Playlist
Show Playlist
Hide Playlist
Cerebral Edema
-
Emergency Medicine Head Injury.pdf
-
Download Lecture Overview
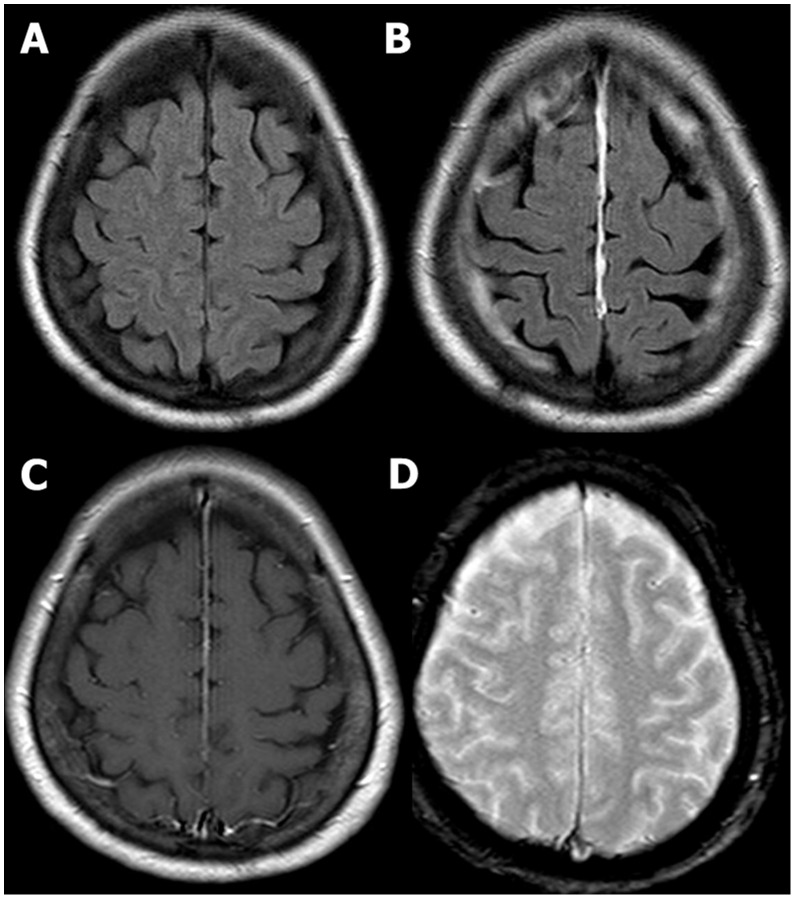
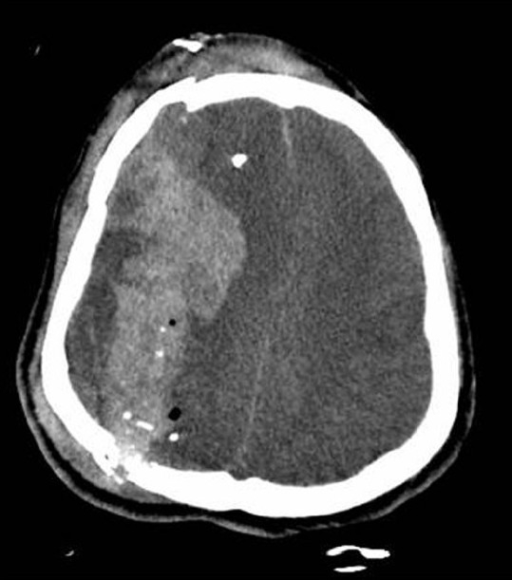
00:01 Alright, the last entity we’re gonna talk about is cerebral edema or elevated intracranial pressure. 00:07 This can be a little bit subtle to pick up on neuroimaging which is why I’ve compared a normal to an abnormal image here. 00:14 So you can see that on the image showing cerebral edema, you’re not actually able to see the sulci within the brain at all. 00:24 Whereas, you can see them clearly on the normal CT on the other side. 00:28 On the normal CT as well, you can also see clear differentiation between the grey matter and the white matter. 00:34 So the grey matter appears a lighter shade, the white matter appears a darker shade, and they’re pretty well demarcated between the two. 00:40 Whereas the edematous CT just shows uniform grey haze throughout the entire brain. 00:45 You also can see the ventricles a little bit on the normal CT, whereas they’re completely effaced on the CT with cerebral edema. 00:54 So the CSF space is that normally should be open and patent, are actually compressed in the patient who has cerebral edema. 01:02 So let’s go back to our patient. 01:04 So he’s had a CT scan and while we’re waiting for the results, we re-examine him and we find his GCS is now down to six. 01:13 So his eyes are still closed, he’s no longer making any noise, and he’s still withdrawing to pain but much more weakly. 01:20 We look at his vital signs and we’ve actually stabilized him hemodynamically. 01:24 He’s done quite well with his fluids and his pelvic binder. 01:27 He’s oxygenating well. 01:29 So really, we don’t have a systemic explanation for the worsening of his GCS. 01:35 So we need to be concerned that he’s got neurologic deterioration. 01:40 So we get his CT back and this is what we find. 01:43 You can see he’s got a large subdural hematoma, so it’s crescent shaped. 01:48 He’s got completely effacement of the ventricle on the affected side, He’s got midline shift over to the contralateral side, so this is a pretty bad CT scan, and it’s not surprising that his neurologic status is deteriorating. 02:03 So what do we wanna do now that we have this information? Well, again, if his ABC’s hadn’t already been stabilized, we would wanna be sure to do that first and foremost. 02:14 We wanna make sure that we keep very close tabs on his neurologic status which is why we were doing a repeat GCS check on him. 02:22 We’ve already obtained early imaging but now that we know that his imaging is abnormal, we wanna get our neurosurgical colleagues on board right away, and while we’re waiting for them to come and help us with definitive management, we wanna make sure that we are optimizing him medically. 02:38 So we wanna treat any physiologic stressors. 02:40 Things like agitation, posturing, vomiting, seizure, these are all things that actually, one, take a lot of metabolic energy which this patient can’t afford to expend right now. 02:52 And two, they actually raise the intracranial pressure. 02:54 So we wanna make sure that we are keeping our patient as stress free and calm as we possibly can. 03:01 We also wanna medically manage the intracranial pressure. 03:04 We can see that this patient has a large bleed with a lot of mass effect and there’s every reason to believe that his ICP is elevated, so we wanna bring that down. 03:13 We also wanna stop any bleeding that’s ongoing, so we don’t want this bleed to get bigger. 03:18 We wanna make sure that we stop it in its tracks before it expands further. 03:22 And we wanna regulate the blood pressure because elevated blood pressure can increase bleeding but however, blood pressure that’s too low can impair cerebral perfusion. 03:33 So we wanna make sure that we’re hitting the right spot in terms of management of his pressure. 03:37 So let’s talk for a minute about intracranial pressure management. 03:41 So the basic physiology behind intracranial pressure was described by Munro and Kellie, and basically, what they said is that the cranium is a fixed volume space. 03:50 That makes sense, right? The skull doesn’t expand. It doesn’t contract. 03:53 It’s just basically a bucket that holds one volume. 03:56 There are three things inside of our bucket. 03:59 There’s brain, there’s blood, and there’s cerebrospinal fluid. 04:03 If the volume of any of these three components increases for any reason, then the intracranial pressure is gonna go up accordingly because the bucket can’t hold any more volume. 04:16 So if you cram more volume in, you’re gonna raise pressure. 04:20 The only way you can lower the pressure is to decrease the volume of one of these three components and this is the physiologic basis for ICP lowering no matter how you go about doing it. 04:32 So you should be worried about elevated intracranial pressure whenever your patient who has a head injury is going into a deepening coma, so their GCS score is decreasing. 04:46 If they’re showing lateralizing signs such as gaze deviation or a blown pupil, you wanna be concerned that they have impending brain herniation, and basically, any sign of neurologic deterioration, you wanna consider the possibility of intracranial pressure elevation and address it accordingly. 05:04 Now, the important thing to remember about intracranial pressure management is that usually, we’re doing it as a bridge to more definitive management. 05:12 So remember, our patient has a big subdural hematoma. 05:15 He’s gonna need surgical evacuation of that hematoma, so we’re gonna lower his intracranial pressure to prevent him from having bad neurologic outcomes, pending his surgery. 05:27 However, there are situations where intracranial pressure management might be the only treatment option. 05:33 For example, in traumatic subarachnoid hemorrhage, there’s not really any surgical intervention that we can perform, so maintaining the patient at the best possible intracranial pressure might be the only thing we can do to optimize their neurologic outcome.
About the Lecture
The lecture Cerebral Edema by Julianna Jung, MD, FACEP is from the course Trauma (Emergency Medicine).
Included Quiz Questions
Which of the following statements about the Monro-Kellie hypothesis is INCORRECT?
- The cranium adjusts its volume according to the volume of its contents.
- The cranium contains the brain, blood, and cerebrospinal fluid.
- An increase of any one of the contents of the cranium will increase intracranial pressure.
- The only way to decrease the intracranial pressure is to decrease the volume of any one of the three contents.
- All interventions to decrease intracranial pressure are based on the Monro-Kellie hypothesis.
Which of the following statements regarding cerebral edema is INCORRECT?
- Cerebral edema will always be evident in neuroimaging.
- There may be sulci effacement in cerebral edema.
- The ventricles may be compressed in patients with cerebral edema.
- There may be a loss of gray-white differentiation in cerebral edema.
- Cerebral edema may result from increased intracranial pressure.
Which of the following statements regarding the management of intracranial pressure (ICP) is INCORRECT?
- ICP control is the definitive management for all intracranial hemorrhage.
- Subarachnoid hemorrhage is managed by control of ICP.
- Gaze deviation in a patient with increased ICP may indicate an impending herniation.
- A patient with a deepening coma may be having an increase in intracranial pressure.
- ICP control may be done prior to surgical evacuation of hematoma to prevent neurologic decline.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |