Playlist
Show Playlist
Hide Playlist
Ventilation – Lung Physiology
-
Slides 02 LungPhysiology Basic.pdf
-
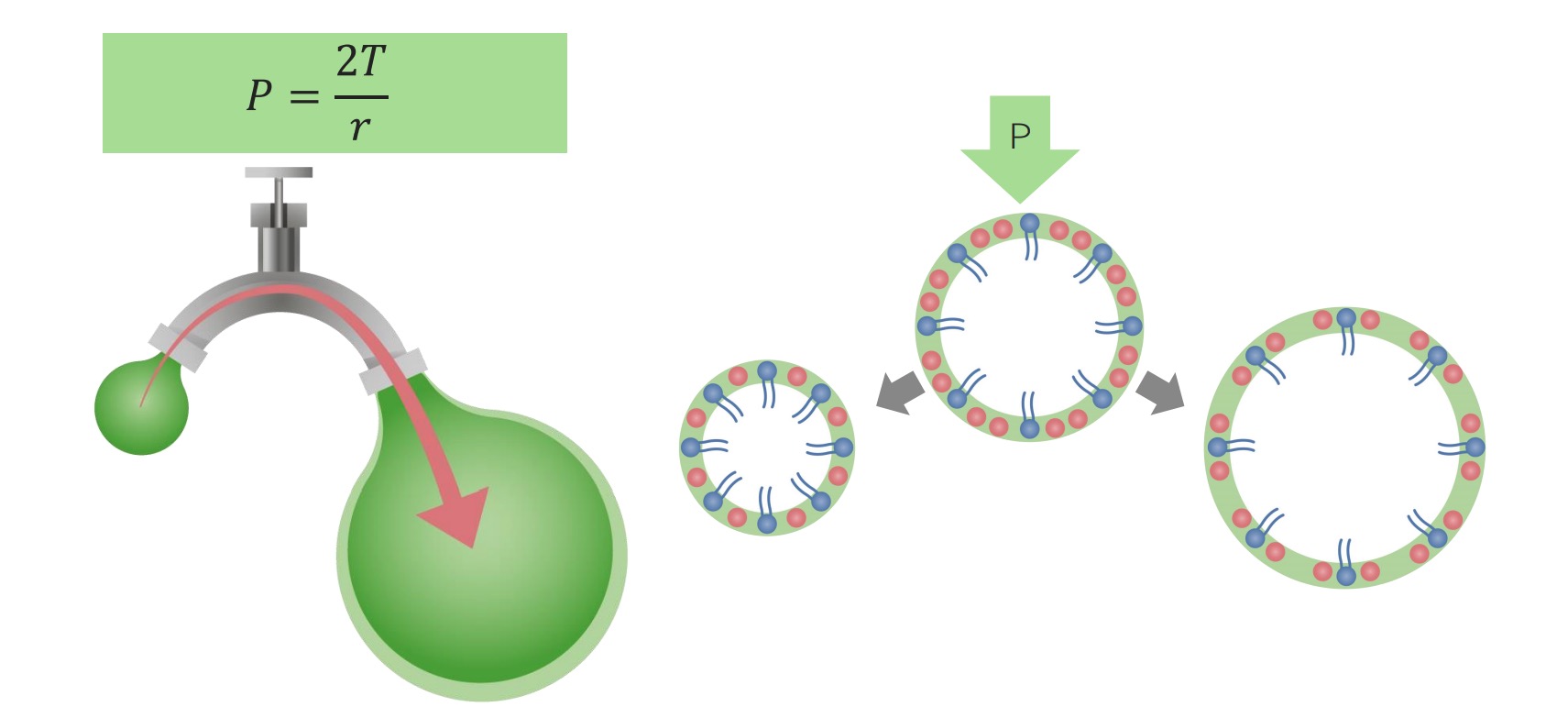
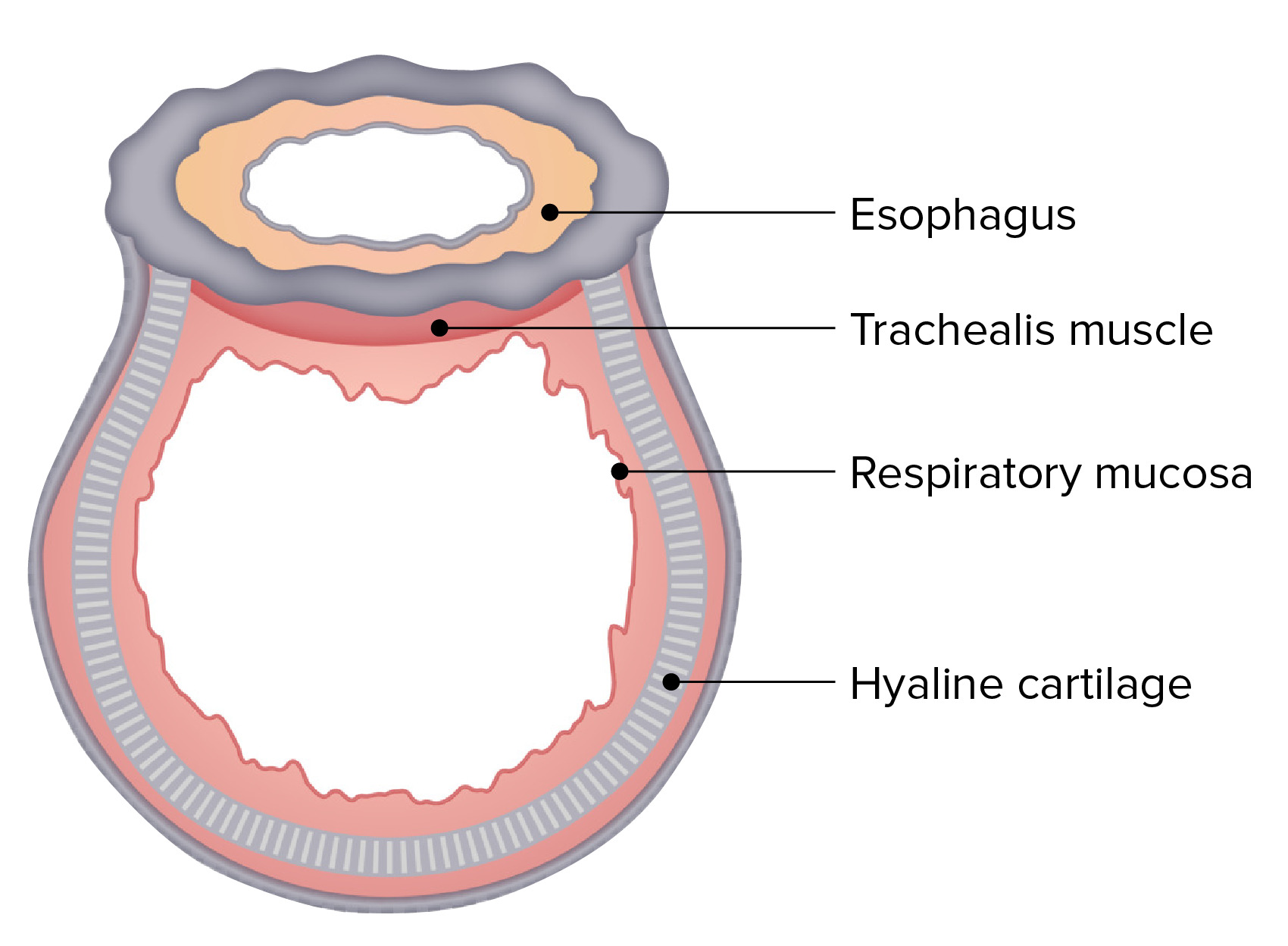
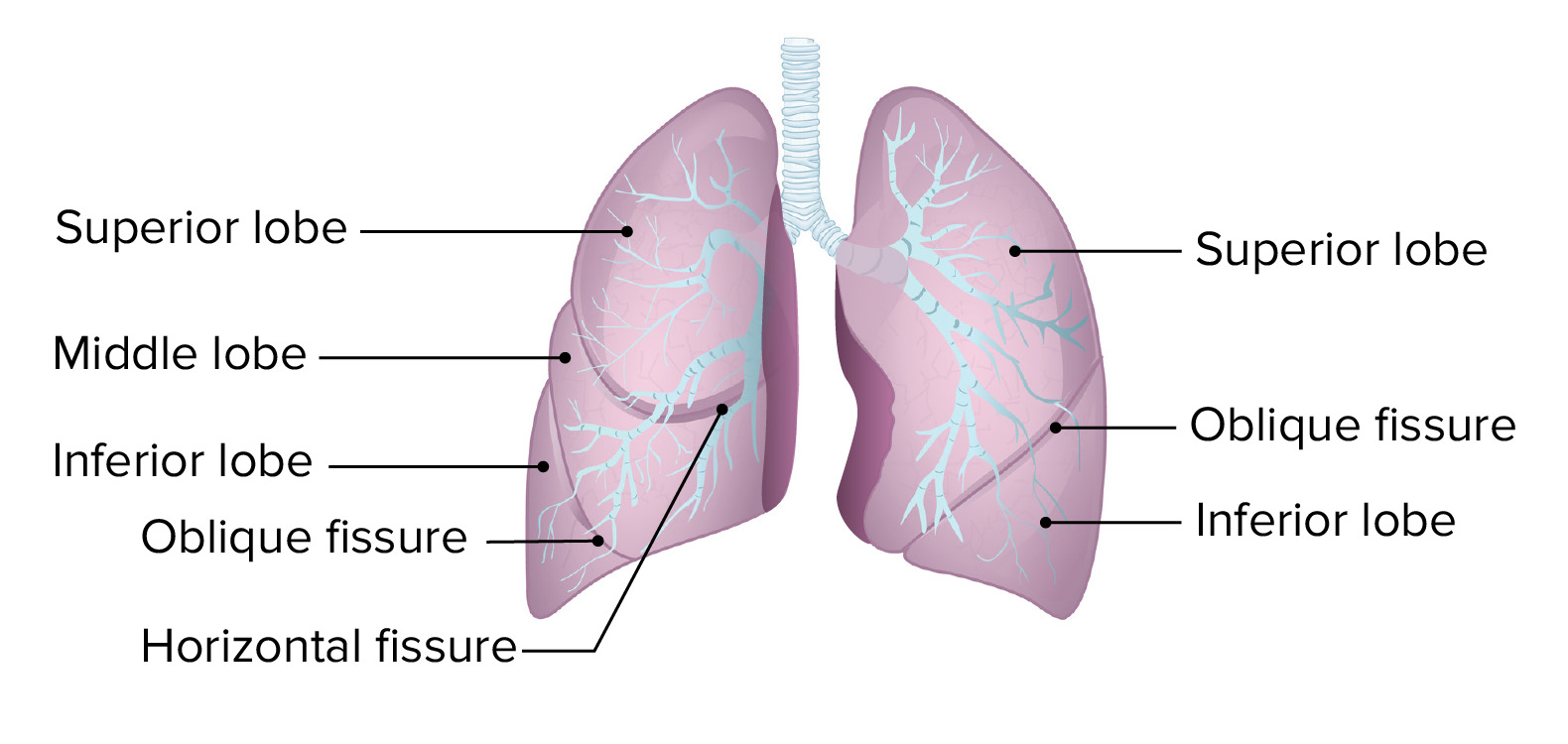
Download Lecture Overview
00:00 Ventilation, how does the air get into the alveoli? Well this largely depends on Boyle’s law. The volume of a gas is inversely proportion to the pressure of the gas, i.e. the gas of this volume, it's in a higher pressure than when it is at that volume. And that means that, if you do this there will be a negative pressure contained within that volume of gas compared to what it was previously. And that is the main driver for ventilation. So if you are going to describe inspiration what happens to that is that this is an active process even at rest. Your diaphragms will contract, that means they will flatten down, that will make the diameter, the top to the bottom length of the lung longer. The ribs will move up and out because the intercostals contract moving the ribs up and out. And that makes the diameter of the lungs in the horizontal dimension larger as well. The consequence of that is that, you have an increased size of the thoracic cavity. And because of the negative pressure in the pleural space the lungs will fill that thoracic cavity and the air inside the lungs will now be at a lower pressure because of Boyle’s Law than atmospheric pressure. And that drives air down through the airways, down through the upper airways, through the trachea and down the bronchi so it finally reaches the alveoli. 01:24 In fact, the movement of air in the terminal bronchioles and the alveoli is very small. 01:31 What actually happens is that the oxygen concentration in the alveoli increases on inspiration by diffusion of the oxygen-rich air that is now being delivered to terminal airways and vice versa for the carbon dioxide. The carbon dioxide diffuses from the alveoli into the terminal airways and then is breathed out. 01:51 So exhalation, expiration is a passive process unlike inspiration unless you are exercising. 01:57 What happens is that the diaphragms and intercostal muscles relax and the lungs because they are elastic they tend to contract inwards and in doing so, they would expel the air within the lungs by generating a positive pressure and that will flow out through the trachea and the bronchi. This is the diagram showing the changes in the skeleton and the diaphragmatic positions during inspiration and expiration. You can see on the left hand side the ribs are more horizontal, the diaphragm is flatter, and that increases the total height of the lung and the total diameter of the lung. And on expiration the reverse happens with the diaphragm relaxing and the intercostal relaxing and the lung returning to its normal resting shape. There are some issues in ventilation. And I am just going through a couple of those now. 02:43 The first is surface tension. So the alveoli have a thin layer of fluid and there is a degree of surface tension and that requires a certain amount of energy and effort to overcome to make the alveoli expand. Now that is actually reduced physiologically by production by alveolar type-2 immunocytes of a surfactant and this is a phospholipid substance which essentially acts a little bit like an oil-type substance that reduces the surface tension and therefore reduces the effort required during ventilation to expand an alveolus. 03:19 Another issue of ventilation is airways resistance. So as the air flows down the tracheobronchial tree, it flows past the mucosa of the tracheobronchial tree and that creates some form of resistance to the airflow. The intensity of that resistance, the strength of that resistance is proportional to the length of the airs flowing down and indirectly proportional to the fourth power of the radius of that airway. That means a small changes in the radius have quite profound effects in the airways resistance. And that is relevant for the airways disease such as COPD and asthma which affect the diameter of the bronchial tree and cause airways resistance to increase as a consequence. In the normal state, most airways resistance actually occurs in larger airways, the major bronchi. So there is a certain amount of muscular effort required to ventilate the lungs and that is called the work of breathing. And that is required to stretch the lungs, the pleura, and the chest wall, overcome the airways resistance we have just discussed and normally it is about 1% to 2% of the total body oxygen required, but if you have significant respiratory problems which may increase the airways resistance or might increase the chest wall and the lung compliance then that portion of the oxygen requirement will increase. Importantly, the work of breathing is lowest at the functional residual capacity that is the beginning of the total volume inspiration, the normal point when you start to inspire when you are at rest. So the work of breathing is increased if the lungs are hyperexpanded and that occurs in airways diseases where the lungs instead working at normal functional residual capacity, it will be working at a higher level of lung volume and that has negative consequences for the work of breathing. Increased airways resistance as we have already mentioned such as airways disease will also increase the work of breathing as will the problems affecting the chest wall, the pleura, also the alveoli interstitial lung disease, all affecting compliance and making the work of breathing higher. Right,
About the Lecture
The lecture Ventilation – Lung Physiology by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Introduction to the Respiratory System.
Included Quiz Questions
According to Boyle's Law, what is the relationship between the pressure of a gas and the volume of its container?
- Inversely proportional
- Directly proportional
- Exponential
- Linear
- Unpredictable
What occurs to the diaphragm when it contracts?
- It flattens.
- It elevates.
- It reverses its shape from convex to concave.
- It pulls the 9th and 10th ribs inwards.
Which of the following processes occurs during exhalation?
- Elastic recoil of the lungs causes them to retract.
- The lungs constrict, assisted by pleural negative pressure.
- The lungs inflate further because elasticity can only drive them to fill with air.
- The lungs stretch because, like a balloon, once inflated pulmonary parenchyma can't return to its original state.
- The lungs remain inflated because the lungs require energy to recoil.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |