Playlist
Show Playlist
Hide Playlist
Acquired Arrhythmia
-
Slides Arrhythmia.pdf
-
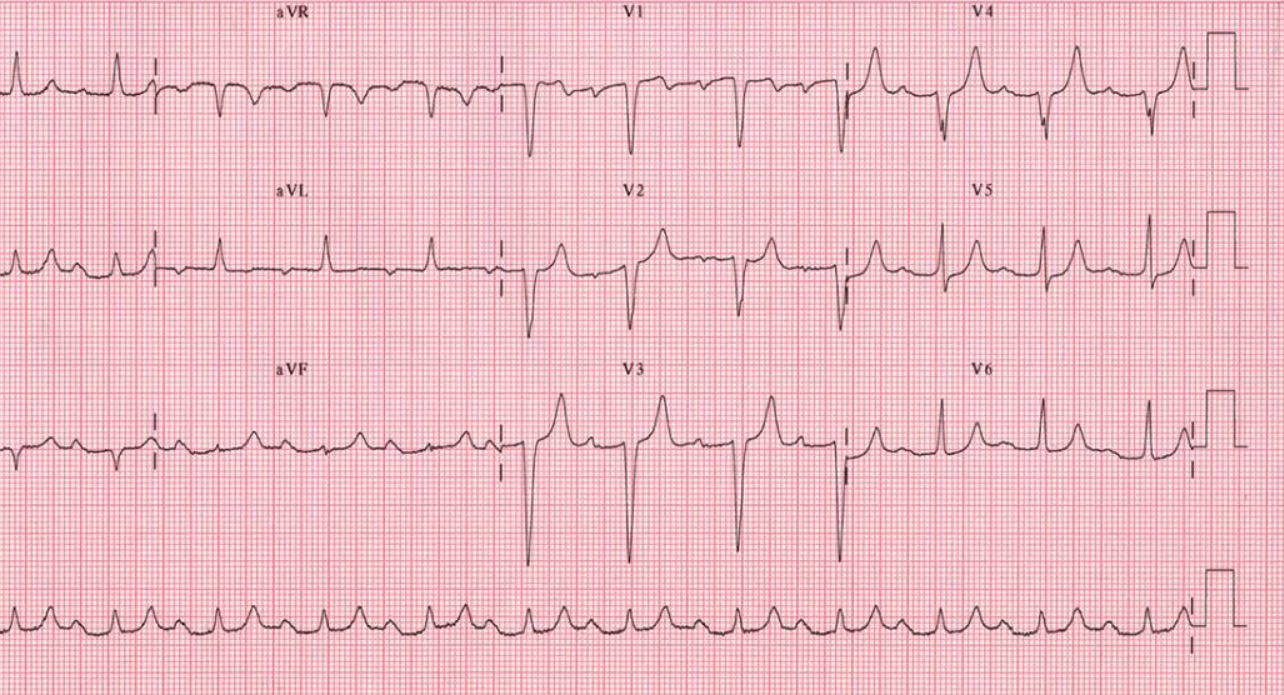
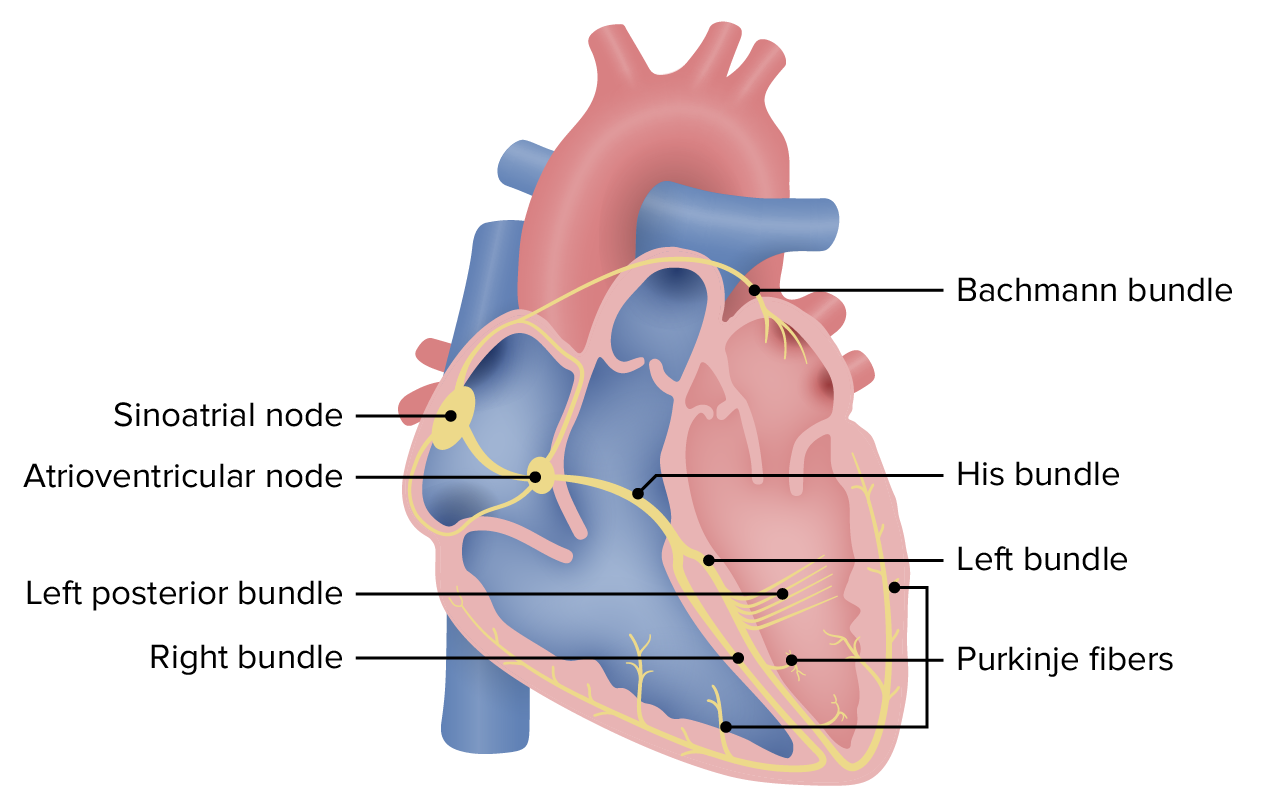
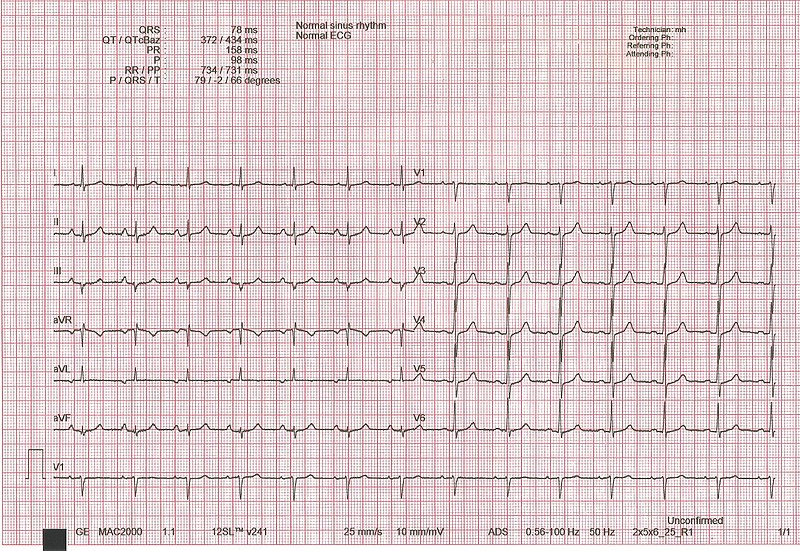
Download Lecture Overview
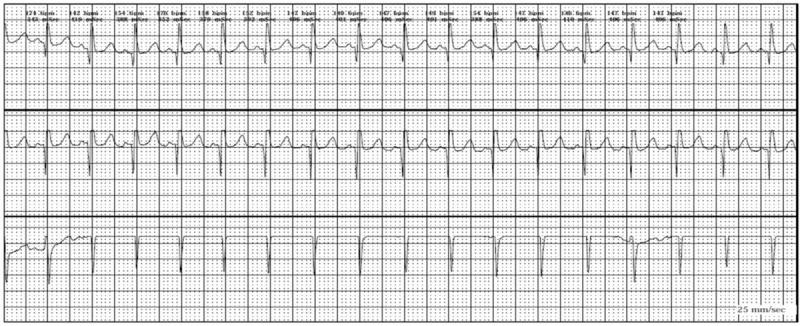
00:01 Forms of arrhythmia or causes of arrhythmia. 00:03 You can have acquired arrhythmias which are probably the most common, or you may have heritable genetic forms. 00:11 Let's deal first with the acquired forms. 00:13 An ischemic injury probably constitutes the vast majority of acquired arrhythmia propensity. 00:19 So you can have direct damage to any element of the conduction system from the AV node all the way down into the Purkinje fibers, and that may be a source of arrhythmia. 00:31 A damaged SA node will give you a sick sinus syndrome. 00:35 These patients tend not to be firing at the sinoatrial node or only intermittently, so that they don't have the normal kind of normal heart rates of 60 or 100 beats per minute. 00:46 In fact, because the SA node is not firing, the AV node says, 'I'll take over'. 00:52 And when the AV no takes over, it has a much slower depolarization rate. 00:57 And so it has, tends to have a relative bradycardia, a so-called junctional bradycardia. 01:05 So that's damaged SA node. 01:07 The AV node will take over as the pacemaker, and you have typically, bradycardia. 01:12 With atrial dilation, and atrial dilation is the major cause of atrial fibrillation, you are stretching those internodal fibers, so they fire either intermittently or fire aberrantly. 01:26 They become irritable, if you will. 01:28 So they can fire sporadically and you can have completely independent polarizations since they're not being entrained by the activity of the sinoatrial node. 01:40 This leads to irregular conduction through the AV node, as we've already talked about. 01:45 So depending on whether the signals reaching the AV node arrive during a a period that will allow them to be passed through or whether they arrive in a relative refractory period, you may or may not have signal conduction through the AV node into the bundle of His, etc. 02:05 So atrial fibrillation will be an irregularly irregular heartbeat, as we've already talked about. 02:14 We can have direct damage to any component of the conduction pathway - AV node, sinoatrial node, the right and left bundle branches, et cetera. 02:27 Let's look at a normal electrocardiogram. 02:30 And I know elsewhere within the entire collection of the Lecturio slide sets, there is a greater and more intense discussion of what the normal electrocardiogram or ECG looks like and how to interpret abnormal electrocardiograms. 02:47 For purposes of arrhythmia, though, we're just going to briefly look at them here. 02:51 So there is a p wave that marches through that represents atrial contraction, and we've marked the first three p waves, little tiny wave, not much myocardium, and we can see that depolarization. 03:05 And then we have a QRS ventricular contraction wave. 03:10 So after the atrial contraction, there's a pause and then the ventricle squeezes. 03:14 Now it's a much bigger spike because there's more myocardium that's firing all at once. 03:20 That's the QRS ventricular contraction wave depolarization. 03:24 Then we have a segment called the S to T segment that is involved with ventricular repolarization. 03:31 So the myocytes are coming back, they are pumping calcium appropriately and they're getting ready for the next wave. 03:38 And so there are certain intervals that occur between the P wave and the QRS complex, the QRS complex and the T wave. 03:46 And those are going to be important when we're thinking about certain forms of arrhythmia. 03:52 So the PR interval is normally 0.12 to 0.20 seconds. 03:57 Depending on disease that may be occurring in the AV node, that may be longer. 04:02 So you can you can have a prolonged PR interval. 04:06 And sometimes as we'll talk about, you can have the AV node so sick or deranged usually due to ischemia that it kind of intermittently or completely ignores that signal coming from the atria. 04:20 And then you can have PR intervals or p waves that kind of march along totally unlinked to any QRS activity. 04:31 The QRS complex is usually nice and sharp. 04:34 So this is reflecting the rather quick propagation of signal from the AV node down through the right and left bundle branches and into the Purkinje fibers and then out to the rest of the myocardium. 04:48 The ST segment is indicated 0.05 to 0.15 seconds and that's our main interval into our T wave, our repolarization interval. 05:01 Okay, so the dysfunctional AV node will give us varying degrees of heart block. 05:10 What is being indicated here on the on the right hand side, you see a little thin fiber, that's one of the internodal fibers bringing signal from the sinoatrial node to the AV node. 05:21 In a normal circumstance, it pauses and then it continues. 05:24 It pauses and then you get a signal propagation and then you see the QRS complex. 05:30 Okay, now we can have a first degree heart block where that AV node takes longer to process a signal and transmit it out through the bundle of His and into the right and left bundle branches. 05:45 And that prolonged PR interval is indicative of AV nodal dysfunction. 05:51 By itself, not a huge problem, but it does portend that you could progress to second and third degree heart block, so what are those? In second degree heart block, the signal comes in through the AV node and it is intermittently transmitted. 06:07 So maybe 1 out of 3 times, or 1 out of 2 times that the signal comes into the AV node, the AV node will pass it along, and at other times it completely ignores the signal. 06:18 So that is, worsening degree of AV nodal dysfunction. 06:22 That's kind of a bad thing, and then it portends getting into third degree heart block, which is a complete failure of the signal to propagate. 06:32 The SA is doing its thing, it's sending the signal along and the AV node is totally blocking it. 06:39 Now the AV node or ventricular myocardium, a little bit downstream of that, may take over so they will depolarize at their rate, just not at the same rate faster rate of the sinoatrial node. 06:51 So you will have a junctional escape rhythm that happens when there's a third degree heart block, but it may be at a very, very slow rate. 07:00 It may be 20 or 30 beats per minute, which may not be sufficient to provide adequate perfusion for a particular individual. 07:10 It's also important to note, once we get the signal out through the Purkinje fibers into the individual myocytes, and then the signal from there is cell to cell to cell all the way back up. 07:21 And the normal structure and distribution of gap junctions indicated here is the little blue rectangles, allows the movement of calcium currents from one cell that's been stimulated into the next cell, which will bring it to threshold and it will fire and send calcium to the next cell, to the next cell, etc. so that we get a nice wave of contraction through these calcium channels through the gap junctions that also allow passage of calcium. 07:47 So that's important. 07:48 If you have unhealthy myocardium, if you have ischemic cardiomyopathy for example, then we will tend to get abnormal distribution and spatial rearrangement of those gap junctions and you may not get a good, orderly propagation. 08:11 So the cell to cell conduction of a calcium current through the gap junctions is also very important for the final step of getting a coordinated contractile wave from apex to base in the ventricles. 08:25 So acquired forms of arrhythmia include ischemia, myocyte hypertrophy. 08:30 Myocyte hypertrophy will make cells much larger. 08:33 We don't change the capillary density, so the middle of these very large cells can be relatively ischemic. 08:39 They may lack sufficient ATP to pump ions appropriately. 08:42 You may have abnormal levels of calcium or other ions, and that may cause arrhythmias in a hypertrophied myocyte. 08:50 Inflammation, such as myocarditis or sarcoidosis, can also cause arrhythmias. 08:56 In some cases by killing myocytes, but in other areas by causing areas of fibrosis. 09:03 So all of these changes, ischemia, myocyte hypertrophy, inflammation can cause an increased irritability, a propensity of the individual cardiac myocytes somewhere along the pathway to fire when it feels like it aberrantly, and that can cause arrhythmias. 09:21 So you can get a cell., normally, as the propagation wave from cell to cell to cell through the gap junctions progresses as the cell is brought to threshold and fires, and then relaxes, there is a period when it cannot fire again, a relative refractory period. 09:38 If you have increased irritability, it is possible that we have cells that are returning back just to a cell as it's coming out of the relative refractory period and it will fire too soon. 09:53 And then we can develop waves of aberrant contraction and propagation, leading to an arrhythmia. 10:00 You can also have non-conducting material, amyloid or scar fibrosis from sarcoid or other previous ischemic injury. 10:09 And that will actually also cause the areas where we can have reentry circuits. 10:13 So if you are a myocyte and then you're connecting to the next myocyte and then to the next myocyte and then you encounter scar or you encounter amyloid, you have to go around and then you can potentially come back and develop reentry circuits. 10:28 So those will disrupt the normal signal propagation cell to cell to cell, leading to reentry circuits and an arrhythmia.
About the Lecture
The lecture Acquired Arrhythmia by Richard Mitchell, MD, PhD is from the course Arrhythmia.
Included Quiz Questions
What is the most common cause of rhythm disorders?
- Ischemic injury
- Channelopathy
- Electrolyte disturbance
- Congenital anomalies
- Anxiety
In a normal electrocardiogram (ECG), what does the P wave represent?
- Atrial depolarization
- Ventricular contraction
- Atrial repolarization
- Ventricular repolarization
- Hypokalemia
In a normal ECG, what does the QRS complex represent?
- Ventricular depolarization
- Atrial repolarization
- Ventricular repolarization
- Time from start of atrial depolarization to start of ventricular depolarization
- Hyperkalemia
Which of the following would be considered a normal time for the PR interval?
- 0.15 seconds
- 0.3 seconds
- 0.1 seconds
- 0.02 seconds
- 0.4 seconds
Which of the following is an acquired cause of arrhythmia?
- Myocyte hypertrophy
- Brugada syndrome
- Romano-Ward syndrome
- Jervell and Lange-Nielsen syndrome
- Catecholaminergic polymorphic ventricular tachycardia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |