Playlist
Show Playlist
Hide Playlist
Hypoglycemia: Treatment
-
Emergency Medicine Bord Hypo and Hyperglycemia.pdf
-
Download Lecture Overview
00:01 So now that we’ve talked about what to do if the blood sugar is too high, we’re gonna take a few moments to talk about what to do if the blood sugar is too low. 00:10 So that’s a condition known as hypoglycemia. 00:12 Now why does hypoglycemia happen? It’s most common actually in diabetic patients and it’s most commonly related to tight glycemic control, an exogenous insulin. 00:23 So for patient who’s on insulin, potentially they didn’t eat as much that day or they missed a meal and then the blood sugar can get dangerously low. 00:33 Now here we start thinking about this when the glucose levels are less than 60. 00:37 Patients may also have increased energy output or exercise so for a patient who has decided to start an exercise regimen or decided to go on a race, that’s something that can also lead to hypoglycemia. 00:51 And lastly, it could be related to oral hypoglycemic agents. 00:56 So someone who had their medication dose increased, potentially your patient who has renal failure in the setting of taking a renally processed medication which means that medication dose is going to be present for longer that can also produce hypoglycemia. 01:16 So here are some key patients though, key patient populations for you to think about when we’re thinking about hypoglycemia. 01:23 When the blood sugar gets low our bodies respond by getting some tremors, potentially getting a little bit sweaty. 01:30 Some patients have what we call hypoglycemic unawareness. 01:34 Now this can be potentially a very dangerous situation because this is a patient who has a low blood sugar but doesn’t necessarily realize it and when the blood sugar gets too low, patients can get seizures, patients can go into a coma and this can be a life threatening condition. 01:50 Patients can die from hypoglycemia. 01:52 So hypoglycemic unawareness can be very dangerous especially for a diabetic patient. 01:58 You also wanna be weary of a patient with alcohol dependence or malnutrition. 02:02 The reason that you wanna be careful with those patients is because they don’t have good glucose stores. 02:08 So for all patients who come in intoxicated to the Emergency Department, especially with alcohol intoxication, one of the main things that I do for that patient is I check a finger stick because they’re gonna—by definition if they’re intoxicated, be a little bit altered. 02:23 I wanna make sure also that their blood sugar isn’t low. 02:28 So blood sugar less than 40 to 50 is when patients start to develop more symptoms and these symptoms are due to epinephrine release and central nervous system dysfunction. 02:39 So what a patient experience, they can be sweaty, they can be nervous or anxious, they may have a little bit of a tremor, the heart rate may be fast, in severe cases they may develop a seizure and eventually a coma. 02:54 Now one of the key medications that can cause severe and prolonged hypoglycemia are sulfonylureas, so this is a medication class. 03:05 The reason that they cause severe and prolonged hypoglycemia is because they stay in the body for longer periods of time. 03:12 Now hypoglycemia related to insulin or Metformin is often times short lived. 03:17 So the diagnosis here is really based on a low blood sugar. 03:23 Patients who present altered, who present confused, who present with a seizure, check a blood sugar. 03:30 This is not something that you wanna miss. 03:32 Now there is a condition of factitious hypoglycemia and what that basically means is that the patient did something to cause their blood sugars to be low. 03:41 For those patients, they may have normal or low levels of Peptide C and they may also have high levels of insulin. 03:50 So this is a patient who injected themselves with too much insulin on purpose. 03:54 What do we do for treatment? A key thing is you wanna give oral intake of sugar containing foods. 04:02 If the patient is more awake and alert, you can go ahead and give them some juice. 04:08 For patients who are more altered, there are glucose containing solutions and tablets that you can place underneath the tongue for absorption. 04:16 Ultimately, what you’re gonna wanna do as patients get better is you’re gonna wanna feed them regular food. 04:22 So we know that if you drink juice, your body processes the glucose, uses the glucose and that goes away very quickly. 04:28 It’s always a good idea for patients who are awake and alert a little bit down the line to eat like a sandwich, a turkey sandwich, something that’s gonna have a mix of protein and carbohydrates that’s gonna maintain the blood sugar for a longer period of time. 04:41 You can also give IV glucose solutions. 04:44 It comes in a variety of concentrations. 04:47 Generally, for an adult patient we give D50 which is 50% glucose containing solution. 04:52 It’s generally a pretty thick solution; it needs to be administered through the IV. 04:57 If a patient doesn’t have IV access and they’re altered and confused and not able to take anything orally, you can give intramuscular glucagon. 05:07 Like we talked about in the beginning of this lecture, what glucagon does is it goes to the liver and it causes release of glucose from the liver. 05:15 Now for more patients this will work fine, but for a patient who is malnourished or has a significant history of alcohol abuse, they might not have enough glucose stores in their liver for this to be effective. 05:27 The other thing that you can do is administer octreotide. 05:32 Octreotide limits insulin release and is a treatment of choice for sulfonylurea overdose. 05:39 So someone took too much of their sulfonylurea medication, octreotide is what you should reach for. 05:44 Now for disposition, many of these patients can be watched in the Emergency Department for a few hours. 05:51 If their blood sugar stays okay, they can go home and be safely discharged. 05:56 You wanna consider admitting patients for recurring hypoglycemia. 06:01 So if they’re in the Emergency Department and their blood sugar goes up to a normal range and then it’s checked an hour so later and it goes back down to being in a dangerously low range, that’s someone who you wanna start thinking about should they be admitted to the hospital to make sure that their blood sugar stays elevated. 06:18 Again, hypoglycemia related to long acting oral medications should also most likely be admitted to the hospital because that’s something that— potentially if you sent someone home their blood sugar gets dangerously low, that can have major and serious implications for the patient. 06:35 So in conclusion here, glucose metabolism is generally very regulated by our bodies, primarily by insulin and glucagon as the main hormones. 06:44 Hyperglycemia can be a manifestation of uncomplicated hyperglycemia, DKA or HHS and we’re gonna use our labs, our history, our physical examination to help distinguish between these three entities. 06:58 In patients with DKA and HHS, be sure to look for an underlying cause. 07:02 It’s often times presenting HHS and definitely sometimes present in DKA. 07:08 Don’t begin insulin treatment until the potassium level is resulted. 07:12 This is a very important point here. 07:15 Iatrogenically, we can make someone very—have very low potassium so don’t start that insulin treatment until the potassium level comes back. 07:23 And when it comes back, be sure to treat accordingly to what that level is. 07:26 Check a finger stick for patients who are altered. 07:29 Hypoglycemia is common in diabetic patients and malnourished patients and requires very prompt treatment.
About the Lecture
The lecture Hypoglycemia: Treatment by Sharon Bord, MD is from the course Endocrine and Electrolyte Emergencies. It contains the following chapters:
- Hypoglycemia
- Hypoglycemia Treatment
Included Quiz Questions
What class of oral hypoglycemic agents can cause prolonged and severe hypoglycemia?
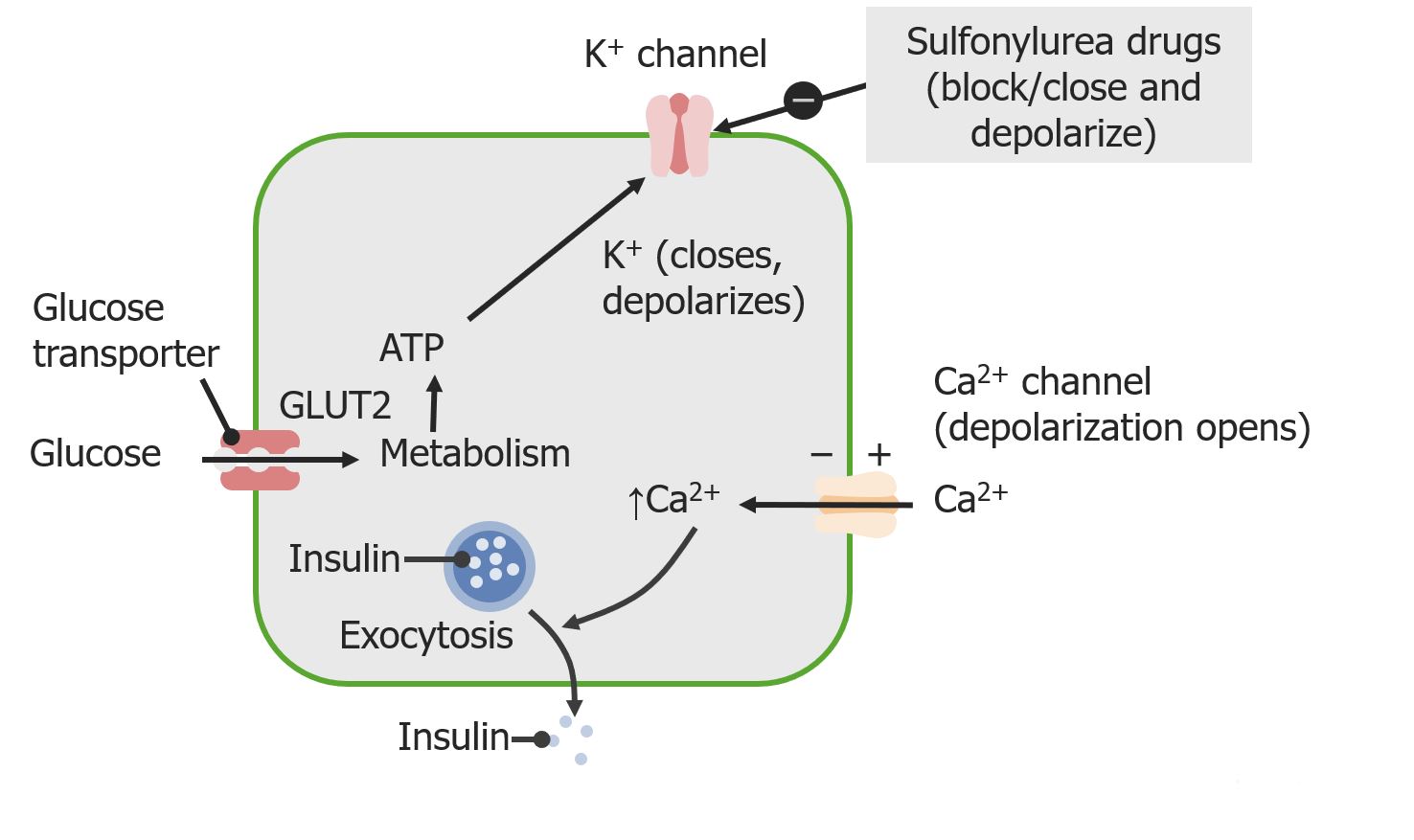
- Sulfonylureas
- Biguanides
- Alpha-glucosidase inhibitors
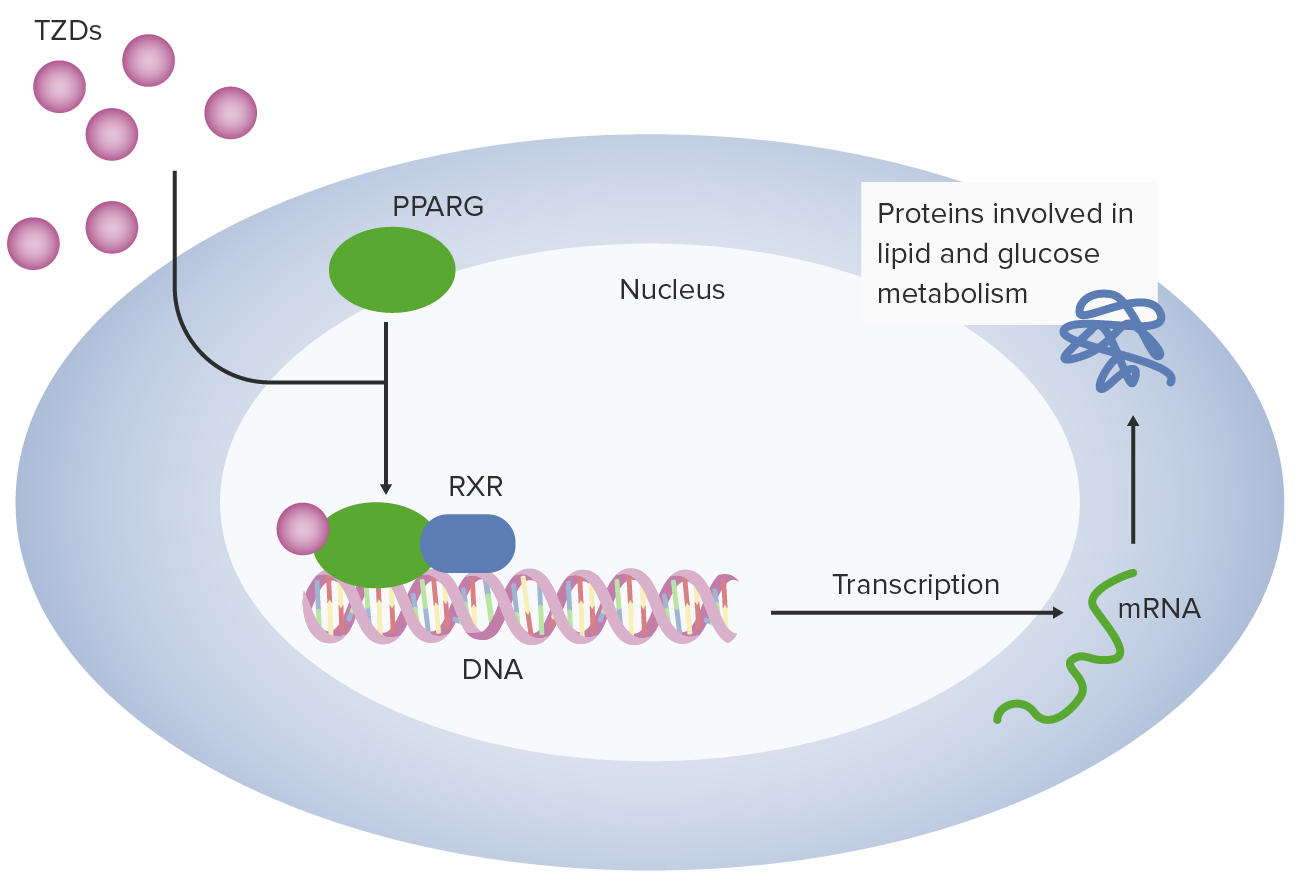
- Thiazolidinediones
- Dipeptidyl peptidase-4
What is the specific treatment for sulfonylurea overdose?
- Octreotide administration
- Pure glucose administered orally
- IV glucose administration
- Intramuscular glucagon
- Sublingual glucose tablet
What is the mechanism of action of octreotide in the management of hypoglycemia due to sulfonylureas?
- Limits insulin release
- Increases blood sugar level
- Limits glucagon release
- Promotes gluconeogenesis
- Increases glycogenolysis
Which of the following is NOT a cause of hypoglycemia?
- Small, frequent feedings
- Oral hypoglycemic agents
- Tight glycemic control
- Exogenous insulin
- Increased energy output
Which hormone release can cause the typical symptoms of hypoglycemia?
- Epinephrine
- Acetylcholine
- Cortisol
- Renin-angiotensin
- Vasopressin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |