Playlist
Show Playlist
Hide Playlist
Epididymitis (Emergency Medicine)
-
Emergency Medicine Bord Sexually Transmitted Diseases.pdf
-
Download Lecture Overview
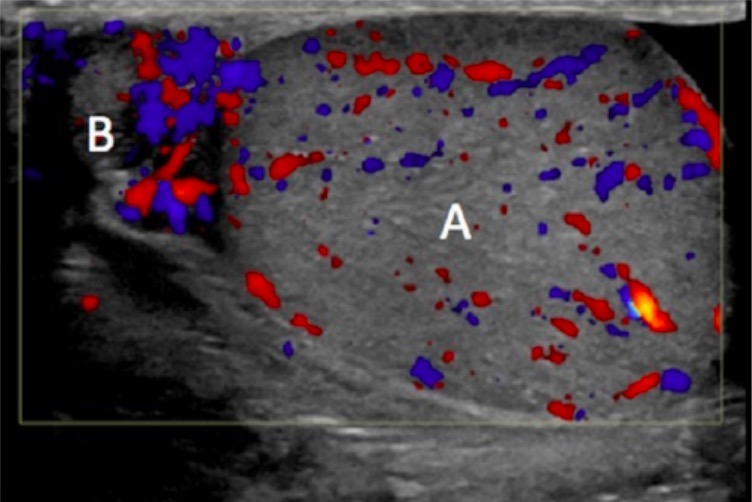
00:01 We're also gonna talk about epididymitis. 00:03 Now epididymitis is kind of like the PID of a male patient. 00:07 So this is, we'll call it I guess ascending infection, eventhough it’s kind of going down and it’s the most common intrascrotal infection. 00:15 It's most common in men, 18 to 35 years old and it's rare in a pre-pubertal population. 00:22 But it also can effect any age, so we know especially in the United States that elderly patients are sexually active more and more now a days, so this is something that can happen in any age group. 00:33 So what is the epididymis? The epididymisis a tightly coiled structure along the posterior aspect of the testicle. 00:42 It’s the place where the sperm mature prior to transfer into the vas deferens. 00:47 So epididymitis develops when the bacteria travel retrograde down the vas deferens. 00:52 So they're basically kind of going backwards into the testicle. 00:55 Orchitis which is an infection of the testicle itself may occur as well when you have epididymitis. 01:02 That's a condition known as epididymo-orchitis. 01:05 So those are somethings that go hand-in-hand sometimes. 01:09 Now, most commonly epididymitis is related to sexually transmitted pathogens, so it's related to chlamydia and gonorrhea. 01:17 Now in medicine, we have this kind of non-specific age cut off or it’s a specific age cut off of 35 years old, so patients who are less than 35 years of age historically, have been more associated with chlamydia and gonorrhea. 01:33 Whereas, as patients get older than 35 years of age, it’s thought that epididymitis maybe more related to bacteria related to urinary tract infection so like E. coli would be a common one. 01:46 Enteric pathogens, you also wanna consider for patients who have insertive anal intercourse. 01:52 Now, it’s important to remember that patients don't always follow the rules. 01:57 So if you're taking care of a patient who is 50 years of age and has engaged in a lot of promiscuous sexual activity, you wanna be thinking about a sexually transmitted pathogen as a cause for that patient's symptoms. 02:10 Whereas, if you have a younger person who potentially hasn't engage in anything along those lines and is not worried that they may have an STD, for those patients, you might wanna be thinking more that this is related to a urinary bug. 02:23 The key things for history you wanna get here, is you wanna take a sexual history. 02:29 You wanna find out if patients are using barrier protection, if they have a partner who has a known history, or a recent diagnosis of gonorrhea or chlamydia. 02:38 You wanna ask if they're having any urinary symptoms. 02:41 Are they having burning when they urinate? Are they having any discharge from their penis? They may have pain and swelling of the testicle, well, in order to diagnose epididymitis, you'll have pain and swelling of the testicle, unilateral pain, unilateral swelling. 02:55 It’s generally of gradual onset, the big thing that we're trying to differentiate epididymitis from is testicular torsion. 03:03 So testicular torsion will be discussed in another lecture. 03:06 But what that is, is that twisting of the testicle on its blood supply causing the testicle to develop ischemia. 03:13 Now, both of this present with pain and swelling of the testicle. 03:18 So we wanna try and differentiate these two conditions when we are caring for patients with pain and swelling of the testicle in the ED. 03:25 Fever is actually pretty rare in epididymitis and it's rare that patients would have severe systemic infections related to it. 03:33 On the physical exam, you wanna check a cremasteric reflex. 03:39 We'll talk more about that in the testicular torsion lecture but in patients who have epididymitis, the cremasteric reflex will be intact. 03:46 So the patient will have elevation of the testicle when you perform this. 03:51 The testis will also be in a normal anatomic position and torsion, they may not be in the normal anatomic position. 03:59 So you wanna definitely consider that when you’re thinking about whether this is epididymitis or whether its torsion. 04:06 And then lastly, we can think about Prehn's sign. 04:09 Prehn's sign is decreased pain with elevation of the testicle. 04:13 So if you lift it up, it hurts less. 04:15 Now, this is a pretty low sensitivity and specificity, but if it's present, it supports the diagnosis of epididymitis. 04:22 Our differential diagnosis here, so UTI is on there, definitely testicular torsion, so in thinking about the differential of consequence. 04:33 So what are the most worrisome things that could be going on, torsion is definitely very high up on that differential of consequence. 04:41 So distinguishing torsion from epididymitis. 04:44 Prostatitis as well as orchitis also on the differential here. 04:48 So how do we diagnose it? You can get a urinalysis. A urinalysis may show pyuria or white blood cells present. 04:58 You wanna do the STD testing that was referred to earlier in these lectures. 05:02 You wanna send-off urine testing for gonorrhea and chlamydia, or urethral swab for those. 05:08 And then you wanna get an ultrasound of the scrotum. 05:10 The ultrasound of the scrotum will show increase blood flow and inflammation of epididymis. 05:15 So here in this picture, that white box is basically demonstrating that the epididymis is inflamed and there's increase blood flow to that area. 05:25 You know if you suspect that this is sexually acquired that it's related to an STD, you wanna treat very similar to how you treat pelvic inflammatory disease with Ceftriaxone and Doxycycline. 05:37 If you suspect that it's more likely related to an enteric pathogen, a Fluoroquinolone is oftentimes the medication of choice. 05:45 A majority of these patients can go home and be treated as outpatients with Urology follow up. 05:53 But if someone has systemic signs of infections, if they have a fever, if they're vomiting, if they're generally not feeling well, they may need to be admitted for IV antibiotics. 06:02 So in conclusion here, chlamydia and gonorrhea are common causes of urethritis and cervicitis. 06:09 And the presentation of these conditions is very similar, so patients will present with vaginal discharge, urethral discharge, and co-infection, so both of these occurring at the same time, is actually quite common. 06:22 You wanna treat symptomatic patients presumptively for both gonorrhea and chlamydia prior to culture data returning. 06:29 Definitely after having a discussion with your patient about the risks and benefits of each option. 06:33 Pelvic inflammatory disease is an infection involving the upper female GU tract and has significant complications. 06:41 And have a very low threshold for treating PID for patients with concerning symptoms and examination findings. 06:47 The other thing that I wanna make sure that I bring up, is that you wanna make sure that the patient speaks with their partner and gets the partner tested as well and possibly treated. 06:56 Because otherwise, these people are gonna keep basically exchanging infection with one another.
About the Lecture
The lecture Epididymitis (Emergency Medicine) by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies. It contains the following chapters:
- Epididymitis
- Epididymitis Examination
- Epididymitis Management
Included Quiz Questions
What is the most common intrascrotal infection?
- Epididymitis
- Scrotal abscess
- Orchitis
- Testicular abscess
- Fournier gangrene
What is Prehn's sign?
- Decreased pain with elevation of the testicle
- Unilateral swelling of the scrotum
- Darkening of the scrotal sac
- Voluntary elevation of the scrotal sac
- Abnormally-looking scrotal sac
If an enteric pathogen is suspected to be the causative agent of epidydimitis, which antibiotic class is recommended?
- Fluoroquinolone
- Cephalosporins
- Penicillins
- Macrolides
- Sulfonamides
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |