Playlist
Show Playlist
Hide Playlist
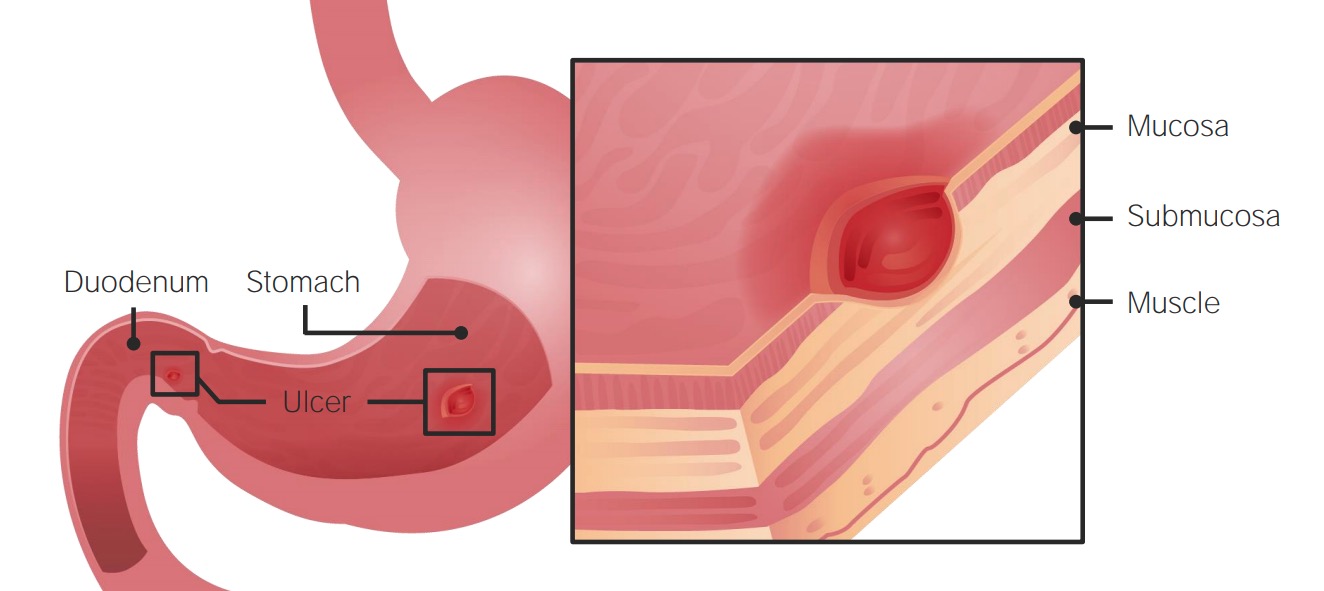
Stomach Ulcer (Peptic Acid Disease) Medication
-
Slides Gastrointestinal Drugs.pdf
-
Slides Gastrointestinal Drugs.pdf
-
Download Lecture Overview
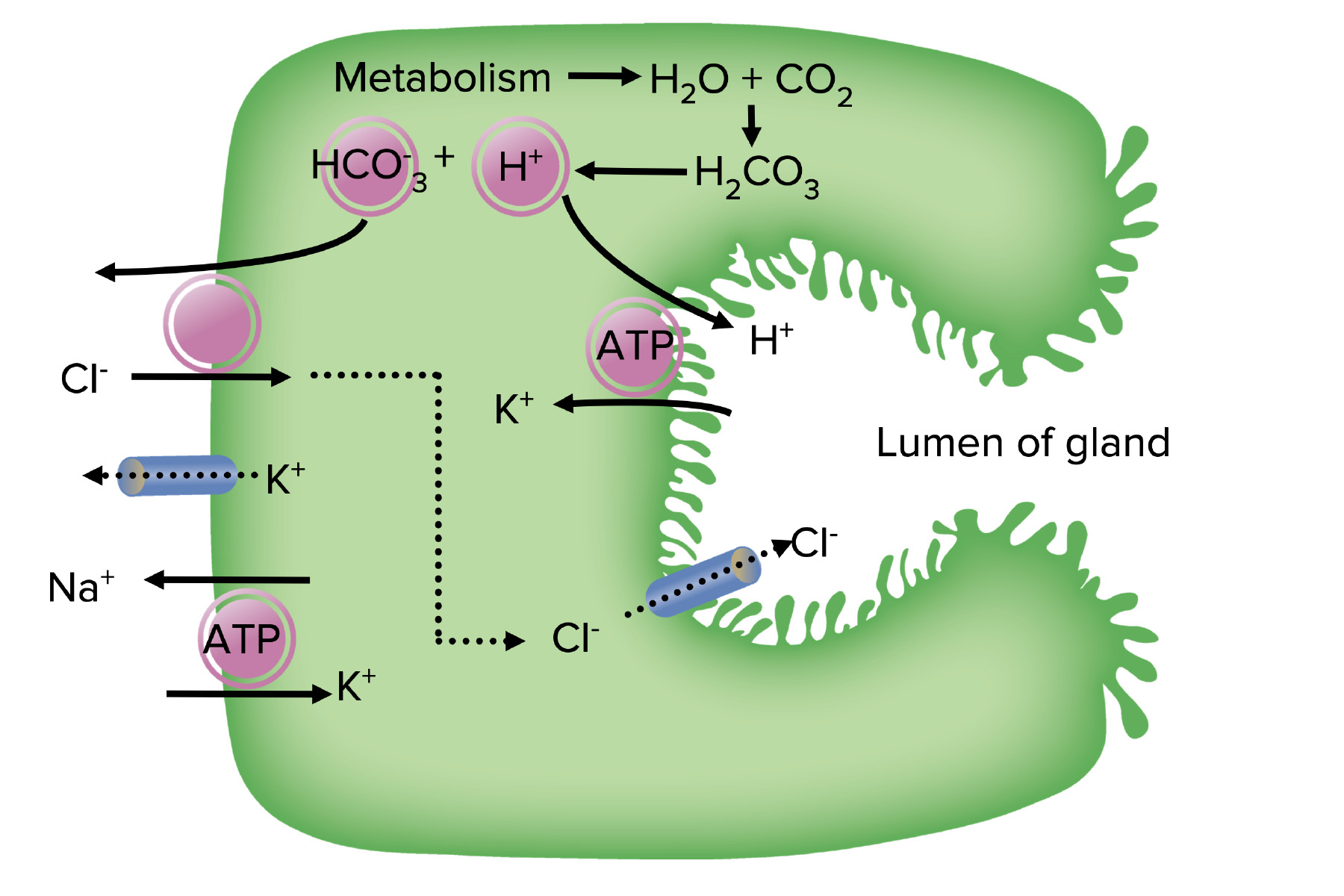
00:01 Welcome to Pharmacology by Lecturio. 00:04 I'm Dr. Pravin Shukle. 00:05 We're going to be covering GI pharmacology today. 00:10 The drugs used for gastrointestinal order spend a huge range of medications. 00:15 We have drugs for peptic acid disease, drugs for pro-motility, drugs for irritable bowel disease, drugs for inflammatory bowel disease, and anti-emetics. 00:27 We have a whole host of other agents as well for various ailments. 00:32 Let's look at peptic acid disease. 00:35 We have the antacids, the H2 blockers, the PPIs, the mucosal protective agents, and the antibiotics. 00:45 Let's start off with the antacids. 00:48 Now, antacids are weak bases that neutralize the low pH environment of the stomach. 00:53 These can include many agents such as magnesium hydroxide which is better known as Milk of Magnesia. 00:59 Milk of Magnesia is a mainstay of antacid therapy and it's probably the first line agent that we use in most cases. 01:07 It has a strong laxative effects so it's very good for patients who are also constipated. 01:12 Another agent that we use is aluminum hydroxide, commonly known as Maalox. 01:17 It has a strong constipating effects so it's better for people who have diarrhoea. 01:22 And calcium carbonate and sodium bicarbonate are just plain antacids. 01:27 They are absorbed by the gut unlike the other agents. 01:31 The first two agents that I mentioned tend to stay in the gut, these agents are actually get absorbed. 01:36 Let's move on to the H2 receptor antagonists. 01:40 These agents block histamine at the H2 receptor inside the gastric mucosa, specifically the parietal cells. 01:48 You can see that they inhibit stomach acid production directly, especially at night, so this is a particularly good agent for people who have night time GERD symptoms. 01:59 They are relatively nontoxic agents, they are actually sold over the counter now, we don’t even prescribe them. 02:06 Cimetidine was the original and prototypical drug in this drug class. 02:11 But we actually don't use it because there are multitude of drug interactions that we get from this particular medication. 02:17 Interestingly enough, some of these agents, in particular cimetidine, do have an antiandrogen effect as well at high doses. 02:26 These are the agents that are commonly sold. 02:28 These agents are sold over the counter, they’re extensively used all around the world. 02:34 Let's move on to the PPIs or the proton pump inhibitors. 02:38 These are lipophilic weak bases. 02:39 So the agents themselves are not antacids. 02:44 What they do is they become protonated, and they work inside the parietal cells and they get concentrated in these areas up to 1,000 times. 02:53 They irreversibly inactivate the hydrogen-potassium-ATPase pump. 02:59 What this does is that it ends up causing less acid secretion, substantially less. 03:04 Now they are rapidly metabolized. 03:06 They may take 3 to 4 days to actually have an effect because of this reason. 03:11 They are far more effective than the H2 antagonists that I spoke about earlier but they last, and they work well, and they are the mainstay of anti-ulcer therapy. 03:23 There are some toxicity issues associated with the PPIs. 03:26 You can get diarrhoea, abdominal pain and headache. 03:30 And you can get hypergastrinemia if you use them for a long time. 03:36 They may also decrease the ability of drugs that require higher acid levels. 03:40 So for example, ketoconazole requires a high acid environment within the stomach to become particularly activated and absorbed, if you give a PPI the same time as you give ketoconazole, you're going to reduce the availability of ketoconazole to the body for it to do its job. 03:56 The same thing will happen with drugs like digoxin. 04:00 Now, a small increase in respiratory and enteric infections are associated with PPI use. 04:06 We have many brands out on the market today, prototypical drug is omeprazole, but you have a whole list of other ones that I've given you here. 04:15 Let's move on to the mucosal protective agents. 04:18 Now the prototypical example of this is sucralfate. 04:21 It's a very poorly soluble molecule. 04:24 It polymerizes inside the stomach. 04:26 And when I say polymerize what I mean is is that it forms chains of molecules. 04:31 This polymer will bind to the injured tissue inside the patient stomach. 04:36 And it forms a protective coating over those ulcers and prevents further damage from occuring. 04:43 The down side of this medication is it has to be taken 4 times a day. 04:47 And that's really the main reason why we don't use it as much as we used to, simply because of the inconvenience. 04:53 It's a very low toxicity agent. 04:55 It has a very low solubility. 04:57 It's quite effective, unfortunately it's inconvenient. 05:01 These medications are great for patients who are very adherent to their schedule and so if you know these patients are going to follow their instructions, it's a great choice. 05:14 Let's move on to other agents. 05:15 Misoprostol is an analogue of prostaglandin E. 05:19 It works at almost the same point in the system as the PPIs. 05:24 You get increased mucosal protection because it directly inhibits acid secretion. 05:29 And it reduces ulcers in NSAID users as well. 05:33 The adverse event rate is quite high because it's poorly tolerated. 05:38 There's lots of GI upset and diarrhoea associated with this agent. 05:42 And for this particular reason, it's not used much anymore. 05:45 It is an agent however that you should be aware of because it is going to be on pharmacology portion of your exam. 05:54 Let's move on to agents like colloidal bismuth. 05:57 So, bismuth subsalicylate, also called Pepto-Bismol, gives a protecting coating on ulcerated tissue much like sucralfate. 06:07 It stimulates mucosal protective systems as well, so it goes a little bit further than sucralfate in that sense. 06:13 It actually has direct antimicrobial effects. 06:17 And you actually have some sequestration of enterotoxins. 06:21 So if there are toxins within the gut, it actually binds those toxins and renders them biologically unavailable. 06:29 It reduces stool frequency in infectious diarrhoea. 06:33 And unfortunately, there is a cosmetic side effect of this medication, it causes a black tongue. 06:40 Now the other important issue that you have to remember is it also causes black stools. 06:44 And many times, people who have melena type stools from Pepto-Bismol are misdiagnosed as having GI bleeds. 06:52 That is not the case. 06:53 So be aware that if you have a patient who presents with melena type stools ask first if they were taking this agent.
About the Lecture
The lecture Stomach Ulcer (Peptic Acid Disease) Medication by Pravin Shukle, MD is from the course Gastrointestinal Pharmacology.
Included Quiz Questions
Which option CORRECTLY pairs the medication with its side effect?
- Magnesium hydroxide --- laxative effect | Aluminum hydroxide --- constipating effect
- Magnesium hydroxide --- constipating effect | Aluminum hydroxide --- absorbed by the gut
- Magnesium hydroxide --- constipating effect | Aluminum hydroxide --- laxative effect
- Magnesium hydroxide --- laxative effect | Aluminum hydroxide --- absorbed by the gut
- Magnesium hydroxide --- laxative effect | Aluminum hydroxide --- causes nausea
What is the mechanism of action of famotidine?
- Blocks histamine receptor type 2 in parietal cells
- Blocks histamine receptor type 2 in the chief cells
- Blocks histamine receptor type 1 in the surface mucous cells
- Blocks hydrochloric acid production by the G cells
- Blocks hydrochloric acid production by the gastric glands
What best describes the process by which omeprazole enters the parietal cell?
- Omeprazole enters the parietal cell with a neutral charge and becomes protonated.
- Omeprazole enters the parietal cell with a neutral charge and becomes polymerized.
- Omeprazole enters the parietal cell with a neutral charge and becomes hydroxylated.
- Omeprazole enters the parietal cell with a neutral charge and becomes hydrolyzed.
- Omeprazole enters the parietal cell with a positive charge and becomes activated when it binds with magnesium ions.
What is a side effect of omeprazole?
- Small increased risk of respiratory or enteric infections
- Paresthesias
- Increased risk of developing hirsutism
- Increased risk of anxiety
- Increased risk of developing dermatitis nigricans
What is the mechanism of action of misoprostol?
- Misoprostol is a prostaglandin E1 analog that increases gastric mucus production.
- Misoprostol is a prostaglandin E3 analog that increases gastric acid production.
- Misoprostol is a prostaglandin E2 analog that reduces gastric mucus production.
- Misoprostol is a neuraminidase analog that increases gastric antibody production.
- Misoprostol is a ghrelin analog that increases gastric acid production and reduces gastric mucus production.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Simple and straightforward and short and sweet which is good.