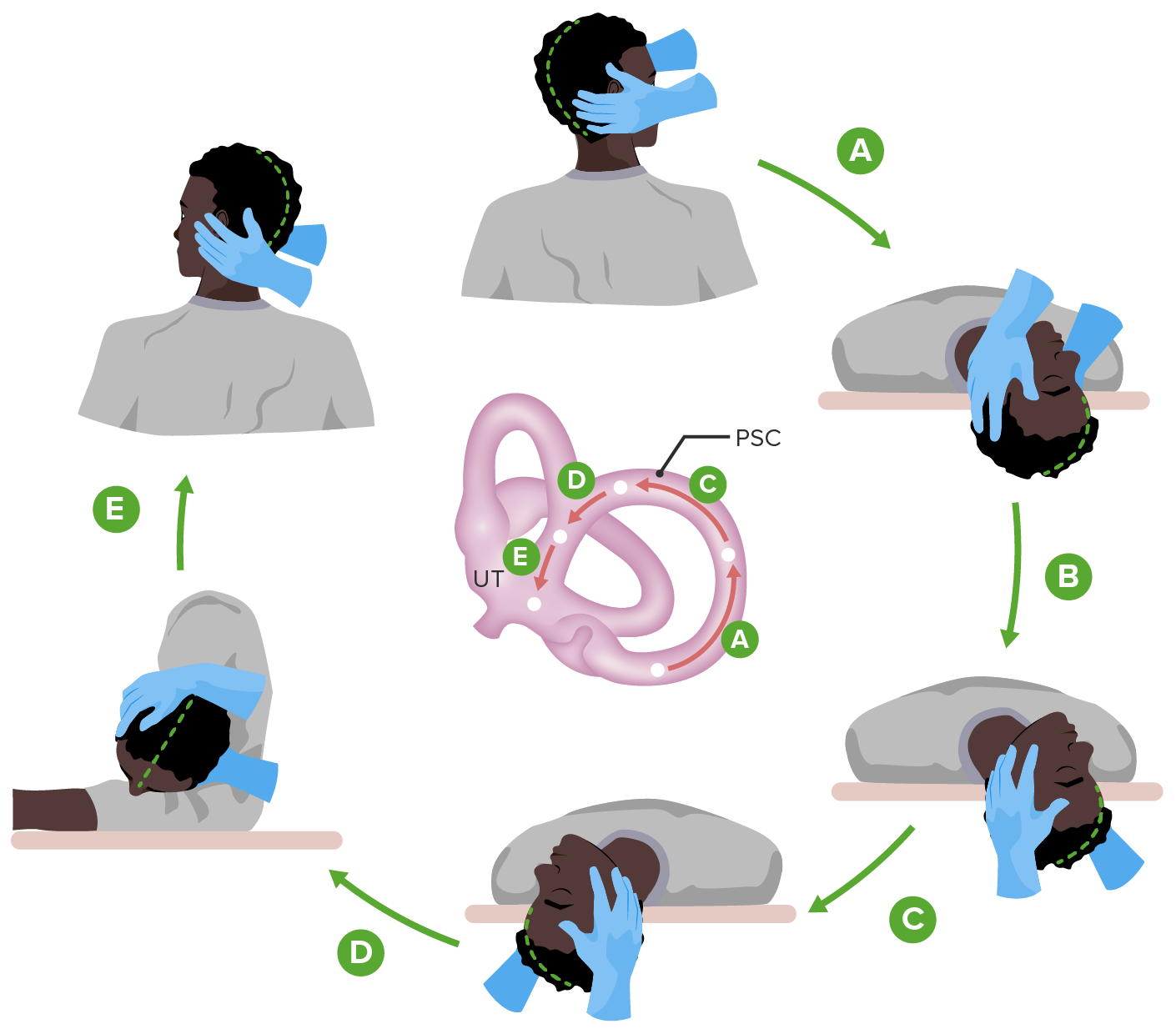
- There are specific head maneuvers that can be used to decrease symptoms.
- Vertigo occurs without any specific triggers.
- Vertigo is constant rather than episodic.
- Patients always describe a feeling of lightheadedness during the episode.
- It usually requires profound management.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |