Playlist
Show Playlist
Hide Playlist
Asthma: Complications
-
Slides 03 Asthma RespiratoryAdvanced.pdf
-
Download Lecture Overview
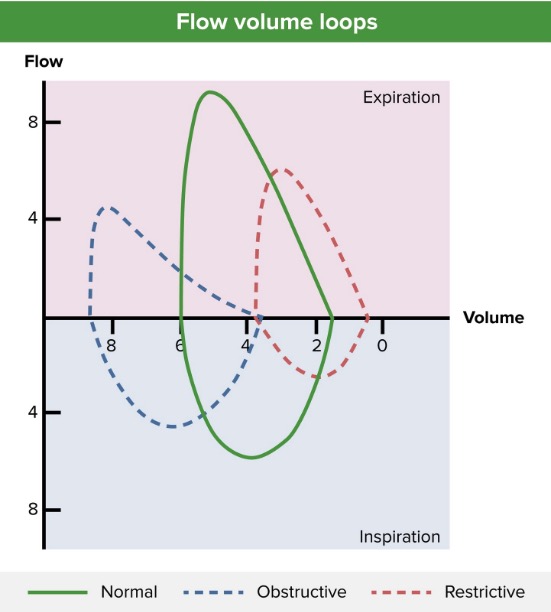
00:01 by effective treatment a few days before they present to the hospital. So asthma can get complicated by a variety of problems. You can get a sputum plug blocking of bronchus causing lobar collapse. You can get pneumothorax and pneumomediastinum. The drugs and cells also can cause complications. So excessive use of salbutamol will cause a tachycardia, and in fact, many patients taking beta2 agonist do complain of palpitations which reflects in that tachycardia. In fact, nebulized beta2 agonist such as salbutamol used in the hospital can drive down the potassium as well and you can get a recordable blood hypokalemia. Clearly, somebody with bad asthma can end up in respiratory failure requiring an intubation and ventilation and there is a very high risk situation which can lead to further complications. Patients with asthma for reasons which are not clear are more at risk with pneumonia and pneumococcal infection. The main problem long-term with asthma are the complications of the inhaled therapy. So the corticosteroids, even when they’re inhaled, do have significant side effects, and the main ones are oral candidiasis with sore mouth and Candida albicans visibly present in the oral pharynx. And dysphonia, and dysphonia is where the patient develops a horse or quiet voice, and in fact, they can lose their voice completely. 01:17 And the reason for that is that the corticosteroids, as they go down into the lungs, leads to a little bit of laryngeal muscle weakness. Both of those problems are related to the dose of inhaled corticosteroids and may limit how much you can use to control the patient’s asthma. High-dose in inhaled corticosteroids also do give you a degree of risk for osteoporosis and cataracts as well. Beta2 agonist where the long-acting or short-acting as I’ve mentioned already cause hypokalaemia and tachycardia. And the muscarinic antagonists, the Atrovent and the tiotropium could have side effects of dry mouth and can sometimes precipitate glaucoma. And all inhalers seem to, in some patients, cause a paradoxical cough and bronchospasm and not that prevent the patient tolerating from using them. 02:12 The chronic complications of asthma, well, allergic bronchopulmonary aspergillosis I’ve mentioned already. I’ve also mentioned that in patients with chronically poorly controlled disease, you may end up with irreversible airways obstruction, and that can in some very small minority patients lead to respiratory failure on a chronic basis. And then there are the complications of the therapy. Now, if you have severe enough asthma that require low-dose oral corticosteroid, step five of the treatment regimen, then the oral corticosteroids do almost invariably cause a variety of very unpleasant side effects for the patient. 02:50 The cushingoid appearance with a fat face to the central petal deposition of fat, the thin skin, the easy bruising, and osteoporosis, osteopenia, some patients may develop diabetes, and anybody on oral corticosteroids will have an increased risk of infections where the soft tissue infections, lung infections, etc. 03:11 So in the last part of this talk, I’m just going to talk about post-infective bronchial hyperactivity. Now, this is a syndrome of cough that occurs after somebody has had a viral infection. Now, that’s also what happens in asthma. Patients with asthma, they get a viral infection, the cough gets worse. The difference here is that these patients don’t know they have asthma. They get a respiratory tract infection and then they cough a several weeks afterwards. And this is either temporary period of asthma like inflammation that will go away eventually, or potentially, the first episode of asthma. Only time will tell. 03:45 The nature of the cough is very similar to the asthmatic cough. It tends to be a diurnal variation that’s worse at night, is set off by cold air, smoke, and dust, and it’s relieved by beta2 agonist. And these patients with post-infective bronchi hyperactivity do very well if they’re treated with inhaled corticosteroids. That settles down that inflammation that has occurred as a consequence of the viral infection and the patient symptoms will resolve. And then they can stop the inhaled corticosteroid at a later stage. If the cough returns, then perhaps it was the first episode of asthma. If the cough doesn’t return, then there’s just one episode of post-infective bronchial hyperactivity. 04:23 So, just to summarize the main learning points for this lecture on asthma, asthma causes intermittent reversible airways obstruction, and that causes the symptoms. Now, the clinical presentation can be very variable from mild problems of just cough alone to severe problems of cough and life threatening acute exacerbations of bronchoconstriction with breathlessness, sputum retention, etc. The diagnosis of asthma is usually relatively easy to make from the history. And the demonstration of reversible falls in the peak flow of the FEV1. The treatment is essentially dependent on inhaled corticosteroids. And these should be very effective. Poor control does result in these potentially life-threatening exacerbations that require hospital treatment. So poor control is not only a problem because it disturbs the patient’s lifestyle, but also, it makes them at risk of exacerbations that could actually end their life or at least meaning, that they have to be in the hospital for a period of time. 05:34 So, poor control needs to be addressed. Acute deteriorations of asthma require regular nebulized bronchodilators and systemic corticosteroids if they’re severe enough to come into a hospital. 05:46 And it’s very severe there are many intravenous bronchodilators, and potentially, intubation and ventilation. Thank you for listening today.
About the Lecture
The lecture Asthma: Complications by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following is NOT a sign of severe and immediately life-threatening asthma?
- Reduced PaCO2
- Bradycardia
- Reduced level of consciousness
- Inaudible breath sounds on lung auscultation
Which electrolyte abnormality can be caused by increased beta agonist use?
- Hypokalemia
- Hyperkalemia
- Hypocalcemia
- Hypercalcemia
- Hyponatremia
Which of the following is NOT a known side effect of chronic inhaled corticosteroid therapy?
- Tachycardia
- Oral candidiasis
- Dysphonia
- Osteoporosis
- Cataracts
Which of the following may be a complication of oral corticosteroid therapy?
- Osteoporosis
- Xanthelasma
- Waterhouse-Friderichsen syndrome
- Pulmonary embolus
- Fever
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |