Playlist
Show Playlist
Hide Playlist
Angiodysplasia
-
Slides GIP Angiodysplasia.pdf
-
Download Lecture Overview
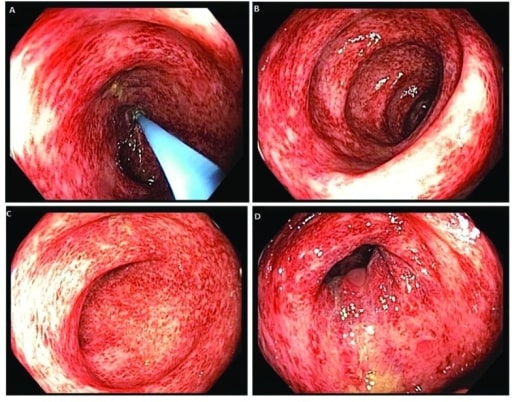
00:01 All right. On this topic of Angiodysplasia, we will spend a few minutes discussing exactly what this is and how it presents and what to do about it. 00:11 Angiodysplasia is a vascular malformation that will occur somewhere within the GI tract. 00:18 It can occur anywhere from the esophagus to the rectum. 00:22 Most commonly, it's going to occur in the colon and that's what we're going to emphasize in this particular talk. 00:28 The epidemiology. Your typical patient with Angiodysplasia is going to be elderly, over the age of 60. 00:36 Most of the Angiodysplasia actually occurs in the left-sided colon. 00:40 Approximately 6% of lower GI bleeds and 8% of upper GI bleeds are associated with Angiodysplasia. 00:51 The things that are associated with this include aortic stenosis, the so called Heyde syndrome, end-stage renal disease, the use of ventricular assist devices, Von Willebrand's disease which may be a hereditary form of Angiodysplasia and Osler-Weber-Rendu syndrome which is also a hereditary basis for having Angiodysplasia. 01:17 The pathophysiologic is basically a malformation between the arteriovenous side. 01:25 What is being shown here on the right-hand side is an artery, the branches and the capillaries that reconstitute into post-capillary venules and then, into a vein. 01:36 What happens in an arteriovenous malformation in Angiodysplasia is that we have direct connections from the artery into the vein so that we bypass the very low pressure in highly distributed capillary system. 01:54 The formation of such arteriovenous malformations, Angiodysplasia between otherwise health vessels can be associated with low-grade venous obstruction of the submucosal veins may be due to reduced precapillary sphincter tone with the opening of arteriovenous communications. 02:14 The association with Von Willebrand's disease or with abnormalities in the processing of Von Willebrand's factor means that we have higher molecular weight multimers of Von Willebrand's which tends to drive these AVMs or Angiodysplasia for unclear reasons. 02:32 And then, the congenital vascular hyperplasia associated with Osler-Weber-Rendu are a variety of mutations associated with vascular hyperplasia. 02:41 The clinical presentation is typically painless GI bleeding. 02:46 The patient doesn't even have any other symptomatology and depending on the amount of blood, may be completely unaware that there has been ongoing bleeding. 02:55 If there is a lot of blood and because of the location typically on the left side of the colon, then, you may have hematochezia or bright red blood per rectum. 03:02 then, you may have hematochezia or bright red blood per rectum. 03:06 If you were to have an Angiodysplasia and arteriovenous malformation more proximally, you may have hematemesis or vomiting of blood. Clearly, if you're using blood chronically, particularly, in a geriatric population, these patients will have anemia. 03:23 And then, will have symptoms associated with the loss of blood. They will be weak. 03:27 There may be hypotension. So, things that you can figure out pretty much from first principles. 03:34 How do we diagnose this? So, we have a patient, geriatric, who is - got clear anemia and we don't have any bleeding source. But we do have occult blood positive in the feces. 03:50 That makes us start to think that this might be a possibility. 03:53 We can do a complete blood count and formally document the anemia and the cause of the anemia, whether it's iron deficiency or something else. We can do endoscopy. 04:02 A colonoscopy will allow us to actually visualize these legions if they are bleeding significantly enough. 04:09 And the gold standard overall is angiography or we will inject radio contrast material and see it extravasate as you see here on the right-hand side into the lumen of the GI tract. 04:22 What's shown on the left-hand side is what this legion would look like on colonoscopy. 04:27 It looks just kind of like a bruise or a vascular malformation that is sitting just below the submucosa. 04:36 How do we manage this? So, we can do an endoscopic treatment if you identify exactly where this is with colonoscopy, you can go in and radio frequency ablate it, just blast it. 04:49 You can do angiographic embolizations. So, you can identify the vessel that feeds the area where the bleeding is occurring and you can put in material to cause vascular occlusion and then, focal ischemia infarction of that area. And for rather larger vessels or malformations or for rather bloody, substantially bleeding malformations, then, we can resort to surgery. With that, we'll close.
About the Lecture
The lecture Angiodysplasia by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
Which is NOT associated with angiodysplasia?
- Cardiac stents
- Aortic stenosis
- End-stage renal disease
- Von Willebrand disease
- Ventricular assist devices
What is the gold standard diagnostic test for angiodysplasia?
- Angiography
- Fecal occult blood test
- Complete blood count
- Endoscopy
- MRI
Which is a common symptom of angiodysplasia?
- Hematochezia
- Thrombocytopenia
- Mucositis
- Vomiting
- Chest pain
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |