Playlist
Show Playlist
Hide Playlist
Anterior Segment of the Eye – Anatomy Review
-
Slides Structures of the eye.pdf
-
Download Lecture Overview
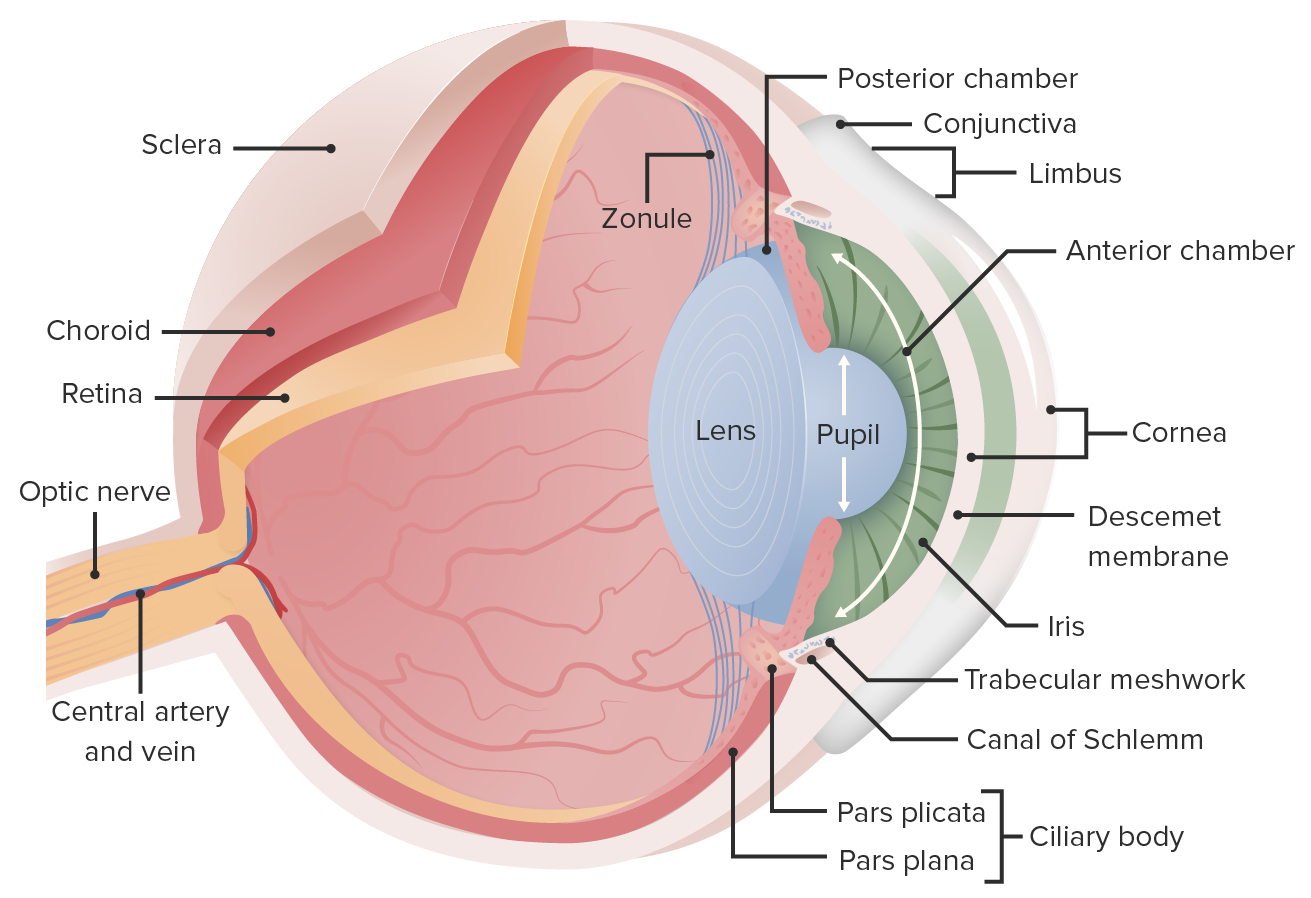
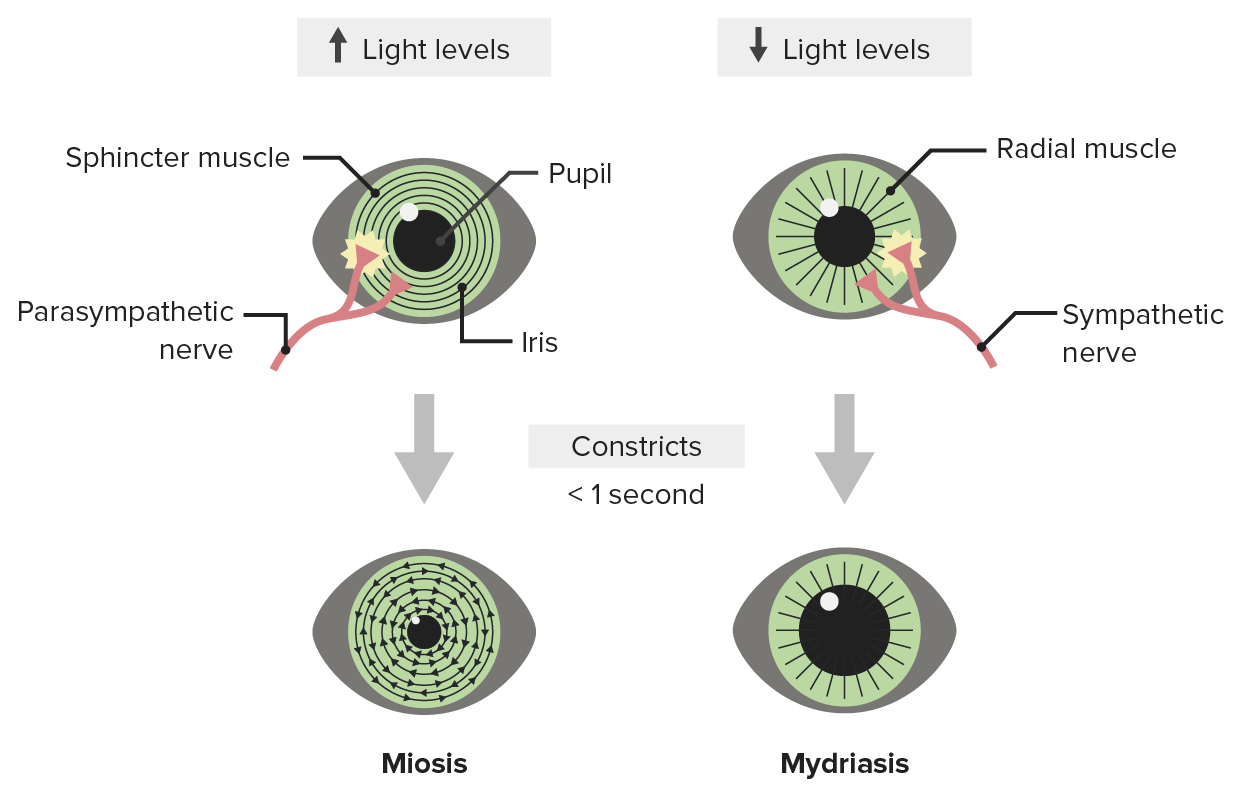
00:01 Here we are with the cornea. That's what we talked about it last. The cornea. 00:05 What does the cornea really look like? Well, it turns out it is a cellular structure, it has to be clear though, we need to be able to get light through it. 00:13 So the cells, and the underlying matrix have to be really nicely oriented and aligned. 00:20 So that light doesn't get blocked. It does get refracted. 00:25 A lot of the refractive power of the eye outside of the lens is because of the cornea. 00:32 So, looking at this image that just came up, the epithelium on the right-hand side of a stratified squamous epithelium. 00:39 It's a lot like what's on the skin, except that it's not keratinized. 00:43 It sits on a basement membrane that's Bowman's layer. 00:46 And then deep to that is a relatively less cellular stroma, that has got a lot of connective tissue in it. 00:55 But again, everything in here has to be perfectly aligned and then deep to that is the endothelium. 01:01 The endothelium sits on a descemet's membrane that separates it and the stroma. 01:08 Now, the endothelium here in this case, is a very leaky endothelium and any water that gets into the stroma needs to be somehow moved into the rest of the eye and then out, so that you don't have kind of an opaque vision. 01:22 So, too much water in the stroma or in the epithelium can give you cloudy sorts of vision. 01:28 Endothelium on the inside, sitting on descemet's membrane, allows that to get out. 01:34 Okay, what does it really look like? Here's an H and E histology of that. 01:38 And again, on the right-hand side is a stratified squamous non-keratinizing epithelium sitting on top of Bowman's layer, the basement membrane, the underlying stroma, and then the epithelium. We'll talk about diseases related to this. 01:52 But again, what's being shown here is that the light has to get transmitted all the way through the cornea. 01:57 And it has to be relatively clear. There are diseases associated with the cornea. 02:07 So, astigmatism, remember we talked about if there's an irregular cornea, that can be a cause of astigmatism, with multiple focal points hitting on top of the retina, you can have infections of the cornea, you can have trauma to the cornea. 02:21 In a subsequent session, we'll talk about all various things that can affect the cornea. Alright, cornea. 02:28 Next up is the iris, and when you look into someone's baby blue eyes, or those brown eyes, or hazel eyes, or the lavender eyes of Elizabeth Taylor, what you're looking at is the iris. 02:42 And the iris is actually a really interesting structure as well, it is going to be the mechanism by which we only allow light to come through the pupil. 02:51 It keeps too much light from coming in. 02:53 So that's why it's so heavily pigmented, and keeps that from happening. 02:58 In albinos, it's actually relatively less pigmented and that can cause problems, photophobia associated with albinism. 03:05 Anyway, in most of us, it's pigmented, it's heavily pigment. 03:10 And we're going to look at a little bit more detail of what's in the iris here, but it's a structure that kind of dangles off the ciliary body, that's going to be up top, and it sits in front of the lens. 03:21 The HD image on the bottom now. The little tiny arrowhead is pointing to a simple squamous epithelium, it sits on top. And underneath it are a variety of smooth muscle cells and matrix. 03:35 So, there's a lot of smooth muscle in the iris. 03:38 That's how we get the iris to go wide, or to constrict down. 03:45 And then, on the very left-hand side. See, all that dark, pigmented material? Well, in fact, those are pigmented cells, pigmented epithelial cells that are responsible for the color of the eye and that will keep the light from coming through. 04:00 So, there are multiple kind of interesting pieces to this, but the smooth muscle and the pigment are probably the ones that will pay the most attention to. 04:10 So, because of all the smooth muscle that's there, the pupil, we can make the iris constrict or relax. 04:18 And so, the normal pupil is some diameter, all the way around. 04:21 And then, when we want it to constrict, we want to limit the amount of light coming through or if we're looking at something nearby to accommodate, we constrict the pupil. 04:32 It's called meiosis. And we have circular bundles of smooth muscle, that are in that iris, as we already showed you. And they will constrict kind of like the diaphragm on a camera. 04:42 When you want them to dilate, that's called mydriasis. 04:46 Mydriasis. And we get a radial pulling of the muscle to open up the iris to enlarge the pupil so that we get more light through. 05:01 There are a number of diseases. 05:04 And we'll spend an entire session talking about these that are associated with malfunction of the iris. 05:10 So-called Marcus Gunn pupil, Horner Syndrome. 05:13 We can have inflammation of the structure. We can have trauma to the structure. 05:17 Next up is the lens. So the lens, kind of like the cornea. 05:22 Interestingly enough, it is a cellular structure, there are cells there, but it's still got to be transparent. So, how does it do that? Looking at the lens. 05:33 So, it's also important that the lens is not a symmetric kind of biconcave structure. It is biconcave but it's not symmetric. The front of the lens tends to be flatter than the posterior aspect of the lens. 05:47 We are looking at a cartoon there of what the lens looks like. The little fibers coming off the top are so-called zonular fibers. 05:55 They're going to be attached to the ciliary body, they're going to allow us to stretch or relax the lens to get various refractive forces. 06:04 Okay, but on the front of the lens, there are actually cells. 06:09 So, the very thin structure all the way out, that's going to be - in this particular case is just going to be part of an iris. And this is from an animal preparation. 06:22 But the lens itself is that big hunk of pink, and the little blue rim around the outside. 06:27 Those are cuboidal cells, epithelial cells that are going to be responsible for making lens matrix. 06:35 And as they proliferate, and then, go about their business, they kick out their nuclei, they kick out all of the organelles, and they become the lens fibrils that are that massive area of pink. 06:52 So, those are kind of residual lens cells that came from the anterior part. 06:59 So, the only - the anterior part has the cells, the whole rest of the lens are just these a nuclear, a organellar, non-organellar fibrils that sit there, and they have to be also perfectly aligned. 07:12 So that we can get light through there, to be transparent, but it also, they do have refractile properties. 07:20 So, in aggregate, they will bend light, going through all of this residual cellular structure. 07:30 And again, the point is we want light to be transmitted all the way through, both the cornea and the lens. 07:37 But we do want it to be focused, we want it to be bent, refracted appropriately, so it hits the retina, just so. There are clearly problems associated with the lens, pathology that we'll talk about in a separate talk. 07:54 These include presbyopia. So, this is - as we get older, the lens gets stiffer. There is less ability of the zonular fibers to pull it and so, it gets much more difficult in older folks, like me, to see at certain distances, including up close. 08:16 So, previously, my lens had been pretty pliable. 08:20 As I get older, less so. That's presbyopia. 08:23 You can have clouding of the lens, that lenses living tissue. 08:27 It's there, and it can get exposed to ultraviolet light it can be subject to the vagaries of diabetes and other things, that will cause clouding of the lens, and not as much light gets through. 08:41 We can have ectopia lentis. This is actually because of the suspensory ligaments, the zonular fibers, that normally stretch or relax the lens, that can also cause lens subluxation. You can get motion of the lens away from where it should be. That's ectopia lentis. 09:00 Alright. So, we'll talk about that. We'll have a whole session - hooray - on lens. 09:05 Okay, so now, we have a little box there. 09:09 We're going to talk specifically about this area. 09:12 This is the ciliary body, and the zonular fibers. 09:15 So, getting up close and personal, you can see the iris. You can see where the pupil is. You can see where the lens is. 09:22 We're going to be looking at the structure. And it's kind of like, gee, it's a little tiny thing. 09:26 It can't be too important. No, it's way important. 09:28 So, the ciliary body which is right there, and it's continuous with the choroid. 09:37 And it's continuous with the iris. That ciliary body is going to be responsible for relaxing the zonular fibers. Those little ligaments that will stretch or relax the lens. 09:50 Okay, so allows the lens to accommodate appropriately until the lens becomes too stiff, and then you get presbyopia, okay. 09:56 The ciliary body is also going to be responsible for the production of aqueous humor. 10:01 So, again, we're very interested in making sure that all components of the eyes are well lubricated. 10:05 And some of these are relatively avascular structure. 10:09 There's no - there are no vessels in the lens. 10:12 So, we need to make sure that we keep it well lubricated. 10:18 And so, we're going to produce an aqueous humor that's going to be in our anterior chamber. 10:24 And when the ciliary body has problems with that production, overproduction or inadequate clearance, we can get glaucoma, too much pressure in the front of the eye. 10:36 Okay. So, we've covered all of these lens apparatus so far.
About the Lecture
The lecture Anterior Segment of the Eye – Anatomy Review by Richard Mitchell, MD, PhD is from the course Introduction to Ophthalmology.
Included Quiz Questions
What type of epithelium is present in the cornea?
- Stratified squamous epithelium
- Keratinized epithelium
- Cuboidal epithelium
- Columnar epithelium
- Pseudostratified epithelium
What condition is characterized by an irregular cornea?
- Astigmatism
- Nystagmus
- Strabismus
- Ametropia
- Hyperopia
What condition is associated with albinism?
- Photophobia
- Blepharitis
- Glaucoma
- Iritis
- Cataracts
What term refers to the loss of pliability of the lens?
- Presbyopia
- Cataracts
- Glaucoma
- Mydriasis
- Myopia
Overactivity of the ciliary body results in what condition?
- Glaucoma
- Astigmatism
- Hyperopia
- Presbyopia
- Cataracts
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |