Playlist
Show Playlist
Hide Playlist
Bacterial Meningitis: Etiology & MCV-4 Meningococcal Vaccine
-
Slides Meningitis InfectiousDiseases.pdf
-
Download Lecture Overview
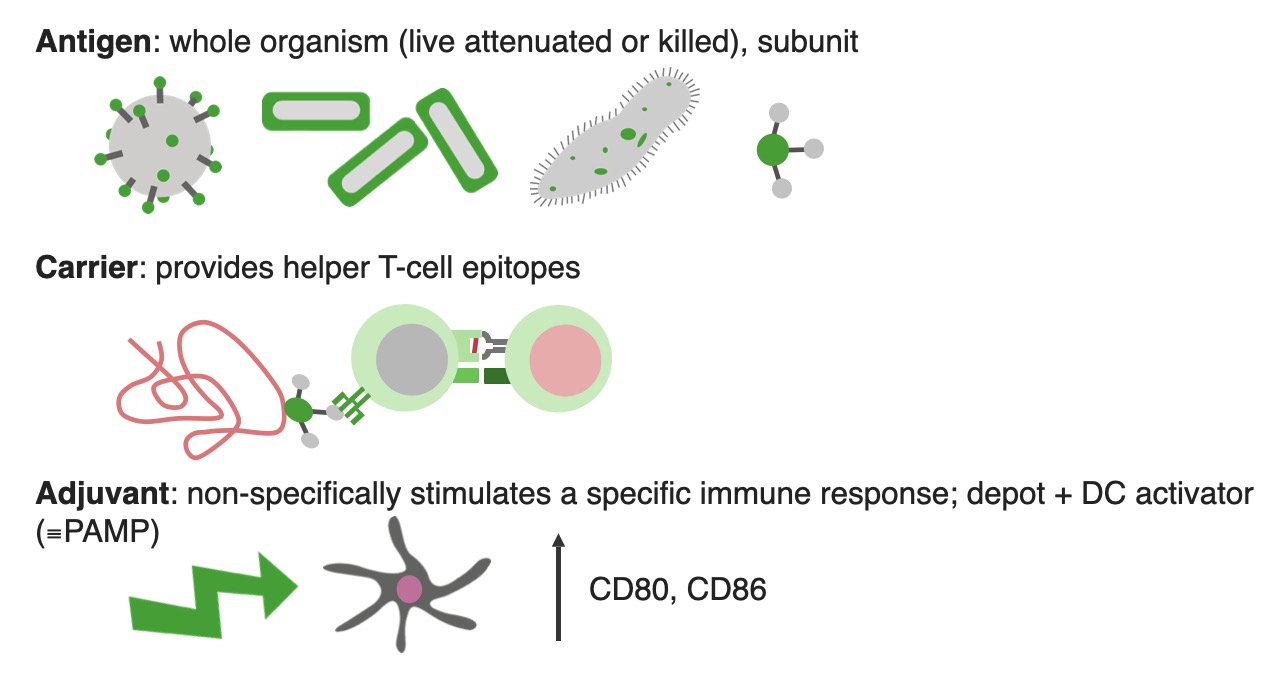
00:01 So, how do we prevent meningitis? Well, if it's the meningococcs we’re trying to prevent and we want to make sure that we prevent this in all our young people, we give them a quadrivalent conjugate vaccine. 00:18 And what this contains is capsular polysaccharide antigens from the most common types of meningococcal meningitis. 00:29 The most common is actually group B. You notice that's not listed here. 00:35 So, the other common types, A, C, Y and W135, those are the other most common types of meningococcus. 00:46 And this is recommended for all persons aged 11 to 18 years and for high risk persons up to 55 years of age. 00:56 For example, patients who would have trouble with the meningococcus, like somebody with a complement disorder, somebody with no spleen. 01:06 They are very susceptible to various kinds of bacteria in the blood stream and meningitis. 01:12 To laboratory personnel who work around cultures of the meningococcus and to travelers in the African meningitis belt, there is a band in Africa – in equatorial Africa where meningitis caused by the meningococcus is actually epidemic. 01:36 So, travelers to this area should receive this vaccine. 01:45 And they also should get a booster dose at the age of 16 or five years after the prior dose. 01:54 And all high risk children should get this quadrivalent vaccine. 02:01 So, what about persons who have been exposed to an individual who has this dreaded disease of meningococcal meningitis. 02:10 They certainly – if they've not been previously immunized, they need to receive the meningococcal vaccine and they would – that would be close contacts of somebody. 02:21 And usually, we’re talking about household contacts. 02:25 It’s controversial as to whether, for example, a physician involved in the resuscitation of a patient with this should get meningococcal vaccine. 02:36 But, personally, I would recommend, if they're involved in mouth-to-mouth resuscitation that they should get the vaccine. 02:45 In the United Kingdom, the partner of someone with confirmed meningitis who has kissed a close contact recently needs to receive antibiotics. 02:56 And also, all of those cases need to be reported to the public health authorities in the UK. 03:07 Now, you notice, we didn't talk about the most common form of meningococcal meningitis and that is group B. 03:15 And the problem with group B is that the capsule is essentially covered with sialic acid, which is very much like the surface of many mucosa in the human body. 03:31 And so, we don't develop antibodies very well. 03:36 So, if you tried to immunize with group B you don't get a good response. 03:42 So, what's been developed is this vaccine specifically targeting group B meningococcal vaccine. 03:50 It’s called Trumenba and it was licensed in 2014. 03:57 And it's the first vaccine that protects against serogroup B disease. 04:04 And the vaccine is based not on a capsule of the organism, which has that sialic acid, but on the outer membrane protein. 04:16 So, this would be indicated for immunization to prevent serogroup B disease. 04:21 And I believe that all persons 10 to 25 years of age should get it, especially since serogroup B is the most common form of meningococcal meningitis. 04:34 We also want to prevent pneumococcal meningitis. 04:39 And for that, we have 23 serotypes that we are interested in. 04:44 And these are the most common serotypes of that organism that cause disease in humans. 04:51 And we’ve got a vaccine that contains those 23 antigens. 04:57 And the efficacy overall is fair to middlin’. 05:00 It’s up to 75% of individuals. 05:05 And we are trying to target normally the elderly persons in a nursing home. 05:14 We especially want to target patients who have no spleen because the spleen is an important organ in our defense against encapsulated organisms like the pneumococcus. 05:27 But remember, in patients with sickle cell anemia, by the time they reach adulthood, they have essentially auto infarcted their spleen and have no functional spleen left. 05:39 So, they need to be immunized against the pneumococcus particularly. 05:44 And because pneumococcal disease is prevalent in elderly persons, we also recommend this vaccine for elderly persons. 05:55 And it's been shown to be cost-effective. 05:58 And unfortunately, the duration of protection is relatively short. 06:03 So, we generally re-immunize patients with the pneumococcal vaccine after about five years. 06:11 There's a new vaccine – relatively new – called the pneumococcal conjugate vaccine, PCV 13, which has 13 of the most common serotypes and it's been conjugated to a harmless variety of diphtheria toxin. 06:29 And the purpose for that is to induce some T cell associated immune response. 06:39 And you get a more vigorous antibody response with T helper cells. 06:45 And the pneumococcal conjugate vaccine is given in four doses and it does reduce the risk of invasive disease even if given to kids and adults because the disease often is spread by kids to us adults. 07:04 And it’s currently licensed for use in children and adults over the age of 50. 07:12 There's also a Haemophilus influenzae B vaccine and that has resulted in almost the disappearance of H. flu meningitis in the United States and other developed countries. 07:27 But H. influenzae B is still an important cause of meningitis in underdeveloped countries. 07:34 But we usually do not vaccinate kids at less than six weeks of age because they may get some immune tolerance to the antigen. 07:45 So, the minimum age that we begin vaccinating these patients is six weeks of age and the minimum interval is four weeks for the primary series. 07:59 And that concludes my discussion of bacterial meningitis. 08:03 I hope you found it useful.
About the Lecture
The lecture Bacterial Meningitis: Etiology & MCV-4 Meningococcal Vaccine by John Fisher, MD is from the course CNS Infection—Infectious Diseases. It contains the following chapters:
- Etiology – MCV-4 Meningococcal Vaccine
- Group B-Meningococcal Vaccine
- Pneumococcal Vaccine
Included Quiz Questions
Which of the following meningococcal strains is not included in the quadrivalent conjugate vaccine (MCV-4)?
- Meningococcal strain B
- Meningococcal strain A
- Meningococcal strain C
- Meningococcal strain Y
- Meningococcal strain W135
For which one of the following patients is the quadrivalent conjugate vaccine (MCV-4) not recommended?
- An otherwise healthy 20-year-old man
- An otherwise healthy 12-year-old girl
- A 21-year-old woman with asplenia
- A 34-year-old man travelling to Uganda
- A 54-year-old human laboratory technician
For whom is the serogroup B meningococcal vaccination recommended?
- All people 10 years or older at increased risk of meningococcal disease
- All people 11-18 years of age regardless of risk of meningococcal disease
- All infants after 6 weeks of age
- All children between 2-12 years of age at increased risk of meningococcal disease
- Only children and adults with asplenia
Which of the following patients should get the 23 serotype pneumococcal vaccination?
- A previously unvaccinated 32-year-old with sickle cell anemia
- A 75-year-old nursing home resident who received complete vaccination upon registration 3 years ago
- An otherwise healthy 45-year-old woman
- An otherwise healthy 60-year-old man
- All children over the age of 2 years
What is the minimum age for Haemophilus influenzae B vaccination?
- 6 weeks
- 6 months
- Only recommended in the elderly
- 2 years
- 11 years
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |