Playlist
Show Playlist
Hide Playlist
Vascular Response to Acute Inflammation
-
Slides Acute and Chronic Inflammation Vascular changes.pdf
-
Download Lecture Overview
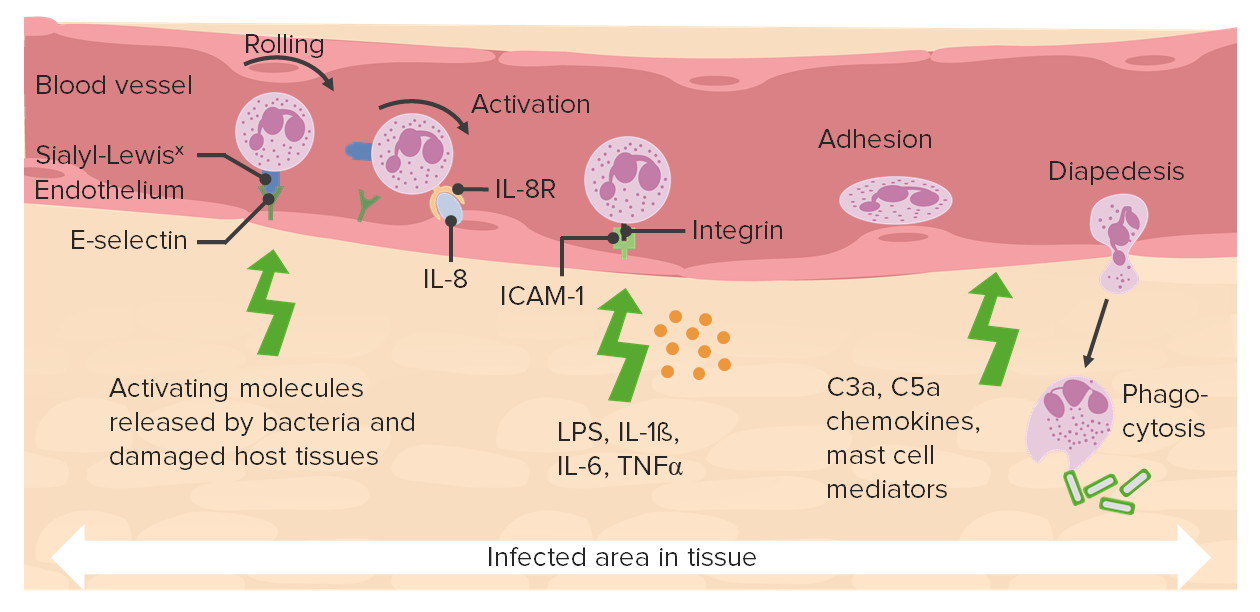
00:00 Welcome. 00:01 We're gonna charge right into the early stages of acute inflammation. 00:06 And before even neutrophils arrive, there are changes in vascular permeability, and vascular flow into the tissue. 00:17 That's going to set the stage for a lot of subsequent things. 00:19 But it's important that we understand the vascular changes that are happening. 00:24 So we have an acute inflammation, three components, three components. 00:28 First one here is the vascular response. 00:30 And that's what this particular topic discussion is about. 00:34 We will then transition to the cellular response, and how the cells the neutrophils get in. 00:42 And then we will finally get into the effector cascades, the mediators that gets secreted. 00:47 But for now we're going to focus on the vascular response. 00:49 And this is going to be part of the three of the cardinal features of inflammation. 00:56 This is going to be the calor, the increased warmth; the rubor, the increased redness; and the tumor, the increased swelling. 01:05 Keep in mind, as we go through all of this, there are lots and lots of details, tons of details. 01:10 Do not get too bogged down in the details. 01:15 Why am I even showing them to you then? Well, one, they're really important therapeutic targets. 01:21 And there are many things that you do for your own treatment when you sprain an ankle or something that are now therapeutic targets because we understand those details. 01:34 But it's also, they're just intrinsically interesting. 01:37 So, but see the big picture, really see and feel the force. 01:43 And don't get too bogged down in whether Darth Vader is your father. 01:48 All right. First up, the vascular response. 01:51 So this is going to increase blood flow, it's going to be increased permeability, and it's going to mediate inflammatory cell recruitment. 01:59 Okay, so that's why we have the initial vascular response. 02:02 And this happens incredibly quickly. 02:05 If I were to bang my hand, right now, within a couple seconds, I would be getting to see the edema. 02:11 And in a couple more minutes, it might get red. 02:14 And it might even get a little bit painful. All right. 02:18 So this vasodilation, why does it happen? Well, I mean, why is it important that it happens? It increases the blood flow into the tissue and allows us to deliver cells and mediators into the tissue. 02:31 So, I'm showing you on the right hand side, this happens to be a preparation from a rabbit ear. 02:37 The central blue stripe is elastic cartilage. 02:41 The glands that you can see top and bottom are little sebaceous glands that are associated with the rabbit hair. 02:50 And we're going to in a minute, add an inflammatory stimulus that will cause the vascular changes, and you'll see how dramatic it can be. 02:57 So that's why the picture is there. 03:00 The vascular changes besides vasodilation, increased size of the vessel going into the tissue, to increase blood flow. 03:07 There is also increased permeability. 03:09 This happens predominantly at the level not of the arterioles, the permeability, or at the capillaries, but rather the post-capillary venules. 03:18 So the veins that are on the other side of the capillary bed, and that's where the permeability is going to occur. 03:25 By having this increased permeability, we're losing fluid into the extravascular space, that slows the blood flow, right? Because all of that extra water is gone. 03:36 So the blood flow slows, and that allows cells that were previously zipping along... 03:41 white blood cells that are previously zipping along in the middle of the bloodstream to tumble out and start rolling over the surface of the endothelium. 03:49 So that increased permeability is going to be important for recruiting inflammatory cells, but it's also going to allow the deposition of circulating mediators. 03:58 Okay. 03:59 And here's what happened to this poor rabbit ear. 04:01 So the the dark blue pink stripe at the bottom this is a slightly different magnification. 04:07 So we can get all on the same screen, that blue little purple stripe, that's that same thickness of elastic cartilage in the rabbit ear. 04:14 And on one side, we have rubbed inflammatory stimulus, we have had increased vascular permeability, and increased vasodilation. 04:23 You see some big blood vessels there that weren't previously apparent, and that is the early vascular response. 04:29 So this would be red, it would be hot, and it would be a edematus. 04:34 So, we'd have rubor, calor, and tumor. 04:37 And I'm sure the poor rabbit had some pain too. 04:39 I'm sorry about that. 04:40 I didn't do it. 04:41 Okay. So in the vascular bed, how is this happening? How are we getting increased blood flow in the vascular bed? And it happens at the level of the arteriole coming into the capillaries. 04:53 So we just drawn kind of a schematic here of an arteriole and then a capillary bed and then a post-capillary venule. 04:59 At the bottom, you see the arrow, the red arrow going up, that's hydrostatic pressure. 05:04 So that's how much force is exerted, because of the pressure within the vessel, the blood pressure, and the green arrow going in reflects the colloid osmotic pressure. 05:14 So that's the effects of albumin and other proteins in the bloodstream, and to push in, or to suck in water. 05:21 So we have hydrostatic pressure pushing water out, and we have colloid osmotic pressure bringing water back in. 05:28 And at the arteriole or side, the pressure winds. 05:31 So you have a net flow of fluid water for the most part, but some electrolyte into the extravascular space. 05:39 In the capillary bed, it's balanced. 05:43 And then on the other side, that's very low pressure. 05:46 We now have the colloid forces, colloid pressure, greater than the hydrostatic pressure, and we have a net inflow of water. 05:55 So across a capillary bed, we have a balance. 05:59 And in most tissues, you don't have any excess edema. 06:02 That changes in the inflammatory settings. 06:06 So that's just setting the stage. 06:08 So now, if we increase arteriolar diameter, now, by increasing kind of flow into the tissue, we have a net flow on the front end that's much greater, because we've increased the dilation and the amount of blood that's getting in there and pressure. 06:25 And we haven't changed the colloid pressure at all. 06:27 So we have a net flow of fluid out because of that dilation. 06:32 And then in the capillary bed, in fact, all those vessels are also dilated, so there's increased hydrostatic pressure across the capillary bed. 06:38 And it even continues into the post capillary venules. 06:43 So that poor colloid osmotic pressure is not able to balance that and we have a net flow of water and electrolyte out into the tissues. 06:52 That's happening just because of increased hydrostatic pressure, squeezing the water across. 06:59 So how is this proximal dilation of the smooth muscle arterioles happening? It's happening through a couple different mediators. 07:07 One is histamine. 07:09 So remember, the mast cells? The poor cell that doesn't get any credit? Well, in fact, one of the things that releases when it's triggered, is histamine. 07:17 And that histamine will cause relaxation of the smooth muscle in that proximal arteriole allowing increased blood flow. 07:25 So that happens through mast cell degranulation. 07:27 It also happens through nitric oxide. 07:29 So nitric oxide is synthesized by endothelium and inflammatory cells. 07:33 So other cells that are part of the equation, and that will also cause vasodilation. 07:39 And there are some other mediators but histamine and nitric oxide are probably the most important ones for you to remember. 07:45 That causes smooth muscle relaxation, increasing blood flow into a capillary bed. 07:49 It also happens that some of the mediators produced by inflammatory cells also drive this process. 07:56 So beyond the nitric oxide, beyond the histamine, we have something called eicosanoids. 08:02 And we will come back to this. We will belabor this point a bit because the eicosanoids are very important. 08:08 They come in several different flavors, prostaglandins and leukotrienes. 08:13 But they also cause relaxation of the smooth muscle in the arteriole allowing increased inflow. 08:20 And those eicosanoids. 08:22 They're made by inflammatory cells, but they're made by every other cell in the mix, including smooth muscle cell, including the mast cell, including macrophages, including endothelial cells. 08:32 So those are important inflammatory mediators. 08:34 And we'll pay attention to those because we have good drugs that block the activation of eicosanoids. 08:42 Believe me, we'll come back to this.
About the Lecture
The lecture Vascular Response to Acute Inflammation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Which of the cardinal signs of inflammation is caused by vascular changes?
- Swelling
- Loss of function
- Pain
- Cyanosis
- Numbness
The increase in permeability during inflammation predominantly occurs at...?
- ...the venules.
- ...the arterioles.
- ...the capillaries.
- ...the arteries.
- ...the veins.
Which of the following cell types secretes histamine?
- Mast cells
- Macrophages
- Monocytes
- Endothelial cells
- Eosinophils
What is the purpose of vasodilation during inflammation?
- Delivery of cells and mediators
- Thermoregulation
- Restriction of the microbial pathogens
- Delivery of oxygen and nutrients
- Alleviation of pain
Increasing the blood flow into the capillary bed will lead to...?
- ...net flow of water and electrolytes into the interstitium.
- ...reducing the hydrostatic pressure in the arterioles.
- ...increasing the oncotic pressure in the venules.
- ...net flow of water and electrolytes into the vessels.
- ...equaling the hydrostatic and oncotic pressures in the capillaries.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |