Playlist
Show Playlist
Hide Playlist
Transudates vs. Exudates
-
Slides 09 PleuralDiseases RespiratoryAdvanced.pdf
-
Download Lecture Overview
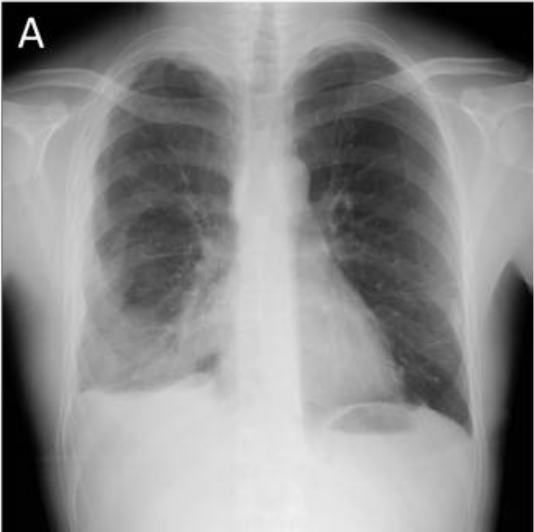
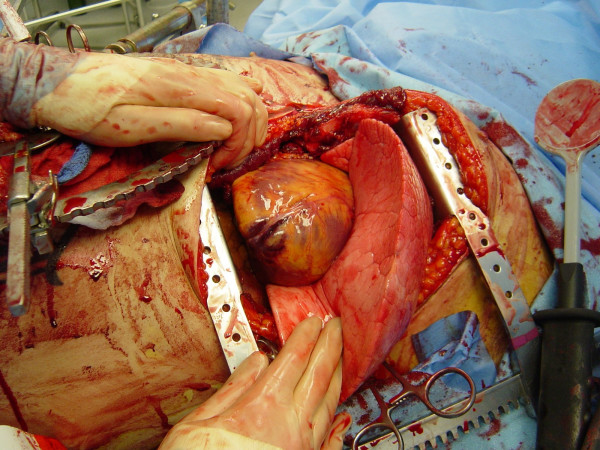
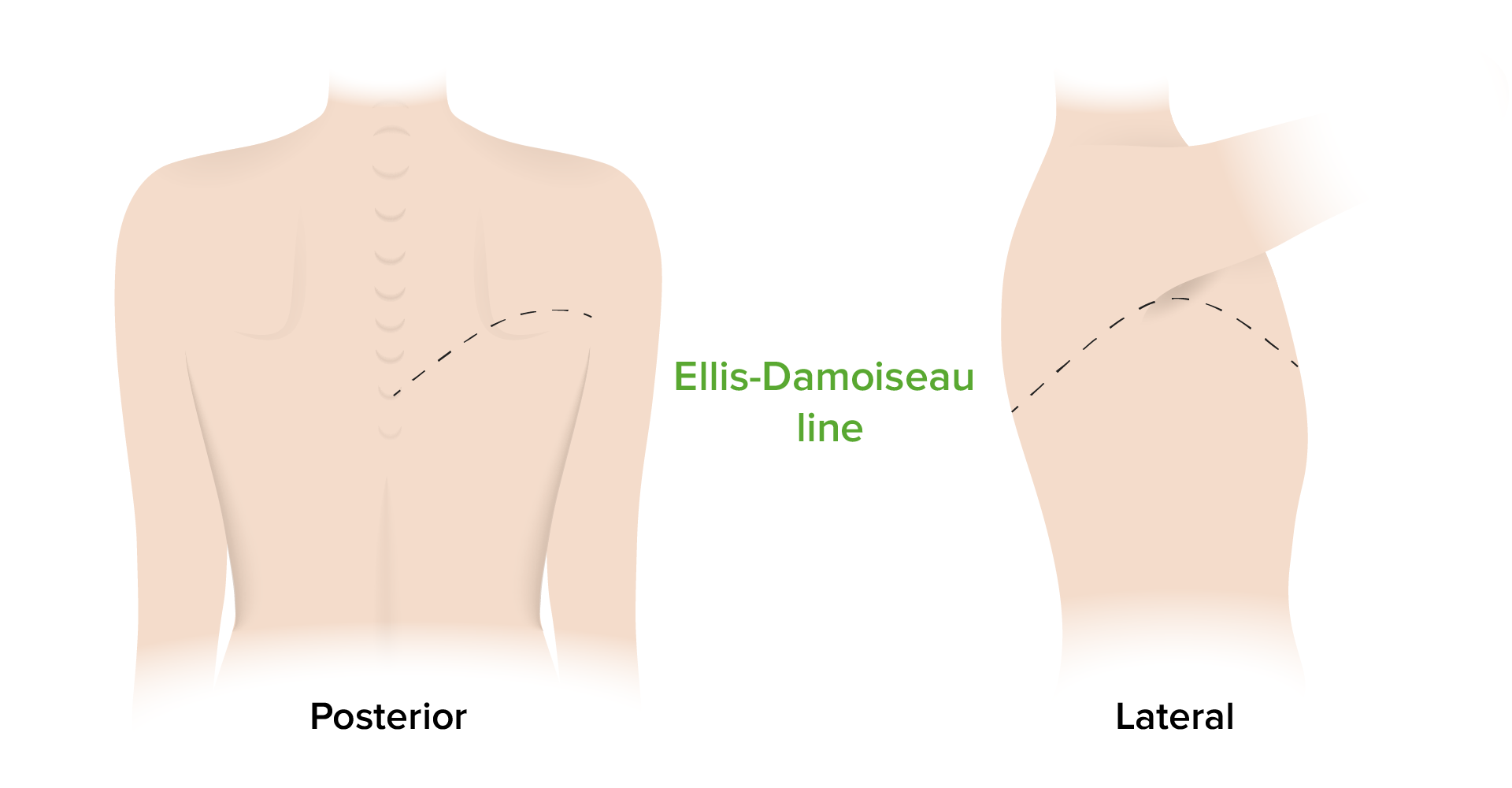
00:00 The big question with pleural fluid is whether the patient has a transudate or an exudate. Now, the difference is that in a transudate, the pleura is normal, and what you’re getting is excessive formation of pleural fluid by a passive transfer across from the blood. So this occurs with increased venous pressure such as heart failure or a low oncotic pressure of the blood such as decreased blood protein content. These may be bilateral but can be unilateral, and it can be associated with peripheral oedema because the same mechanisms would cause pleural fluid in these patients will also be caused of peripheral oedema. Exudates, in contrast, the pleura is the abnormality. The problem is that the pleura is abnormal and driving fluid formation. And that occurs with tumour of the pleura, inflammation of the pleura, or an infection. And these tend to be unilateral and won’t have associated peripheral oedema because this is a specific pleura abnormality. So, what are the causes of pleural effusions? Well, with transudates, you can have an increased venous pressure and that might be due to cardiac failure, mainly right side of cardiac failure, but also left side of cardiac failure. 01:13 It could be fluid overload. If somebody has got renal failure and they have an excess amount of fluid in the system, then you may get pleural fluid forming. And pericardial disease also causes pleural effusion. It’s often forgotten as a cause of this. 01:30 The protein content of the blood is required for retaining fluid within the blood. 01:36 And that with a low albumin content, you end up with the fluid seeping out into the pleural space, into ascites, and into the peripheral oedema as well. So patients with very low protein content of the blood will present with pleural effusions. These include liver cirrhosis, nephrotic syndrome, and very rarely, protein losing gut enteropathies or malabsorbtion. 01:54 But the commonest cause there would probably be the renal and the liver problems. 01:59 Exudates, in contrast, are due to abnormalities of the pleura as I mentioned before. So these occur in tumours, and usually, there’s a secondary pleural metastases, either from a lung cancer, from a breast cancer, or from a GI tract malignancies. Those are the common causes, but in fact, multiple different types of cancers can spread to the pleura to cause pleural effusions. And the presence of a pleural effusion with somebody with no malignancy is very suggestive. They’re going to have metastatic disease affecting the pleura. 02:28 Then again, there are primary pleural cancers as well. Actually, these are very rare in general apart from mesothelioma which is a primary cancer of the pleura that is associated with asbestos exposure that I’ve discussed in the lung oncology lecture. There are other causes of exudate pleural effusions. These basically involve pleural inflammation. 02:50 Probably the common cause might be a pulmonary embolus where you often get small effusions formed with that. But then there are connective tissue diseases. Rheumatoid arthritis, for example, will often have patients with pleural effusions, and systemic lupus erythematosus is another cause of inflammatory pleural effusions. Benign asbestos effusions occur in people who have been exposed to asbestos where the asbestos has inflamed the pleura and caused an exudated pleural effusion but hasn’t gone on to cause a mesothelioma. Occasionally, drugs can cause pleural effusions. And then actually, many exudate pleural effusions we cannot identify the cause and can’t characterize as idiopathic. 03:28 The last major category of exudated pleural effusions is those due to infection. 03:33 It’s an incredibly important category, and these occur in three main circumstances. One is a para pneumonic effusion which in effusion is associated with pneumonia. The second is the empyema which is a pleural infection without associated pneumonia. And the third very important is tuberculosis. There are a whole range of very rare causes of pleural effusions needing chylothorax, we have chyle forming in the pleural space, ovarian tumours, or Meig’s syndrome. Pancreatitis can cause inflammation of the pleura, and of course, trauma itself can cause the leaking of blood into the pleura and that’s called haemothorax. But those are all, in general, relatively rare or obvious diagnosis. 04:14 So, how would you investigate somebody with a pleural effusion? Well, first off, you need to confirm there’s a pleural effusion by doing a chest X-ray, and a pleural ultrasound will be also very helpful indeed. This is an ultrasound picture showing that they clearly are very black area which is the fluid with a lung separated from the chest wall by that black area. If somebody has bilateral pleural effusions, then they are likely to be transudated just because they’re bilateral. So if somebody has bilateral effusions, there’s an obvious cause for transudate, such as known heart failure or low albumin due to nephrotic syndrome. 04:48 Actually, you don’t need any further tests. The answer to why the patient has pleural effusions is there. It’s due to the cause of the transudates.
About the Lecture
The lecture Transudates vs. Exudates by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Pleural Disease.
Included Quiz Questions
Which of the following is TRUE regarding exudative pleural effusion?
- The cause is active inflammation of the pleura.
- The pleura is usually unaffected.
- The cause is decreased serum protein content.
- Peripheral edema is almost always present.
- The condition is usually bilateral.
Which of the following is LEAST likely to cause malignant pleural effusion?
- Astrocytoma
- Ductal breast carcinoma
- Small cell carcinoma
- Lymphoma
- Mesothelioma
Which of the following generally refers to a transudative pleural effusion?
- Hydrothorax
- Pyothorax
- Hemothorax
- Chylothorax
- Pneumothorax
Which of the following best describes Meigs syndrome?
- Benign ovarian tumor with ascites and pleural effusion
- Gastric carcinoma with pleural effusion
- Lung cancer and transudative pleural effusion
- Pleural effusion in a patient with preexisting ascites
- Pleural effusion following acute pancreatitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very clear explanation about transudates and exudates. Unfortunatelly, the subtitles in spanish are not very accurate.