Playlist
Show Playlist
Hide Playlist
Acute Ischemic Stroke: Major Treatment Types
-
Slides Management of Acute Ischemic Stroke.pdf
-
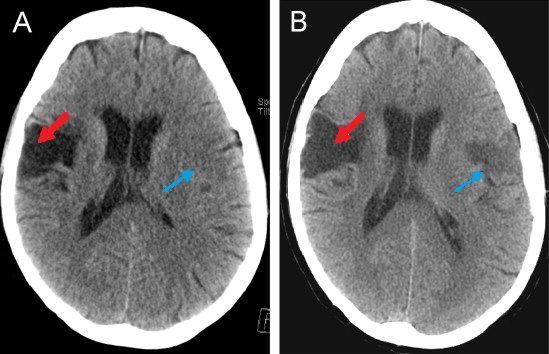
Download Lecture Overview
00:00 Now let's talk about the types of interventions. So we've evaluated the patient in the ER, we've done those initial steps, we've determined that we think this is an ischemic stroke, we'd assessed the stroke with the NIH stroke scale, the patient presented within a time that we can intervene. What are our options for intervening? Well, the first is intravenous tPA, IV tissue plasminogen activator. This is a clot-busting medication. It is a lytic agent or a fibrinolytic. It works by lysing the clot, increasing the fibrinolysis around this acute clot within one of the cerebral vessels. The second option for intervention is intra-arterial thrombectomy. This is not an intravenous procedure, this is done and performed thru catheter angiogram. A catheter is inserted into the groin, put in to the arteries, trafficked up to the cerebral circulation. And we can either remove a clot or inject intra-arterial tPA or tissue plasminogen activator to try and remove and bust up that clot typically in a proximal blood vessel. Here you can see this is an intra-arterial procedure, there is clot removal. We can also use balloon for angioplasty and opening up an area of stenosis or clot as well as stent placement in selective procedures. So let's walk through how and when we would use each of these interventions. So for thinking about things from the standpoint of the patient, the patient is seen in the field, we identified the stroke signs and symptoms, EMS is activated. There are important interventions that are done at the scene, evaluating glucose and blood pressure, managing blood pressure and evaluating other hemodynamics and vital signs, airway breathing and circulation. These important interventions are already started as the patient is being brought to the emergency department and should typically occur within 10 minutes of arrival at the minimum. We plan and anticipate and expect to do a neurologic assessment at the time that the patient arrives in the emergency department and for these patients these code strokes or brain attacks there are a number of physicians and providers that are all in the emergency department waiting for the patient so that this can be done quickly and effectively. We like to see that stroke scale done within 25 minutes of arrival so that we can start to confirm that this is a stroke and determine the size of stroke and the necessity of intervention. A non-contrast head CT is done on all patients to determine whether this is a hemorrhagic or an ischemic stroke. We're evaluating for head bleed with the CT. We can see signs of an ischemic stroke, but the goal of this test is to evaluate for hemorrhage. If a hemorrhage is found, the patient is moved on to a hemorrhagic stroke pathway with consultation of neurologist with or without neurosurgeon and management at the appropriate level of care. If there is no head bleed, then we look for possible intervention for an ischemic stroke with some type of fibrinolytic therapy or thrombectomy. The first assessment is to determine whether the patient qualifies for fibrinolysis for intravenous tPA or some other lytic therapy. If the patient does meet criteria for a fibrinolytic, our goal is within 60 minutes of presentation to be administering IV tPA. 03:25 And that 60-minute time point is critical. The shorter we can make that, the better it is for the patient. If the patient is not a candidate for fibrinolytic therapy, we would consider aspirin followed by conservative management or in selected patients intravenous thrombectomy which we'll talk about in the next series of slides. Importantly, during that assessment, we're looking for contraindications to tPA to lytic or fibrinolytic therapy. 03:53 There are some absolute contraindications and some relative contraindications and this is an area of movement in the field of stroke with changes that are being implemented in the guidelines frequently. But in general, we think that stroke within 3 months is a contraindication. So patients who have had a recent stroke or a major surgery within 14 days; patients who have a history of intracranial hemorrhage, we wouldn't want to call us that again. Patients with sustained elevated systolic blood pressure at higher risk of hemorrhage, we work to control that either the systolic or diastolic blood pressure, but if we can't we would worry that this increases their risk of hemorrhage. If aggressive treatment is needed to lower the blood pressure, that's okay but if they cannot achieve blood pressure control, we would be concerned. Patients who have symptoms suggestive of subarachnoid hemorrhage, we wouldn't want to do lytic therapy in that situation. GI bleeding is nowadays a relative contraindication, but recent GI bleeding would be certainly be a concern. Arterial puncture. Heparin within the last 48 hours or active use of Coumadin with an INR greater than 1.5. In addition, there are some relative contraindications. If the patient's already improving, we do wonder "Is this actually a stroke?" If the patient had a seizure, we may be dealing with a seizure as opposed to stroke but we want to make sure that stroke wasn't inciting event for the seizure. Patients with severe thrombocytopenia, we need to be concerned. Glucose abnormalities can also masquerade a stroke so we're seeing some of those stroke mimics. Patients with really large strokes maybe at higher risk for hemorrhage and so we'd worry about that. As well as patients who already have large territory of infarction on the CT. If we're already seeing that ionic or even vasogenic edema on the CT, there's a higher risk of hemorrhage in those patients. When we're giving IV tPA, it's given at a flat dose for all patients and that those is based on weight. 0.9 mg/kg for each patient again based on weight is divided as 10% as an IV bolus over 1 minute and then 90% of the dose is given over a 60-minute infusion. The max dose is 90 mg. Whenever we're thinking about any intervention, we're balancing benefit and risk, and IV tPA is not free. There are side effects and risks. The risk that we would consider with IV tPA as with any fibrinolytic therapy is that of bleeding. And for patients who are having a stroke, the bleeding risk is bleeding in the brain. In studies, IV tPA is safe. It has an estimated 10 times greater chance of benefit than risk of harm. And that is substantial. In addition, the association of IV tPa with risk of intracranial hemorrhage is low. In some studies, that's as low as 1 in every 15 patients and recently as we learned to select appropriate patients, that risk of harm has gone down even further. What about thrombectomy and intra-arterial therapy? How does that work? Well, as you see here, it's done through a catheter. That catheter is inserted typically into the femoral artery and maneuvered up into the cerebrovascular circulation. 07:05 That catheter is put into the vessel where a proximal clot lies. Very distal clots, we may not be able to access, but proximal and mid proximal clots are easily accessible through catheter procedures. There are a number of procedures that can then be done. The clot can be removed and that's thrombectomy. We can administer intra-arterial tPA to bust up the clot intra-arterially, that reduces the risk of bleeding but gives that important fibrinolytic therapy. We can balloon open the clot with a balloon and that's called angioplasty, or stented area of stenosis if needed. Each of these are determined at the time of the evaluation with a data supporting removal of clot early and as early as possible after the stroke as being most effective for patients. Let's walk through a typical algorithm for understanding how we integrate intra-arterial thrombolytic therapy. So again, we're dealing with patients who are suffering an acute ischemic stroke. When the stroke team is activated, our thrombectomy interventionalists are also alerted. Patients undergo stat CT of the head without contrast to rule out hemorrhage and help to rule in ischemic stroke. Patients who may be stable or not have disability or rapidly resolving symptoms, we would not consider intra-arterial intervention. The data supports use of intra-arterial intervention at varying time points and with patients who have substantial deficit or deficit that can be rescued. 08:39 Here you can see defined in this algorithm in an NIH stroke scale of greater than 4 or isolated aphasia or hemianopsia or other deficits that would lead to significant dysfunction down the road. Patients presenting within 4-1/2 hours are candidate for IV therapy and if IV therapy is not working, we may consider intra-arterial thrombectomy. For patients in this in between period of time or greater than 8 hours, we would consider intervening particularly those where additional imaging suggest the opportunity to salvage our patient's symptoms mismatch with the imaging indicating a large area of penumbra. In some cases even with fluctuating symptoms, for patients who have severe strokes and where angiography may have the potential to rescue that patient's symptoms prior to a large territory stroke, we would also consider intervention. So we consider endovascular therapy and that's thrombectomy for removal in patients who are less than 6 hours and have clear evidence of substantial stroke that would be benefited from intervention. Those patients would undergo emergent catheter angiography and revascularization. For patients in the 6 to 8-hour time point, we would consider emergent catheter angiography and mechanical thrombectomy for patients particularly where there is a perfusion mismatch that indicates an area of brain to salvage. And then for patients who are longer hours, for those patients we would consider for posterior circulation strokes where long-term neurologic deficits could be devastating, or again if there is considerable perfusion imaging that suggests an area of penumbra to salvage. So again, when we're evaluating patients for an acute ischemic stroke, intervention is key and time is brain. We ask patients to present and to act fast to present with facial droop or arm weakness or signs of speech abnormalities and come in as early and as timely as possible. Those patients should be evaluated with an algorithm to expedite that evaluation and consider either intravenous or intra-arterial therapy.
About the Lecture
The lecture Acute Ischemic Stroke: Major Treatment Types by Roy Strowd, MD is from the course Stroke and Intracranial Hemorrhage.
Included Quiz Questions
What is the primary purpose of a CT scan in a patient who presents with stroke symptoms?
- To determine if there is any sign of intracranial bleeding
- To determine the size of the stroke
- To determine the location of the stroke
- To determine the level of disability the stroke will cause
- To determine whether a patient is a candidate for tPA
What is the next step in the management of a patient with an acute ischemic stroke (without any bleeding on CT) if they are not a candidate for tPA due to the time elapsed since the last known time without symptoms?
- Give aspirin
- Obtain brain MRI
- Obtain neurologic consultation
- Admit to ICU or stroke unit
- Administer anticoagulants (heparin or low-molecular-weight heparin)
What is one of the absolute contraindications to tPA for acute stroke?
- Open heart surgery 1 week ago
- Previous ischemic stroke 1 year ago
- Hip replacement surgery 1 month ago
- Systolic blood pressure of 165
- Diastolic blood pressure of 100
What is a relative contraindication to tPA for a patient presenting with ischemic stroke symptoms?
- Glucose < 50 since hypoglycemia may mimic stroke
- Mild to moderate stroke symptoms on the NIH stroke scale
- CT with no abnormal findings around the middle cerebral artery
- Symptoms rapidly worsening in the emergency department
- Stroke symptoms waxing and waning for more than 24 hours
How is a thrombectomy performed in a patient with a middle cerebral artery (MCA) stroke?
- IV catheter through the femoral artery up to the cerebral circulation
- IV catheter through the femoral vein up to the cerebral circulation
- IV catheter through the carotid artery up to the cerebral circulation to place a stent
- IV catheter through the subclavian vein up to the cerebral circulation
- Transcranial access to the middle cerebral artery to deliver intra-arterial tPA
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |