Playlist
Show Playlist
Hide Playlist
Bacterial Meningitis: Introduction and Symptoms
-
Slides CNS Infections Meningitis.pdf
-
Download Lecture Overview
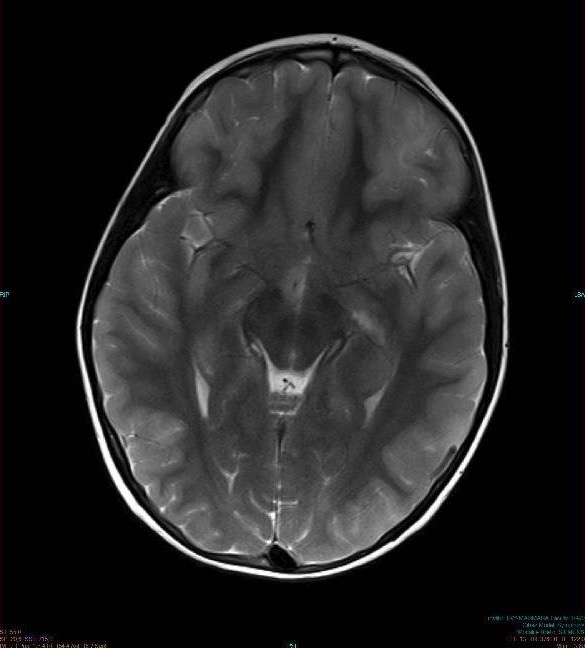
00:00 So let's learn more about meningitis. What is meningitis? Well this is inflammation of the protective membrane surrounding the brain and spinal cord, the meninges, and specifically we're going to think of meningitis as a problem in the dura, that outer and last outer layer of the meningeal surface. What are the types of things that cause a meningitis? Bacteria, viruses, fungi, and potentially an aseptic process not from an organism but often from some chemical irritation. We think about drugs like methotrexate, intravenous immunoglobulin, chemical meningitis, and sometimes carcinomatous or cancer-induced meningitis. So how do patients present? Well the classic triad is headache, fever, and neck stiffness or meningismus. 00:51 And this is a really important triad to remember. Headache is extremely common, it's seen as you can see on the slide in 90% of patients. This triad, all 3 symptoms; headache, fever, neck stiffness is only seen in about 44% of patients. But 95 will have at least 2 of those, headache and fever or headache and neck stiffness or fever and neck stiffness. And any 2 of those symptoms should point us in the direction of needing to evaluate for a meningitis. Patients can be altered and that can range from confusion to mild lethargy to severe coma depending on how rapidly this process occurs and how late the patient presents. We also see other symptoms; nausea, vomiting from increased intracranial pressure, photo and phonophobia from meningeal irritation, and we can see seizures, anything that comes from a primary brain problem. When we think about meningitis, we can categorize it into acute meningitis and chronic meningitis, and their different organisms that cause each of those and different presentations that we need to think about. Let's talk first about acute meningitis. The etiology, the causative agents are often viral and bacterial processes. This presents suddenly or acutely. And bacterial processes should be top on our list for these patients. Symptoms develop over hours to usually less than a day. Rapid diagnosis and empiric antibiotic therapy is imperative. If an acute bacterial meningitis is on your differential, antibiotics should be ordered promptly for these patients. They can decompensate really quickly and timing of administration is crucial. In patients with acute meningitis, we also think about corticosteroids. 02:39 Corticosteroids can prevent long-term sequelae from a meningitis. Patients are less likely to have hearing loss which can be a late complication from this problem or other neurologic events. Importantly, if the antibiotics had been administered, that initial antibody delivery results in lysis of bacterial organisms and a vigorous inflammatory response and the goal of steroids is to prevent that. So the steroids have to be administered before or at the time of the initial antibiotic administration. If antibiotics have been started, you can't start steroids afterwards. They don't help, they no longer prevent that late neurologic sequelae of the infection. And importantly, corticosteroids have been shown to be most beneficial in certain types of acute bacterial meningitis like H. flu, Strep pneumonia, and tuberculous meningitis. 03:30 So an important thing to note when you're evaluating these patients particularly in the emergency department. What about chronic meningitis? It's different. The etiology is different and the presentation is different. We can see certain bacterial processes, but often we're thinking viral, rickettsial, parasitic, or definitely fungal organisms as causative of a patient with chronic meningitis. We can also see non-infectious causes; neoplastic meningitis, meningitis that comes from cancer or a CNS vasculitis or chemical meningitis can present in this fashion. Patients, again, present with headache and fever as well as meningismus, but this has usually been going on for greater than 4 weeks of duration and sometimes the headache is really mild because the symptoms, the processes happen so slowly that the brain has been able to accommodate that. Fever may not be seen. Many of these patients don't have fever and it's the headache, meningismus, and other symptoms that point us in this direction. In these patients, we must ask certain questions on the history. We need to ask about recent travel to areas where fungi could be endemic. We should ask about animal exposure both occupational or travel or even at home. And the immune status of the patient is really important. Does the patient have HIV or HIV-risk factors or any other immunocompromising condition or medications. When we think about chronic meningitis, there are certain organisms that we consider. For bacteria, we need to think about microbacterium or TB. For fungi, we think about coccidio, histo, crypto is an important one to consider, blasto, and paracoccidio are common fungal infectious causes of a meningitis. There are a number of parasitic organisms that can cause a parasitic meningitis and you can see some of those here. And then there are other causes that we have talked about. Hypertrophic pachymeningitis is idiopathic. We don't know why it occurs. Leptomeningeal carcinomatosis or meningitis or metastasis comes from cancer and we can also see this with certain vasculitides.
About the Lecture
The lecture Bacterial Meningitis: Introduction and Symptoms by Roy Strowd, MD is from the course CNS Infections.
Included Quiz Questions
What is the rationale for using corticosteroids as adjunctive therapy for bacterial meningitis?
- They decrease the likelihood of neurologic sequelae.
- They have antipyretic and analgesic effects.
- They have bactericidal effects.
- They increase intracranial pressure.
- They decrease the risk of abscess formation.
Which of these clinical manifestations of meningitis is caused by increased intracranial pressure?
- Nausea and/or vomiting
- Photophobia
- Fever
- Meningismus
- ADHD
What is a common cause of chronic bacterial meningitis?
- Mycobacterium tuberculosis
- Neisseria meningitides
- Streptococcus pneumoniae
- Haemophilus influenzae
- Streptococcus agalactiae
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |