Playlist
Show Playlist
Hide Playlist
Macrocytic Anemia: Introduction and Etiology
-
Slides Macrocytic Deficiency.pdf
-
Download Lecture Overview
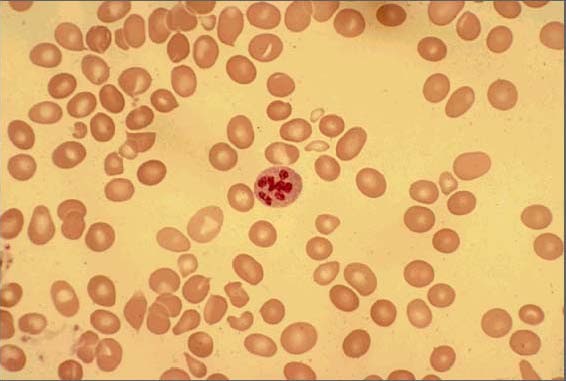
00:01 Macrocytic anemias, we’ll divide this into megaloblastic and non-megaloblastic. 00:06 For those of you that were unclear or unsure about the differences between megaloblastic and non-megaloblastic both being under macrocytic, well, we’ll be clarifying that in this lecture series. 00:17 Macrocytic anemias are most commonly caused by, well, some of the megaloblastic we’ll take a look at are B12 and folate. 00:24 These are the age old vitamins that you will be talking about and have been discussing in your medical education for years now. 00:33 So, we should be able to go through this rather quickly. 00:35 So, I will just reinforce those little biochemical facts that become really important for us. 00:41 We’ll take a look at B12 and folate deficiency. 00:43 Both of these are megaloblastic anemias. 00:47 Now, if it’s B12, we will take a look at this in number of DNA steps synthesis as is folate. 00:55 Now, what does that even mean and how can you then associate this with megaloblastic? So you need B12 and folate for proper DNA synthesis, both purines and pyrimidines, right? Especially that step that we'll be dealing with quite a bit. 01:09 We are trying to turn dUMP into dTMP. 01:13 And if you don’t B12 or folate, then you can’t produce proper DNA. 01:17 Where do you form RBCs? Bone marrow. 01:22 Is it only RBCs that you produce in bone marrow? That’s a stupid question, isn't it? So you’re going to form many, many, many cells, hematopoietic stem cells. 01:30 That’s what you have, they're pluripotent. 01:32 And you give rise to myeloid. 01:35 And by myeloid, we mean that referring to our megakaryocytes and platelets, referring to erythropoiesis and RBCs, and our granulocytes referring to our neutrophils, eosinophils and basophils. 01:46 Okay. What will happen if you didn’t have proper DNA synthesis and the bone marrow has been affected? Then you don't have proper maturation of your cells, do you? What’s this called when you don’t have proper formation of platelets, proper formation of RBCs nor your proper formation of your granulocytes? It’s called pancytopenia. 02:08 Fascinating, isn’t it? Now, if you have pancytopenia and you’re producing immature type of cells, especially RBCs, that’s what we are doing here, macrocytic, then you’re going to form this blasts. 02:19 What does a blast mean to you? It means it is an immature type of cell that’s inside my bone marrow. 02:24 Last time we had this discussion, ladies and gentlemen, was when we’re dealing with sideroblastic anemia and microcytic anemia. 02:30 And we were talking about the porphyria pathway Do you remember that? So here macrocytic, what are you looking at first and foremost? Interpretation of this, I’ll walk you through the history, not to worry. 02:42 But labs, you have an MCV greater than 100. 02:47 An MCV of greater than 100, that’s where we are right now. 02:51 In addition, you’ll end up forming or having pancytopenia and megaloblast.
About the Lecture
The lecture Macrocytic Anemia: Introduction and Etiology by Carlo Raj, MD is from the course Macrocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following conditions is most likely with significant deficiency of vitamin B12 or folate?
- Pancytopenia
- Increased DNA synthesis
- Leukocytosis
- Erythrocytosis
- Reduced number of blasts
Which of the following is NOT a feature of megaloblastic anemia?
- Increased erythropoiesis
- Reduced pyrimidine synthesis
- Reduced DNA synthesis
- Mean corpuscular volume > 100
- Pancytopenia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |