Playlist
Show Playlist
Hide Playlist
Postoperative Care (Part 1)
-
Slides Post-operative care Special Surgery.pdf
-
Download Lecture Overview
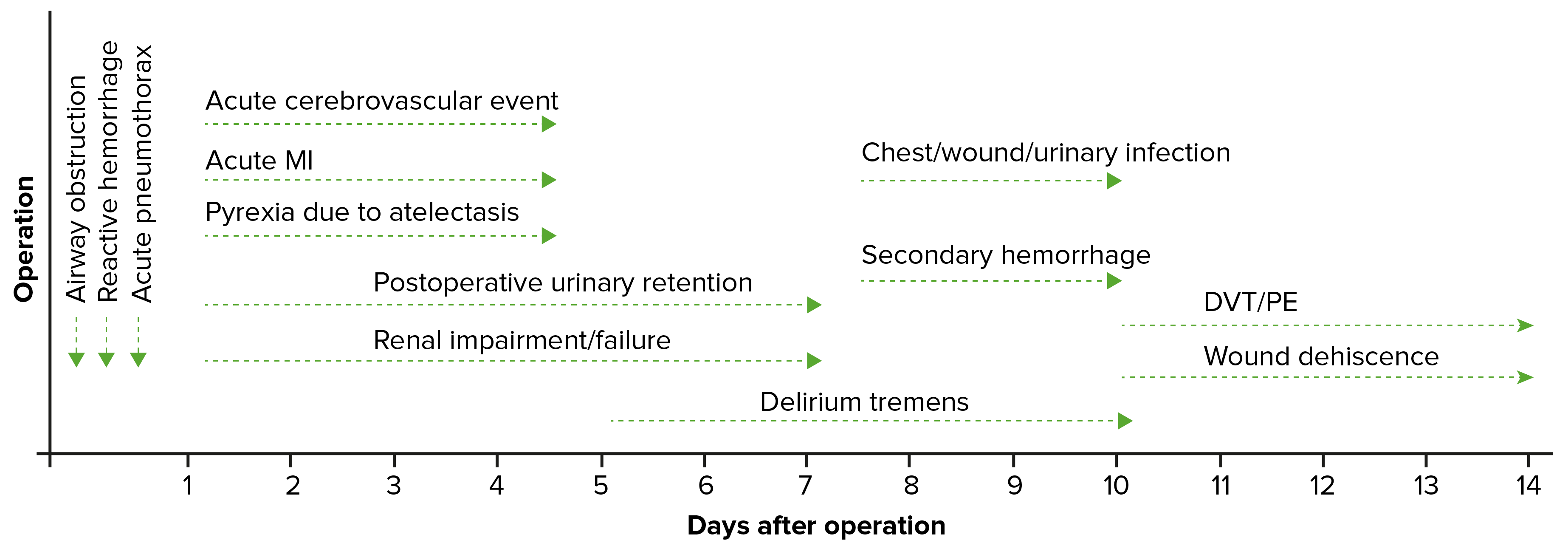
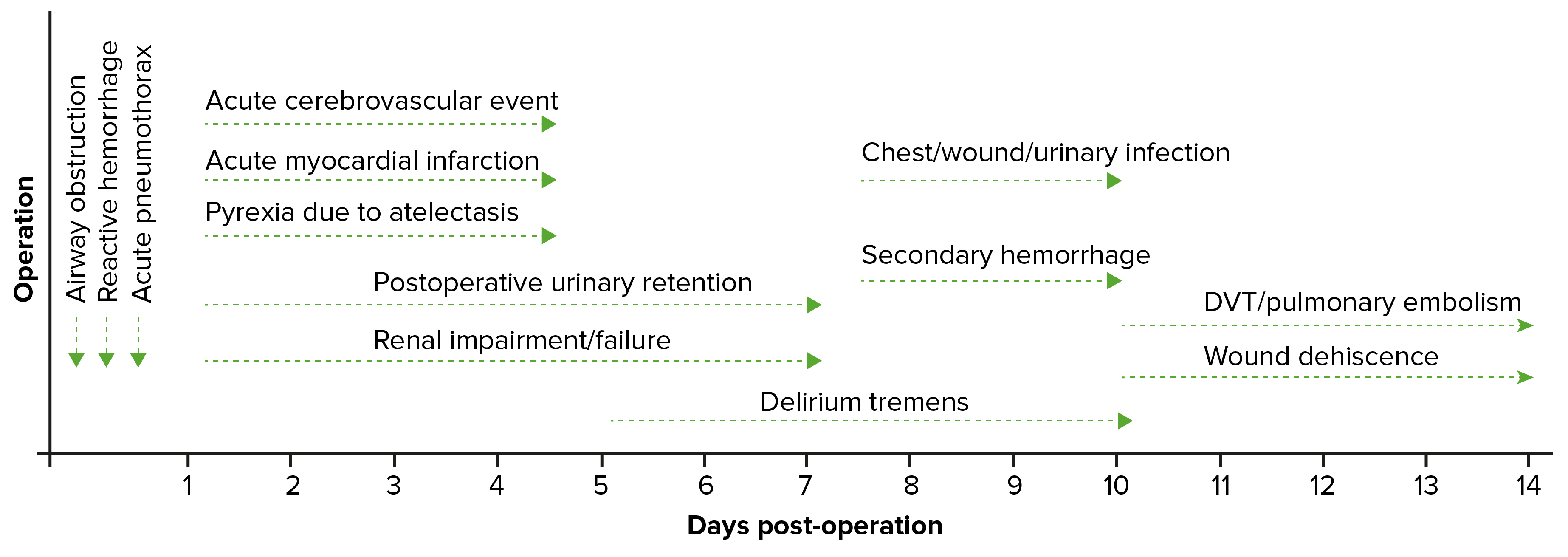
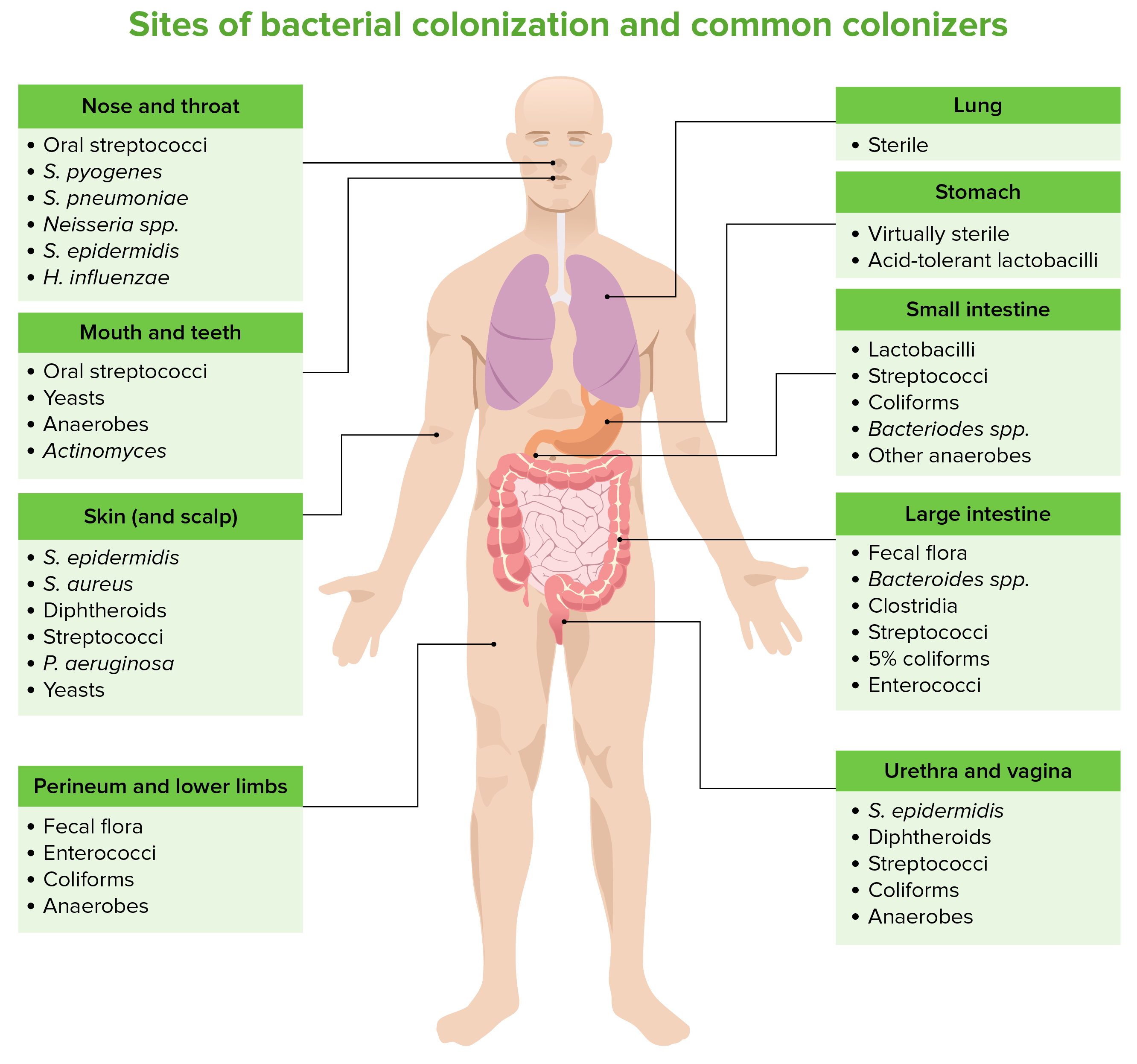
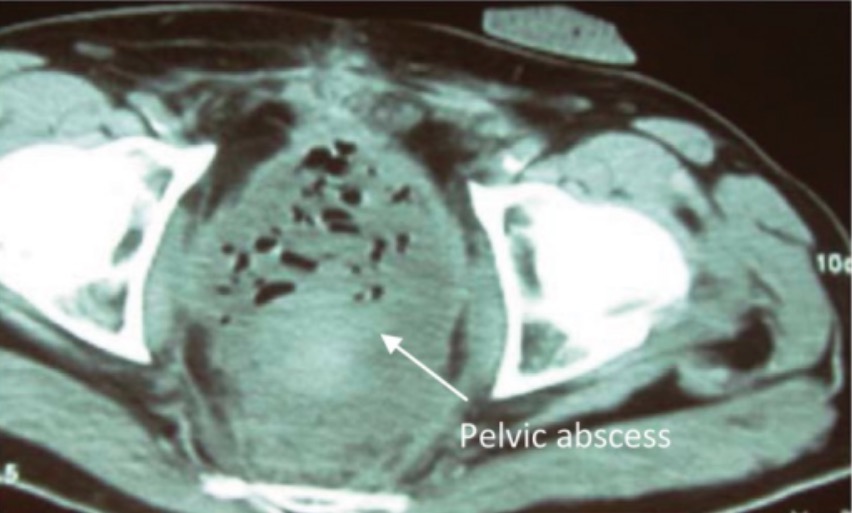
00:01 Welcome back. 00:02 Thanks for joining me on this discussion of postoperative care and some of the common problems that we may see in the postoperative period in this section of perioperative care. 00:15 Let's first visit tachycardia. 00:17 You know, when I was a resident, one of the things that we were always most afraid of is being called by the nurse to the bedside and told that your patient had a sinus tachycardia. 00:26 Why is that? I'll show in a second. 00:29 Look at this laundry list of potential differential diagnosis, all of which you have to rule out. 00:35 Pain is probably one of the most common postoperative or post-surgery causes of tachycardia. 00:41 But patients can actually be having a myocardial infarction or pulmonary embolism, hypovolemia, maybe an infection, anxiety, bleeding, hypoxia, withdrawal if the patient has history of alcohol, or they may be developing sepsis. 01:03 And when you look at this laundry list of problems, you can understand why we always get a little tachycardic when we get called to the bedside for evaluation of a patient’s sinus tachycardia. 01:15 Let's evaluate one of the causes of pulmonary embolism. 01:19 What are some risk factors for pulmonary embolism? First, any major surgery or any periods of immobility. 01:28 This is the perfect storm for surgical patients because they undergo major surgery. 01:32 And for a period of time, it may be painful due to incisions, in which case the patients become immobile. 01:39 How do we prevent DVTs and subsequent pulmonary embolism? Well, we give pharmacologic DVT prophylaxis in the setting of surgery. 01:49 Sometimes, we give the pharmacologic DVT prophylaxis before even making incision. 01:55 The choice of DVT prophylaxis is up to you and your institution. 01:59 There is some evidence that sequential compression devices may also help, although, by themselves, are not sufficient to prevent DVTs and subsequent pulmonary embolism. 02:12 Diagnosis of pulmonary embolism may be aided by giving an arterial blood gas. 02:16 In an arterial blood gas, generally, we demonstrate hypoxia, but very importantly hypocarbia. 02:24 That's because most patients with pulmonary embolism also hyperventilate, causing a reduction in the CO2. 02:33 How do we treat pulmonary embolism? Unfortunately, a lot of it is up to your own body to break down the clot. 02:39 Remember, the same clot process that allows us to stop bleeding also has a mechanism by which clots are broken down in an organized fashion. 02:47 We give systemic anticoagulation for two reasons. 02:51 Number one, to decrease the propagation of further clot, both in the legs and in the lungs. 02:57 And number two, to decrease inflammatory response. 03:02 Let's move on to a discussion of myocardial infarction in the postoperative period. 03:08 On the far left side of the screen, you see a normal EKG. 03:13 As highlighted by the green bars, you see various changes when a patient may have a myocardial infarction. 03:19 You can see hyperacute T waves and ST elevation. 03:22 And in the third quadrant, you see, when the ST elevation has improved, depending on when you actually capture the EKG. 03:27 and in the fourth quadrant you see that there are Q waves that developed, which is a later stage. 03:34 In patients who have had a myocardial infarction, there may actually be Q waves that persist even though the T waves have normalized. 03:41 Coupled with the troponin, this may be highly sensitive for a myocardial infarction. 03:47 What happens during a myocardial infarction is that the coronary vessels are not perfusing the heart enough with oxygen. 03:56 And our main goal of the preop workup is to predict and try to prevent a postoperative myocardial infarction. 04:03 Remember, patients who present with myocardial infarctions, particularly in the postoperative period, may have atypical symptoms. 04:12 And because the pain - because the patient may be experiencing pain elsewhere, it may be masked by other surgical pain. 04:22 Remember, getting EKG and a set of troponins, these are high-value, low-cost studies. 04:28 If the patient is determined to have a myocardial infarction, we initiate MONA therapy. 04:35 And we also start statins to reduce in-hospital mortality. 04:40 MONA stands for morphine, oxygen, nitroglycerin and aspirin. 04:47 Let’s move on to fevers as potential causes of tachycardia and fevers in general in the postoperative period. 04:55 If a clinical scenario is presented to you in the immediate postop period, within a few days of surgery, the most likely cause of fevers is atelectasis. 05:05 Patients can also develop pneumonias and urinary tract infections in the postop period. 05:12 DVTs is also a possibility, so are foreign objects. 05:17 Do you have a central line in? Is there a urinary catheter infection? Did you implant mesh during inguinal hernia repair? Did the orthopedic surgeon put any new hardware implants in joints? And lastly, but not - but not any less important is surgical site infections, particularly deep surgical site infections, such as intra-abdominal abscesses. 05:41 Intra-abdominal abscesses take time to form and typically no imaging study is usually useful until about postop day number four or five for intra-abdominal surgeries. 05:51 A word of caution, however. 05:52 Immediate surgical site infections can be of the necrotizing infection variety. 05:58 In these patients, there can be rapid deterioration if the surgical site infection is not recognized. 06:06 This is why we always teach our residents and students, look at the surgical wound. 06:10 It is potentially a common sight of postoperative fevers. 06:16 The timing of fever is also very important. 06:18 This can be remembered by using the mnemonic: Wind, Water, Walking Wound and Wonder drugs. 06:23 Wind is for atelectasis, at post-op day 1-2. 06:27 Water is for UTI at post operative days 3-5. 06:31 Walking is for DVT at post-operative days 4-6. 06:35 Wound is for the surgical site infection at POD 5-7 and more that 7 days think of drugs causing fever.
About the Lecture
The lecture Postoperative Care (Part 1) by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
An ABG of a post-operative patient presenting with pulmonary embolism is obtained. Which one of the following findings would you expect?
- Hypocapnia
- Decreased A-A gradient
- Hyperoxemia
- Respiratory acidosis
- Hypercapnia
An EKG is obtained in a post-operative patient showing an acute myocardial infarction. Which of the following findings would NOT be expected?
- Prolonged PR interval
- Q waves
- T wave inversion
- Hyperacute T waves
- ST elevation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good review and explanation of important topics! It helped me remember important stuff for my surgical clinical rotation.